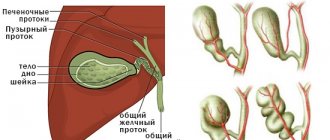
Primary biliary cirrhosis is a destructive and inflammatory liver disease characterized by a chronic course. It is accompanied by damage to the intrahepatic ducts. As such cirrhosis progresses, ductopenia (disappearing bile duct syndrome) and persistent cholestasis (decreased bile flow into the duodenum due to disturbances in its production, excretion and/or excretion) may develop. In the terminal stage of the disease, liver failure is usually observed.
1.What is primary biliary cirrhosis and its causes?
Primary biliary cirrhosis
is cirrhosis of the liver caused by damage to the bile ducts. Like many other liver diseases, primary biliary cirrhosis continually attacks the liver, damaging it. As a result, healthy liver tissue is replaced by scar tissue (fibrosis). And as more scar tissue forms, the structure and function of the liver suffers.
The exact causes of biliary cirrhosis are not known. But there is an opinion that this disease may be associated with a problem with the immune system - the body's natural defense system.
A must read! Help with treatment and hospitalization!
general description
Biliary cirrhosis is
a chronic autoimmune disease that occurs as a result of a violation of the outflow of bile through the intrahepatic and biliary tract (cholestasis) and is characterized by the replacement of parenchymal liver tissue with connective tissue (fibrosis). The prognosis of the disease itself depends on diagnosis and in undiagnosed cases leads to deterioration of development: progressive destruction of the parenchyma with the formation of foci of fibrosis, which results in liver cirrhosis and liver failure.
According to statistics, in economically developed countries, biliary cirrhosis is diagnosed in people aged 30 to 55 years, more often in men. The ratio of incidence among men to women is approximately 3 to 1.
2. Symptoms of the disease
Many people with primary biliary cirrhosis have no symptoms at all. But if they are, signs of the disease may be:
- Itching;
- Fatigue;
- Yellowing of the skin and whites of the eyes (jaundice);
- Discomfort in the upper right part of the abdomen;
- Dry eyes and dry mouth;
- Vaginal dryness in women.
With more severe liver damage, complications of cirrhosis may occur, such as:
- Fluid accumulation in the abdominal cavity (ascites);
- Bleeding from dilated veins of the esophagus, stomach and rectum (bleeding from varicose veins);
- Premature thinning of bones (osteoporosis).
Visit our Hepatology page
Forecast
Life expectancy for asymptomatic PBC is on average 17-20 years. In patients with severe intrahepatic symptoms, the prognosis of the disease is much worse - no more than 7 years. Increasing signs of hepatic cell failure and portal hypertension entail side diseases - ascites, encephalopathy, hepatic coma, scleroderma, “spontaneous” peritonitis, etc. The course of the disease is aggravated by hemorrhagic syndrome, in which life expectancy, as a rule, does not exceed 2 years.
The prognosis of secondary biliary cirrhosis worsens if it is not possible to eliminate the obstruction of the biliary tract even surgically. The accumulation of bile in the body leads to serious complications - portal vein thrombosis, intestinal bleeding, liver cancer, abdominal dropsy, etc. Life expectancy with ascites is on average 2-3 years, and with a cancer complication - no more than 3-6 months.
3.Diagnosis of the disease
A doctor may suspect primary biliary cirrhosis based on a medical history, a physical examination of the patient, and laboratory tests that show high levels of the enzyme alkaline phosphatase and antimitochondrial antibodies in the blood. If necessary, your doctor may order an ultrasound, which can show images of the liver and other tissues inside the body. A biopsy - taking a tissue sample from the liver and further examining it under a microscope - is the best way to definitively make a diagnosis.
About our clinic Chistye Prudy metro station Medintercom page!
Review of drugs
Drug therapy only stops pathological processes in the digestive gland and does not lead to recovery. With the help of hepatoprotectors, antibiotics, diuretics and other medications, it is possible to reduce the severity of symptoms and thereby alleviate the patient’s condition. Biliary cirrhosis can be treated with the following drugs:
- cytostatics (“Aminosol”, “Decapeptyl”) - antitumor medications that prevent the formation of malignant tumors;
- choleretic drugs (“Nicodin”, “Hologon”) - increase the concentration of acids in bile and stimulate its production in the digestive gland;
antioxidants (“Essentiale”, “Complivit Selenium”) - neutralize harmful substances and free radicals in the body;- hepatoprotectors (“Heptral”, “Karsil”) - protect hepatocytes from the negative effects of toxins, antibodies and other substances;
- diuretics (“Spironol”, “Aldactone”) - promote the excretion of salts and toxic substances in the urine;
- anti-inflammatory drugs (“Essliver Forte”, “Kuprenil”) - reduce inflammation in the parenchyma, thereby slowing down the process of death of hepatocytes.
Irrational use of diuretics can lead to impaired renal function and the development of encephalopathy.
4. Treatment of primary beliary cirrhosis
Primary biliary cirrhosis is difficult to cure because the disease is associated with problems in the body's immune system. As with other forms of cirrhosis, treatment primarily focuses on relieving symptoms of the disease, preventing and treating complications, and preventing other health problems that can further damage the liver.
One of the drugs that can be prescribed to patients after a diagnosis of primary biliary cirrhosis is Ursodiol
. It helps bile move from the liver to the small intestine. If treatment is started early enough, ursodiol may improve liver function and may even help avoid liver transplantation.
Other medications prescribed by your doctor will help relieve the itching. Since primary biliary cirrhosis can cause dry eyes and mouth, eye drops (artificial tears) are used to combat these symptoms. Regular chewing gum or lozenges help with dry mouth - they will help increase salivation. If they do not help, there are special medications that will help cope with the problem.
Because people with primary biliary cirrhosis have an increased risk of developing osteoporosis
, they need to have bone mineral density scans periodically. In addition, your doctor may recommend calcium and vitamin D supplements or medications.
Liver transplantation
– a method of treating patients with the last stage of primary biliary cirrhosis. But the peculiarity of the disease is that the problem in the immune system cannot be treated, which means that cirrhosis can recur again even after a liver transplant.
Publications in the media
PRIMARY BILIARY CIRRHOSIS
- chronic non-purulent destructive cholangitis of small and medium-sized intrahepatic bile ducts, leading to their destruction and the development of liver cirrhosis.
Frequency • The disease is observed everywhere, the prevalence varies in different countries (in Europe - from 2 to 24 cases per 100,000 population) • Women make up up to 75–90% of cases • The predominant age is 35–60 years.
Genetic aspects . Occurs as a result of deficiency of dihydrolipoamide acetyltransferase (109720, [EC 2.3.1.12, B]).
Etiology and pathogenesis are not fully understood • Impaired immunoregulation with loss of immune tolerance to tissues (bile ducts) • High titer of autoantibodies in the blood serum, primarily antimitochondrial autoantibodies • Destruction of small and medium-sized intrahepatic bile ducts leads to the development of cholestasis, regeneration of damaged bile ducts ducts are defective • Toxic components that are usually excreted into bile (bile acids, copper, etc.) are retained in the liver and cause secondary damage to hepatocytes.
Pathomorphology • Destruction of the bile ducts • Lymphomonocytic inflammatory infiltration around the damaged ducts, formation of granulomas • Proliferation of the bile ducts • Fibrosis in the portal zone and beyond • Biliary cirrhosis.
Clinical manifestations • Possible asymptomatic course until the death of the patient • The disease begins with skin itching, usually without jaundice • Jaundice develops 6–24 months after the onset of itching • Pain in the right upper quadrant of the abdomen, which may subsequently disappear • Enlarged liver • Increased fatigue • Skin hyperpigmentation is possible • In the later stages of the disease, osteoporosis, xanthomas, duodenal ulcers, signs of liver cirrhosis and its complications (bleeding from esophageal varices) are observed.
Laboratory tests • Significant increase in the activity of alkaline phosphatase and g-glutamyl transpetidase in the blood serum • Not a constant increase in the concentration of cholesterol in the blood serum, the concentration of direct bilirubin at the onset of the disease does not exceed 35 µmol/l • Increase in the concentration of IgM in the blood serum • Titer of antimitochondrial autoantibodies 1: 40 or more.
Instrumental studies • Liver biopsy • In atypical cases (disease in a man, absence of antimitochondrial autoantibodies, severe abdominal pain, uninformative liver biopsy), the bile ducts are examined using endoscopic or percutaneous cholangiography.
Differential diagnosis • Primary sclerosing cholangitis • Cholestatic variant of sarcoidosis • Autoimmune cholangiopathy • Cholestatic reaction to drugs.
Concomitant diseases • A combination of primary biliary cirrhosis with almost all autoimmune diseases has been described • Often combined with rheumatoid arthritis, scleroderma, CREST syndrome, Sjogren's syndrome, autoimmune thyroiditis, etc. • The risk of developing breast cancer in patients is 4.4 times higher than in the general population.
Treatment • Symptomatic treatment of cholestasis (see Primary sclerosing cholangitis) • Taking ursodeoxycholic acid 13–15 mg/kg 2 times a day significantly, although to a small extent, increases the life expectancy of patients and allows delaying liver transplantation • The effectiveness of GCs, cytostatics, colchicine is minimal, and given this, as well as severe side effects, it is not recommended to prescribe these drugs • Since there is a threat of bleeding from varices of the esophagus even before the development of cirrhosis, it is necessary to promptly consider the issue of portacaval shunting, which in patients with primary biliary cirrhosis has positive effect • It is not recommended to remove gallstones if they are not located in the common bile duct, because patients do not tolerate surgery well • Liver transplantation is more successful if it is performed in the early stages of the disease •• Patients should be referred to a transplant center when the serum bilirubin concentration is 150 µmol/l •• Five-year survival rate is 60–70% •• After transplantation, the disease may recur.
Complications and their treatment • Osteoporosis • Varicose veins of the esophagus develop in a third of patients on average after 5.6 years, half subsequently experience bleeding • Other complications of liver cirrhosis • Infectious complications (sepsis).
Course and prognosis • The course is unpredictable • Life expectancy with asymptomatic course is about 10 years, with symptoms - about 7 years • Adverse prognostic factors in the presence of clinical manifestations - old age, hepatosplenomegaly, ascites, constant increase in bilirubin concentration more than 100 µmol/l ( life expectancy is no more than 2 years), the concentration of albumin in the blood serum is less than 30 g/l.
SECONDARY BILIARY CIRRHOSIS develops with long-term disruption of the outflow of bile (cholestasis) due to a pathological process in any area from the hepatocyte to the common bile duct.
Etiology • Mechanical obstruction of the bile ducts (usually extrahepatic) •• Stones of the common bile duct •• Cancer of the pancreas and papilla of Vater •• Benign strictures of the ducts •• Infections of the bile ducts •• Cholangiocarcinoma growing into the main intrahepatic ducts • Drug-induced hepatitis, cholestatic variant of the viral , alcoholic hepatitis • Taking oral contraceptives • Bile duct atresia • Sepsis • Byler family disease • Lymphogranulomatosis • Benign recurrent cholestasis • Amyloidosis
Pathomorphology • The liver is enlarged, green in color • Proliferation of the bile ducts • Ruptures of the interlobular bile ducts with the formation of “bile lakes” • Accumulation of copper in hepatocytes (in a non-toxic form) • Fibrosis is first periportal, then septa are formed and nodular regeneration of hepatocytes develops (biliary cirrhosis of the liver) .
Clinical picture • Skin itching • Jaundice • Malabsorption in the intestines, steatorrhea • Hypovitaminosis A, E, D, K • The liver is enlarged, hardened, painless • Splenomegaly at the stage of cirrhosis • Osteodystrophy (osteoporosis and osteomalacia) •• Bone pain •• Fractures with minimal trauma • Xanthomas, xanthelasmas, skin pigmentation • Feces are discolored, urine is dark.
Laboratory tests • Increased serum concentrations of direct bilirubin, alkaline phosphatase, cholesterol (not constant), lipoproteins • Direct bilirubin in the urine.
Instrumental studies • Ultrasound can detect dilation of the extrahepatic bile ducts, in this case, endoscopic retrograde or percutaneous transhepatic cholangiography is then performed; if there are no ductal lesions, a liver biopsy is necessary • If the extrahepatic ducts are not dilated on ultrasound, a liver biopsy is performed; If biopsy reveals changes in large ducts, cholangiography must be performed.
Treatment is aimed at eliminating the cause of cholestasis • Symptomatic treatment of cholestasis (see Primary sclerosing cholangitis) • Indications for surgical intervention (removal of stones, tumors, drainage of the biliary tract, anastomosis) are determined by the cause of obstruction and the patient’s condition.
Synonyms • Hypertrophic cirrhosis Ano • Cholangiolytic cirrhosis
ICD-10 • K74.3 Primary biliary cirrhosis • K74.4 Secondary biliary cirrhosis •• K74.5 Biliary cirrhosis, unspecified
Diagnostics
NEARMEDIC clinics perform thorough diagnostics. The disease is detected in the early stages, when the disease can be brought under control, tissue can be restored, and progression can be interrupted. The initial appointment is carried out by an experienced gastroenterologist. The doctor establishes the clinical picture.
What tests are taken:
- general blood test (detects an increased content of leukocytes, a decrease in hemoglobin, platelets);
- biochemical blood test shows alkaline phosphatase, increased levels of bilirubin, ALT, AST, decreased albumin, high levels of potassium, urea, sodium, creatinine.
Hardware diagnostics and treatment
In NEARMEDIC clinics, modern ultrasound examination devices allow you to assess the condition of the organ: check the enlargement (accurately determine the size), see changes in the size of the spleen, evaluate the shape of the internal organs.
A computed tomography scan is performed to carefully examine the condition of the ducts, vessels, and tissues for damage. If a disease is suspected, Doppler measurements are performed to evaluate the blood vessels, and the doctor also recommends an MRI.
The most informative method is a biopsy: it best shows changes and the extent of organ damage. They will allow you to choose the most effective treatment method. Often, a diet, avoidance of harmful foods and drinks, and taking medications are sufficient for this.
Choose the clinic correctly so as not to pay too much for your health.
Diagnostics at the clinical hospital on Yauza
Diagnosis of cirrhosis includes a whole range of measures and begins with a survey and examination of the patient by an experienced gastroenterologist-hepatologist. Having suspected a patient of cirrhosis, our doctors send him for additional examination.
Laboratory diagnostics
The range of available laboratory tests includes all the necessary tests:
- general clinical blood and urine tests;
- a detailed biochemical blood test, especially important in diagnosing the functional state of the liver;
- serological studies and PCR diagnostics for viral hepatitis;
- blood clotting test;
- markers of thesaurismosis (storage diseases);
- markers of autoimmune liver diseases.
Additional tests are also prescribed to exclude concomitant pathologies of other organs and systems.
Instrumental examination
Ultrasound examination – ultrasound of the abdominal organs with triplex scanning of the vessels of the portal system at an expert level. Allows you to draw up a detailed picture of the state of the hepato-biliary system and other abdominal organs, assess portal blood flow, and identify signs of portal hypertension.
If necessary, the examination can be supplemented with:
- computed tomography (CT scan of the abdominal cavity);
- magnetic resonance imaging (MRI of the abdominal organs, MRI of the liver and pancreas, MR cholangiopancreatography);
- expert gastroscopy (FGDS);
- Endoultrasound is an endoscopic ultrasound examination that can detect formations of 1 mm in size in the upper parts of the digestive tract, including in the gallbladder and ducts, liver;
- fibroelastography – assessment of the severity of liver fibrosis;
- It is possible to perform a puncture biopsy.
The expert level of diagnosis of liver cirrhosis, its causes and severity is ensured by the high qualifications of our specialists and the advanced equipment of the Yauza Clinical Hospital, recognized as one of the best in Moscow. An in-depth examination allows you to accurately determine the stage of the disease and the nature of its course, and select treatment taking into account the individual characteristics of each individual patient.
Sign up for a consultation
In most cases, complications of the disease can be prevented if detected in the early stages. However, the disease is usually asymptomatic. Only regular preventive examinations can detect pathology in time. Sign up for an examination now to avoid problems in the future.
Differential diagnosis
It is carried out in the presence of non-cirrhotic causes of liver enlargement. The disease is differentiated from viral, drug and alcohol-type hepatitis. For this, immunology, PCR and hepatitis virus markers are used.
Differential diagnosis is necessary with:
- congenital pathologies (Wilson-Konovalov disease, hemochromatosis, alpha-1-antitrypsin deficiency);
- non-alcoholic fatty liver disease;
- metastases or malignant neoplasm of the liver;
- sclerosing cholangitis of the primary type;
- biliary cirrhosis (primary and secondary);
- autoimmune hepatitis;
- toxic effects of medications, heavy metals, etc.;
- narrowing of the bile ducts.
To make an accurate diagnosis, a consultation with a geneticist, cardiologist, ophthalmologist and psychiatrist is prescribed.
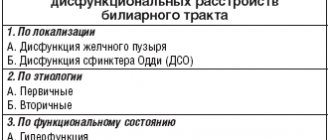
Classification of the disease
Biliary cirrhosis of the liver is assessed using the Child-Pugh scale, which implies an assessment of the functioning of the organ and:
- the presence of ascites and encephalopathy (one of the most common complications of liver diseases);
- bilirubin level;
- albumin concentration;
- prothrombin index, which indicates the presence of blood clotting disorders.
The difference between a healthy liver and a liver affected by cirrhosis
After studying all these indicators, points are given (from 0 to 10), then they are summed up and the class of biliary cirrhosis is determined. In total, there are 3 classes of this disease:
- A – it is characterized by minimal scores, the average life expectancy after surgery is 20 years;
- B – the number of points is average, after surgical interventions, life expectancy is on average 10 years, strip operations end in death in 30% of cases;
- C – high score, surgical interventions are rarely performed, abdominal operations end in death in 80% of cases.
There is also another classification of biliary cirrhosis of the liver - METAVIR, which is used to determine the degree of damage to the organ by fibrous tissue. This assessment is carried out through a biopsy. Gradation of degree - from 0 to 4.
Causes of the disease
The main causes of liver cirrhosis are systematic alcohol consumption, the presence of viral hepatitis B, C. The disease can also be triggered by uncontrolled medication use, metabolic pathology, and heredity.
The general condition of the blood vessels plays an important role. The reasons for its occurrence are different, but there are general statistical data: people over 45 years of age are more likely to get it. This is largely due to the deterioration of metabolic processes and individual lifestyle characteristics. Including diet, frequency of alcohol consumption. There are more cases of the disease among men than among women, and a higher percentage of those diagnosed with the alcoholic form of the disease. The occurrence of the disease in women cannot always be associated with any exact cause.
Modern treatment technologies and preventive measures help reduce mortality from the disease.
Reasons that can trigger the disease:
- daily/frequent drinking of alcohol (80 ml or more of ethyl alcohol – people get sick in more than 30% of cases);
- hepatitis: C, B,
- autoimmune disorders;
- enzyme deficiency;
- Wilson-Konovalov disease;
- Bud-Chiari syndrome;
- diabetes;
- operations on the gastrointestinal tract;
- obesity;
- parasitic infection of internal organs.
Diet
Diet plays an important role in the treatment of biliary cirrhosis. With the development of this disease, the functioning of not only the liver, but also other internal organs fails. And in order to reduce the burden on them and prevent the development of complications, all patients, without exception, need to follow certain rules in their diet. Depending on the severity of the disease and its accompanying complications, patients are assigned to treatment table No. 5a or No. 10 (mainly used when ascites occurs).
Violation of nutritional rules in biliary cirrhosis of the liver shortens the patient’s life
The daily calorie intake should not exceed 2900 kcal. In this case, it is imperative to refuse:
- fatty and fried foods;
- alcoholic drinks;
- dairy products;
- honey;
- fatty fish and meat;
- seafood;
- nuts
The main part of the diet should be fresh vegetables and fruits. You need to eat food in small quantities, but often - about 5-6 times a day. The last meal should be 2-3 hours before bedtime.
Food should be consumed boiled. Some dishes can be steamed. It is not advisable to bake food in the oven even without using oil and spices. In this case, food should be eaten warm. If liver function is impaired, hot and cold foods and drinks should not be consumed. Fasting days are held once every 2 weeks, during which the patient must eat only fresh vegetables and fruits.
Vegetables and fruits provide the body with vitamins and minerals, maintaining its functionality at the proper level.
An important point is compliance with the drinking regime. This allows you to avoid the occurrence of edema and complications in the form of disorders of the urinary system. Patients with biliary cirrhosis are recommended to drink at least 2 liters of purified water per day (this volume does not include teas and liquid dishes).
Liver cirrhosis symptoms
Many symptoms may indicate pathology, but sometimes signs of the disease do not appear. Therefore, you should not always wait for open signals; it is enough to take care of your health. Doctors recommend checking the abdominal organs regularly, since the disease tends to progress slowly. In NEARMEDIC clinics, complete diagnostics are carried out during preventive examinations. Thanks to this, it is often possible to detect pathology in men and women in the initial stages and begin treatment on time.
The disease, complicated by concomitant pathologies, can develop very quickly. If tissue damage is not stopped, the disease can lead to irreversible consequences within a year. The disease itself often develops within 5-6 years; if it occurs in a latent form, then the patient comes to the doctor with symptoms that arose from complications.
Types of cirrhosis and symptoms
Various signs of the disease may be observed, depending on the form and stage. In medicine, there are several types of disease, each of which arises for its own reasons and proceeds differently.
Toxic cirrhosis of the liver
The disease occurs against the background of intoxication. This could be minor poisoning, systematic use of toxic substances. For example, antibiotics, non-steroidal anti-inflammatory drugs, taking anabolic steroids and others. Working with chemicals can also lead to the development of liver pathology. Some herbs can affect the body when brewed almost on par with mercury and cadmium.
With gradual poisoning, progressive destruction occurs. However, symptoms can appear already at the most life-threatening stages; they manifest themselves acutely, with a whole set of unpleasant signs.
- increased fatigue, loss of appetite, sudden weight loss;
- the temperature rises, hypothermia may occur;
- yellowness of the skin and eyes;
- the level of hemoglobin in the blood drops;
- the condition of the skin changes: itching appears, a vascular network forms;
- pain on the right (if there is no pain with other symptoms, this indicates a worsening situation);
- an increase in the size of the abdomen, vomiting blood, blood from the nose (internal bleeding).
The toxic form can lead to mental disorders and impaired consciousness.
Reasons for development
It has not yet been possible to establish the specific cause of the formation of biliary cirrhosis. Some theories of its formation are considered:
- hereditary predisposition to the disease;
- previous infectious liver lesions - viral, bacterial, parasitic;
- toxic liver damage;
- autoimmune inflammation.
It is currently impossible to confirm a direct connection between these conditions and the formation of cirrhosis.
First, under the influence of certain reasons, lymphocytes begin to destroy the cells of the bile ducts - an inflammatory process is formed in them. Due to inflammation, the patency of the ducts is disrupted and bile stagnation develops. In these areas, hepatocytes are damaged and inflammation develops again. Massive cell death can lead to the formation of cirrhosis.
Alcoholic cirrhosis of the liver
The disease is triggered by regular alcohol consumption. The usual “100 grams” every day after work may well lead to the development of the disease. The body suffers especially if the patient eats abnormally. A small amount of food or accompanying consumption of harmful food significantly increases the risks.
Liver cirrhosis: stages and symptoms in alcoholic form
At the initial stage, the pathology does not make itself felt and develops hidden. However, hardware studies reveal increased sizes of the organ.
This type of disease is characterized by reproductive dysfunction: women experience spontaneous abortions, men experience impotence and testicular atrophy. The same disorders include hormonal imbalances in the body.
How does the alcoholic form of the disease manifest:
- bowel dysfunction;
- loss of appetite;
- regular attacks of nausea and vomiting;
- loss of sensation in the limbs;
- muscle tissue becomes thinner.
Among the subtle symptoms are protein and vitamin deficiency in the body.
Causes of cirrhosis
According to statistics, about 50% of liver cirrhosis is associated with alcohol abuse and the development of alcoholic liver disease (ALD). 1Moreover, 25% of them had a history of viral hepatitis.1
Other causes of cirrhosis include2:
- metabolic diseases associated with excessive accumulation of iron, copper and other elements;
- Autoimmune lesions;
- Primary and secondary biliary cirrhosis;
- Diseases of the vascular system (Budd-Chiari disease);
- Long-term use of medications that have a toxic effect on the liver;
- non-alcoholic fatty liver disease (NAFLD), which is associated with the accumulation of large amounts of free fatty acids in hepatocytes (liver cells), is characterized by a chronic course and potential progression from stage to stage: steatosis - steatohepatitis - fibrosis - cirrhosis (same as alcoholic disease liver, but the likelihood of developing cirrhosis in AFLLD is 10 times higher).5
Regardless of the cause, cirrhosis develops in the same way: the lobular structure of the liver is disrupted with the formation of nodes in place of destroyed hepatocytes—the so-called false lobules.
- Small nodular - the size of fibrous nodes is no more than 3 mm;
- Large nodular - nodes 3-5 mm;
- Mixed.
Viral cirrhosis of the liver
The disease can develop as a result of viral hepatitis B, C and D. Infection with these viral infections occurs through the blood, sexually (hepatitis B), and they can also be acquired in utero from the mother.
Most often, symptoms appear in the last stages. However, there are a number of symptoms that may signal the disease.
- lethargy, loss of strength (affect performance);
- the liver increases in size and becomes denser;
- the patient experiences weight loss, nausea (sometimes to the point of vomiting);
- aching nagging pain in the liver area.
If the viral form develops into liver failure, then the symptoms rapidly change, the patient’s condition sharply worsens:
- weight drops significantly;
- swelling of the limbs appears;
- vomiting, diarrhea and constant nausea;
- nervousness, sleep problems, loss of performance due to weakness;
- itching of the skin;
- yellowness is pronounced on the skin, as well as yellowness of the eyeballs;
- problems with blood pressure and heart rate;
- bleeding is observed from the mucous membranes of the mouth, in the gastrointestinal tract, and at the injection site.
Symptoms
In the initial period of its development, the disease may not manifest itself with specific symptoms. Occurring pathological changes in the organs of the hepatobiliary system are diagnosed accidentally, during a routine medical examination or medical examination. The asymptomatic period can last several years, which is extremely dangerous because the person is unaware of the presence of the disease, which progresses silently, killing liver cells.
Typical symptoms of PBC at an early stage: dysania (sleep disorder) or chronic drowsiness, loss of strength, causeless lethargy, asthenia (neuropsychological weakness), loss of appetite. After a short period of time, skin itching occurs, first affecting the palms and feet, then spreading throughout the body. Treatment with dermatological agents for external use has no effect.
Scratching on the skin heals slowly, and if a bacterial infection occurs, it turns into suppuration. Itchy symptoms are most troublesome at night. Against the background of a general decrease in tone, constant lack of sleep due to itching negatively affects the psycho-emotional state of the patient. The person becomes irritable, sometimes aggressive. A little later, a bitter taste in the mouth (usually after waking up) and discomfort in the right hypochondrium appear.
The skin and eyeballs gradually turn yellow. A capillary network (spider veins) is visible under the skin. Due to high cholesterol and lipid metabolism disorders, subcutaneous deposits of triglycerides (fats) - xanthomas - appear on the body. They look like solid yellowish nodules and are localized, most often, on the eyelids, chest (in women - under the mammary glands).
Xanthomas can have different shapes and sizes
The development of cholestasis disrupts metabolic processes, causing the body’s inability to fully absorb vitamins, micro- and macroelements and other nutrients and essential amino acids. This leads to the manifestation of the following symptoms: loss of body weight without changes in diet and exercise, alternating constipation (constipation) and diarrhea (diarrhea), intense gas formation, heaviness in the epigastric (epigastric) region. As the disease progresses, the condition worsens. Hematomas appear on the body (without mechanical impact).
Observed:
- stable hyperthermia;
- eating disorder;
- bloating;
- dark brown urine color;
- greasy consistency and discoloration of excrement (steatorrhea);
- swelling and discoloration of the tongue to purple (“liver tongue”);
- hemorrhoidal cones in the rectum and perianal area;
- regular nosebleeds.
In the third and fourth stages, symptoms progress. The feet and palms swell greatly. Due to a deficiency of calcium and vitamin B, bones become brittle and dental problems appear. The skin and eyeballs have an intense yellow color. Numerous symptoms of associated complications develop.
FAQ
How to deal with insomnia with liver cirrhosis?
Proper rest is an integral part of successful treatment. You need to sleep at least 8 hours a day. The cause of insomnia in CP is stress. Experiences and imbalances in the level of melatonin and cortisol in the body. To overcome insomnia, it is recommended to go to bed at the same time every day. You should also not forget about outdoor walks and physical activity during the daytime.
You can see prices for services