The article was prepared by a specialist for informational purposes only. We urge you not to self-medicate. When the first symptoms appear, consult a doctor.
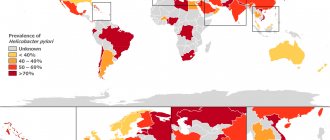
Half a century ago, there were several theories offering their own version of the causes of gastric and intestinal ulcers. The turning point came in 1979, when, as a result of scientific research, it was proven that the primary source of this problem is the bacterium Helicobacter pylori, which normally safely exists in the gastrointestinal tract of more than half of all representatives of humanity. Any decrease in immune defense is a good reason for the proliferation of Helicobacter pylori colonies. To treat heliobacteriosis, schemes have been created to eradicate pathogenic bacteria from the human body.
A little about Helicobater pylori and the concept of “eradication”
Helicobacter pylori is a microorganism that causes erosive processes in the mucous membranes of the gastrointestinal tract.
Helicobacter pylori is a pathogen that is able to live and multiply in conditions of aggressive contents of the human stomach.
This microorganism causes erosive processes in the mucous membranes of the gastrointestinal tract. Methods for determining Helicobacter in the body:
- Examination and interview of the patient
- Gastroscopy of the stomach with sampling of contents for analysis
- Blood tests
- Immunological tests
- Breath test
- PCR tests
- Culture of stomach contents
- Once the presence of a pathogen is confirmed, the physician must take steps to remove the pathogen.
Eradication is a medical term that denotes a set of measures aimed at destroying the infection and creating favorable conditions for the restoration of the body. Simply put, this is a high-quality treatment for Helicobacter pylori infection.
For the first time, Berry Marshall tested the “eradication” technique. The scientist provoked an inflammatory process in his stomach by drinking an isolated culture of Helicobacter pylori. For treatment, B. Marshall used a combination of metronidazole and bismuth subcitrate.
The third line of eradication of Helicobacter pylori
It is extremely rare to switch to a third line of eradication therapy, but such a possibility still exists. Before starting the third regimen, the patient is tested for the sensitivity of the Helicobacter pylori strain to antibiotics.
3rd line drugs:
- Two antibiotics that have not been used before and have shown the highest degree of effectiveness in laboratory diagnostics;
- Bismuth preparations;
- Proton pump inhibitors.
Medicines based on bismuth (tricotassium bismuth dicitrate) have a complex effect:
- Relieves symptoms of dyspepsia (bloating, heartburn, gastralgia); acts against Helicobacter pylori as an effective bactericidal agent;
- Stimulate the regeneration of damage to the deeper layers of the stomach walls.
Third-line therapy according to the Maastricht recommendations of the third convocation includes drugs from the group of rifamycins (Rifabutin) and quinolones (Levofloxacin). This combination was effective in 91% of cases. The resistance of Helicobacter pylori to Rifabutin is very low, so its inclusion in the treatment protocol together with Amoxicillin and a proton pump inhibitor makes it possible to increase the effectiveness of therapy and even ignore the bacterial resistance to Metronidazole and Clarithromycin.
Requirements for eradication recommended by WHO
Treatment regimens for Helicobacter pylori infection have been developed and introduced into medical practice over the course of 30 years.
Currently, the Maastricht IV recommendations from 2005 are used. The criteria for the effectiveness of the Helicobacter treatment regimen are:
- Positive result in 80% of patients
- The duration of active therapy is no more than 14 days
- Use of non-toxic drugs
- The occurrence of side effects in no more than 10–15% of patients
- The intensity of side effects should not be such as to stop treatment
- Low drug resistance of Helicobacter
- Ease of use of medications
- Low frequency of taking medications. Use of long-acting drugs
- Interchangeability of medications in various treatment regimens
Second line of eradication of Helicobacter pylori
Four components of a second line eradication regimen:
- 2 antibiotics: Tetracycline + Metronidazole, or Amoxicillin + a drug from the nitrofuran group;
- Proton pump inhibitor;
- Bismuth preparation.
Bismuth-based preparations are excellent cytoprotectors that restore the structure of cells in the gastric and intestinal mucosa and their resistance to the aggressive effects of acid and waste products of Helicobacter pylori. In addition, they have a bactericidal effect and minimize the risk of relapse of heliobacteriosis. When planning a second-line eradication regimen, it is not recommended to use previously used antibiotics. The effective, accessible and cheap regimen of quadruple therapy with bismuth is also not without its drawbacks:
- A large number of tablets taken (18 pieces per day);
- Frequent side effects;
- 4-fold dosing regimen.
To enhance the effectiveness of therapy with bismuth preparations, fruits, juices, and milk are excluded from the diet during treatment. The duration of second-line therapy is 10-14 days.
Eradication of Helicobacter with propolis
An aqueous solution of propolis is excellent in the fight against Helicobacter pylori.
This technique was patented in 2006. The authors are a group of Russian scientists.
Currently, propolis therapy is not included in official eradication schemes. Researchers insist on its effectiveness. The diagram looks like this:
- An aqueous solution of propolis with a mass fraction of the active substance of 25–30% orally 3 times a day before meals
- Propolis in oil – 2 times a day
- The drug "omeprazole" in standard dosage
- The duration of treatment ranges from 2 to 4 weeks.
Lapina T.L. Eradication therapy for Helicobacter pylori infection.
Eradication therapy for Helicobacter pylori infection
T.L.
Lapina 2005 is the year of two significant events associated with the microorganism Helicobacter pylori. The first event has a huge public resonance: the Nobel Prize in Physiology or Medicine in 2005 was awarded to two Australian researchers - Barry J. Marshall and J. Robin Warren for the discovery of “the bacterium Helicobacter pylori and its role in gastritis and peptic ulcers.” The first culture of a then unknown microbe, isolated from biopsy specimens of the human antrum, was obtained in 1982. Since then, a significant amount of knowledge has been accumulated about the significance of H. pylori in the pathogenesis of human diseases and the possibilities of therapy for these diseases. The second event was expected by doctors and specialists. This is another revision of authoritative European recommendations for the diagnosis and treatment of H. pylori infection. Based on the name of the place where the first conferences to develop consensus in this area were held - the city of Maastricht - the recommendations are called Maastricht, and based on the number of such conferences - the third Maastricht recommendations (the previous conferences were held in 1996 and 2000).
Indications for eradication therapy of H. pylori infection
The indications
for mandatory treatment aimed at destroying H. pylori are:
• Peptic ulcer of the stomach and duodenum, both in the acute and remission stages, as well as after treatment of complications - complicated forms.
• MALToma (rare tumor - B-cell lymphoma, originating from lymphoid tissue associated with mucous membranes).
• Atrophic gastritis.
• Condition after gastric resection for cancer;
• Close relationship with persons suffering from stomach cancer (that is, eradication of H. pylori is indicated for persons who are close relatives of patients with stomach cancer).
• The desire of the patient (after full consultation with the doctor).
The above list of indications was proposed by the participants of the Maastricht Conference back in 2000. Over the past 5 years, it has been possible to accumulate enough new facts that confirm the correctness of the choice of these conditions for mandatory anti-helicobacter therapy. It has been objectively shown that it is the destruction of H. pylori in peptic ulcer disease that leads not only to successful healing of the ulcer, but to a significant reduction in the frequency of relapses of the disease, as well as to the prevention of complications of the disease. Eradication therapy for H. pylori in atrophic gastritis, in relatives of patients with stomach cancer, and also after gastric resection for cancer is regarded as a preventive measure to prevent precancerous changes in the gastric mucosa and cancer itself.
Dyspepsia syndrome (pain and discomfort in the epigastric region) is one of the most common reasons for visiting a general practitioner and gastroenterologist. Should the diagnosis of H. pylori and anti-Helicobacter therapy be planned as necessary measures in the presence of dyspepsia syndrome? International experts propose to distinguish two clinical situations: 1) dyspepsia syndrome, the cause of which has not been established; 2) an established diagnosis of a functional disease - functional dyspepsia. When first contacting a doctor for dyspepsia (“unspecified” dyspepsia), persons under 45 years of age without warning symptoms (weight loss, fever, dysphagia, signs of bleeding) are advised not to undergo an endoscopic examination and to follow a “test-and-treat” strategy. “Test-and-treat” involves diagnosing H. pylori using a non-invasive method (not requiring endoscopic examination with a biopsy) and prescribing eradication therapy if the result is positive. In countries with a high incidence of H. pylori infection (such countries include Russia), this approach allows saving healthcare resources and achieving a positive clinical effect from empirical anti-Helicobacter therapy.
H. pylori eradication therapy should be considered an acceptable treatment option for functional dyspepsia, especially in countries with a high incidence of infection. As evidence for this statement, we present data from a systematic review of the Cochrane Foundation (P. Moayyedi, S. Soo, J. Deeks et al.s 2006). An analysis of 13 randomized controlled trials (with a total of 3186 patients) showed that the relative risk of dyspeptic complaints in patients undergoing H. pylori eradication was reduced by 8% (95% CI = 3% - 12%) compared with the group receiving placebo. NNT (to cure 1 case of dyspepsia) was 18 (95% CI = 12 - 48). The positive effect of anti-helicobacter therapy in patients with functional dyspepsia is statistically significant, although insignificant. This, apparently, determined the recommendatory (but not mandatory) nature of prescribing eradication therapy for functional dyspepsia.
, astroesophageal reflux disease and gastropathy induced by non-steroidal anti-inflammatory drugs can be called urgent problems of modern gastroenterology.
. The significance of H. pylori in the pathogenesis of these diseases is controversial, and anti-Helicobacter therapy should be subject to a number of provisions.
Eradication of H. pylori does not provoke the development of gastroesophageal reflux disease.
Eradication of H. pylori does not affect the outcome of the use of basic drugs for the treatment of reflux disease - proton pump inhibitors. Diagnosis of H. pylori should not be regarded as a routine test for esophageal reflux disease, however, determination of H. pylori and anti-helicobacter therapy should be carried out in patients who require long-term maintenance use of proton pump inhibitors.
This recommendation is based on the interesting relationship between chronic gastritis caused by H. pylori and gastroesophageal reflux disease requiring treatment with a proton pump inhibitor. About 10 years ago, data were published on the accelerated development of atrophy (especially in the body of the stomach) with long-term therapy with histamine H2 receptor blockers and proton pump inhibitors. Atrophic gastritis is a precancerous disease, which calls into question the safety of the use of these powerful antisecretory agents. With a more detailed study of the relationship between atrophic gastritis and proton pump inhibitors, it turned out that the drugs do not have any effect on the morphology of the gastric mucosa. The cause of chronic gastritis is H. pylori infection. The proton pump inhibitor, having a significant effect on the pH of the stomach, alkalizes the microenvironment of the bacteria, making their viability almost impossible. With monotherapy with a proton pump inhibitor, H. pylori is redistributed throughout the gastric mucosa - from the antrum it moves into the body of the stomach with lower pH values, where inflammation is activated.
BE Schenk et al. (2000) studied the characteristics of gastritis in gastroesophageal reflux disease during 12 months of treatment with omeprazole 40 mg in three groups: 1) H. pylori-positive patients underwent eradication therapy; 2) H. pylori-positive patients received placebo instead of eradication therapy; 3) patients initially without H. pylori infection. When H. pylori persisted, inflammatory activity increased in the body of the stomach and decreased in the antrum; with successful eradication of H. pylori, inflammatory activity decreased both in the body of the stomach and in the antrum; in patients initially without H. pylori infection, no histological changes were detected. Thus, there is no connection between the progression of atrophic gastritis and taking omeprazole. Progression of atrophic gastritis occurs only against the background of the presence of H. pylori infection. This led to the recommendation to first destroy the microorganism, and only then prescribe proton pump inhibitors for a long term for reflux disease of the esophagus.
Relationships of gastropathy induced by non-steroidal anti-inflammatory drugs
(NSAIDs), and H. pylori, the authors of international recommendations were also summarized in several provisions.
• H. pylori eradication is indicated for people who are forced to take NSAIDs for a long time, but this course is not enough to prevent the occurrence of ulcers.
• Before starting a course of NSAIDs, anti-helicobacter therapy should be carried out to prevent ulceration and bleeding.
• If long-term use of aspirin is necessary and if there is a history of bleeding, a test should be performed to determine H. pylori infection and, if positive, anti-Helicobacter treatment should be prescribed.
• If long-term use of NSAIDs is required and peptic ulcers and/or bleeding are present, maintenance therapy with proton pump inhibitors is more effective than eradication of H. pylori infection (to prevent ulceration and bleeding).
First time in recommendations. Maastricht - 3 extragastric diseases, which through a number of pathogenetic mechanisms can be associated with H. pylori infection, were analyzed as indications for eradication therapy. So treatment can be prescribed for iron deficiency anemia, the cause of which is not established, or for idiopathic thrombocytopenic purpura. Despite the fact that the level of scientific evidence is not the highest and the degree of urgency of the recommendation is also not maximum, these provisions are certainly balanced and have a certain foundation. Thus, in a significant percentage of patients (50%) with idiopathic thrombocytopenic purpura, after successful eradication therapy for H. pylori infection, it is possible to achieve normalization of platelet levels.
Treatment regimens for eradication therapy of H. pylori infection
Regimen for successful H. pylori eradication therapy have been developed empirically, both in terms of their components, drug doses, and duration of treatment. They meet certain requirements for efficiency (consistently high percentage of microorganism destruction reproducible in various populations) and safety.
As first-line therapy, the following three-component treatment regimens are proposed (see Table 1): proton pump inhibitor (or ranitidine bismuth citrate) at a standard dosage 2 times a day + clarithromycin 500 mg 2 times a day + amoxicillin 1000 mg 2 times a day or metronidazole 500 mg 2 times a day. The combination of clarithromycin with amoxicillin is preferable to clarithromycin with metronidazole. In our country, this is primarily due to the levels of resistance of H. pylori strains to antibacterial agents. Thus, the percentage of strains resistant to metronidazole (in adult patients) in 2005 was 54.8%, and resistant to clarithromycin - 19.3% (L.V. Kudryavtseva, 2006: personal communication).
Table 1. Schemes of eradication therapy for H. pylori infection (1st line)
| 3rd component of the circuit | ||
| proton pump inhibitor: lansoprazole 30 mg twice daily or omeprazole 20 mg twice daily or pantoprazole 40 mg twice daily or rabeprazole 20 mg daily or esomeprazole 10 mg twice daily | Clarithromycin 500 mg twice daily | amoxicillin 1000 mg 2 times a day |
| or ranitidine bismuth citrate 400 mg 2 times a day | or metronidazole 500 mg 2 times a day |
If treatment is unsuccessful, second-line therapy is provided - a four-component treatment regimen: proton pump inhibitor (or ranitidine bismuth citrate) in a standard dosage 2 times a day + bismuth subsalicylate/subcitrate 120 mg 4 times a day + metronidazole 500 mg 3 times a day + tetracycline 500 mg 4 times a day (see Table 2). One of the new provisions of the Maastricht Consensus 3 is an indication of the possibility of using quadruple therapy in certain clinical situations as first-line therapy (alternative first-line therapy).
Table 2. Schemes of four-component eradication therapy for H. pylori infection (2nd line)
| 1st circuit component | 2nd circuit component | 3rd component of the circuit | 4th circuit component |
| proton pump inhibitor: lansoprazole 30 mg twice daily or omeprazole 20 mg twice daily or pantoprazole 40 mg twice daily or rabeprazole 20 mg daily or esomeprazole 10 mg twice daily | bismuth subsalicylate/subcitrate 120 mg 4 times a day | metronidazole 500 mg 3 times a day | tetracycline 500 mg 4 times a day |
Has the understanding of optimal first-line therapy changed in the 5 years since the adoption of the Maastricht Consensus 2? One of the current provisions of Maastricht 3 is that the combination of proton pump inhibitor - clarithromycin - amoxicillin or metronidazole remains the recommended first-line therapy for populations with a frequency of clarithromycin-resistant strains less than 15 - 20%. In populations with a metronidazole resistance rate of less than 40%, the proton pump inhibitor-clarithromcin-metronidazole regimen is preferable. The above domestic data on antibiotic resistance focus our attention specifically on the “proton pump inhibitor - clarithromycin - amoxicillin” scheme.
The minimum duration of triple therapy is 7 days. However, according to modern data, it turned out that for the regimen “proton pump inhibitor - clarithromycin - amoxicillin or metronidazole”, a 14-day course of treatment is more effective than a 7-day course (by 12%; 95% CI 7 - 17%). However, 7-day triple therapy may be adopted if local studies show it to be highly effective and serves as a more cost-effective choice in countries with low healthcare costs.
Thus, it should be concluded that the range of indications for H. pylori eradication therapy is expanding. Standardized triple therapy remains a reliable tool in the treatment of H. pylori-associated diseases.
Eradication therapy for Helicobacter pylori infection.
T.L. Lapina.
Clinic of Propaedeutics of Internal Diseases, Gastroenterology and Hepatology named after. V.Kh. Vasilenko MMA named after. THEM. Sechenov.
Helicobacter eradication with folk remedies
A decoction of flax seed is a folk remedy in the treatment of Helicobacter.
Herbal medicine is widely used in the treatment of Helicobacter pylori infection. Many of them are included in traditional medicine courses and are prescribed by a doctor. What can be used during treatment:
- Flax seed decoction - prepared using classical technology - 250 ml of boiling water for 1 teaspoon of raw material. Pour in and leave for 2 hours. Take the slimy infusion along with the swollen seed. Flax has an enveloping effect on the inner lining of the stomach, prevents irritation of areas of erosion by hydrochloric acid, and promotes their healing.
- A decoction of chamomile and yarrow, sea buckthorn oil - they have an anti-inflammatory and wound-healing effect.
- Do not use aggressive foods and juices. Garlic and onions, although they are powerful antiseptic products, are prohibited for erosive processes in the gastrointestinal tract.
Do not prescribe herbal medicine or other traditional medicine recipes without consulting your doctor.
Independence during the “eradication” of Helicobacter can result in perforation of a section of the stomach or duodenum.