Very often, a general practitioner at a medical center has to deal with the conclusion of an ultrasound specialist who has examined the liver and gallbladder, where the expression “Sludge syndrome” is used. What is it?
Sludge translated from Latin means mud, dirt. Biliary sludge (BS) is any heterogeneity of bile or sediment formed during stagnation of bile, identified by echo examination. In fact, BS is a clinical form of cholelithiasis, its initial stage. The frequency of detection of biliary sludge syndrome, according to various sources, ranges from 7% to 60%, depending on the concomitant pathology.
Causes of the disease and its varieties
Experts call the following main prerequisites for the occurrence of sludge syndrome. First of all, this is:
- Impaired motility of the gallbladder.
- Changes in bile lithogenicity, heterogeneity in the gallbladder.
- Inflammation of the walls of the gallbladder.
There are 3 types of BS:
- Microlithiasis is a suspension of hyperechoic microparticles, from single to multiple.
- Putty-like bile clots are heterogeneous bile with clots of varying densities.
- Mixed type, i.e. a combination of putty-like bile with microliths.
If we talk about the types of pathology, then we are talking about:
- primary sludge is a syndrome that occurs as an independent disease, there is no connection with another pathology;
- Secondary BS occurs against the background of concomitant pathology, and it is very diverse, ranging from blood diseases to metabolic disorders.
Experienced therapists consider risk factors for the disease to be:
- gender, often female;
- heredity;
- obesity;
- sedentary lifestyle;
- nature of nutrition;
- age;
- alcohol abuse.
On the frequency of detection of “bile sludge” using ultrasound
SonoAce Ultrasound Magazine
Contains current clinical information on ultrasonography and is aimed at ultrasound doctors, published since 1996.
Introduction
With the development of various imaging methods, in particular ultrasonography, specific nosological forms have appeared, among which “bile sludge” (previously not diagnosed using x-ray examination) is found. “Bile sludge” is a mixture of mucus, calcium bilirubinate and cholesterol crystals. It appears when bile becomes thick and viscous, replacing normal bile [1, 2].
There are different points of view regarding the etiology and pathogenesis of sludge. Some view “bile sludge” as a precursor to gallstones, while others view it as a transient, reversible condition of bile balance. “Bile sludge” appears when the ratio of the main components of bile changes or a violation of gallbladder emptying develops.
Considering the etiology of “bile sludge”, it can be classified into secondary and primary. Secondary sludge appears when there is a well-known etiopathogenetic condition: after shock wave lithotripsy for gallstones, gallstone disease, pregnancy [3, 4], liver cirrhosis, obstructive jaundice, hydrocele of the gallbladder, long-term parenteral nutrition [5, 6], diabetes mellitus, sickle cell anemia [7], after taking ceftriaxone [8, 9]. Primary sludge is regarded in cases where none of the above conditions can be identified.
Materials and methods
In a study conducted in the USA, “bile sludge” appeared as a hyperechoic formation in the gallbladder with a horizontal level without a posterior shadow, the shape of which slowly changed with the movement of the patient [10]. A characteristic sign of “bile sludge” is a change in its appearance on the scanogram depending on the change in the position of the patient’s body and the slow achievement of a new horizontal level. The general rule is the absence of a distal acoustic shadow. The echogenicity of sludge can vary. Sometimes sludge fills the entire gallbladder, making it difficult to differentiate between liver tissue and the gallbladder. This situation is called “hepatization of the gallbladder” (Fig. 1).
Rice. 1.
Hepatization of the gallbladder, completely filled with sludge.
In addition to the typical appearance, “bile sludge” can have a special appearance, similar to a round polypoidal space-occupying formation with sharp edges or an uneven contour (“tumor-like bile sludge” or “sludge balls” [12, 13]). When the patient's position changes, sludge balls are seen rolling or collapsing, then again forming the original space-occupying formation (Fig. 2-8).
Rice. 2.
Gallbladder half filled with sludge.
Rice. 3.
Large gallbladder with sludge.
Rice. 4.
“Bile sludge” in a patient with liver cirrhosis.
Rice. 5.
Gallbladder filled with sludge in a patient with cirrhosis.
Rice. 6.
Gallbladder and bile sludge.
Rice. 7.
“Bile sludge” in the form of a ball.
Rice. 8.
Ball-like "bile sludge".
Using the definition of “bile sludge,” we prospectively screened 11,800 patients for sludge detection using an ultrasound scanner with 3.5 and 5 MHz convex and sector probes. Ultrasound examination was performed after at least a 10-hour fasting period.
Based on clinical or paraclinical data, we divided sludge into primary and secondary.
results
“Bile sludge” was diagnosed in 68 (0.6%) patients, including 39 men and 29 women. The average age of those examined was 55.3 years. Considering the etiology of sludge, we found secondary “bilious sludge” in 75% of cases (51 patients), and primary in 25% (17 patients) (Fig. 9).
Rice. 9.
Etiology of “bile sludge”.
Secondary sludge was more often found in liver cirrhosis (22 cases), then with concomitant gallstones (15 people) and obstructive jaundice (11 patients) (Fig. 10).
Rice. 10.
Cases of secondary sludge.
Discussion
The presence of “bilious sludge” in 0.6% of patients who underwent ultrasound examination means that this nosological form is relatively rare. While the question regarding secondary sludge is quite clear, the clinical significance of primary “bilious sludge” is not yet fully understood. In a study of 96 patients with gallstones, ultrasound follow-up was carried out for an average of 38 months, and W. Middleton [14] showed that 14 (14.5%) patients developed gallstones, 6 (6.2%) patients with sludge complained of hepatic colic (in the absence of cholelithiasis).
Given that gallstones may develop in a proportion (15%) of patients with primary bile sludge, treatment with ursodeoxycholic acid may be effective [15], but the treatment strategy is not yet well established. Another option is to monitor these patients for a long time and then treat only those who develop small gallstones.
As for tumor-like bile sludge, its ultrasound diagnosis can be difficult because differential diagnosis with cancer and gall bladder stones is required (in particular, bilirubin stones sometimes have a subtle acoustic shadow).
Another aspect that needs to be discussed is the false appearance of sludge when the sound power is mismatched (too much gain). To correctly determine the localization of sludge, it is necessary to monitor its movement by changing the position of the patient’s body. But for a sufficiently experienced ultrasound technician, correctly diagnosing sludge is almost never difficult.
conclusions
With the advent of new imaging techniques, the detection of “bile sludge” has become a reality, which has clinical significance. Its frequency is not so high (0.6% of all cases examined with ultrasound), but individual patients with primary “bile sludge” require follow-up to subsequently decide on possible treatment.
Literature
- Goldberg V. Textbook of abdominal ultrasound. Baltimore: Williams and Wilkins, 1993.
- Terada T, Nakanuma Y, Sat to K, Kono N. Biliary sludge and microcalculi in intrahepatic bileduct. Morphological and X-ray microanalytical observations in 18 among 1,179 consecutively autopsied livers. Acta Pathol JPN 1990; 40(12): 894-901.
- Caruso MG, Giangrande M, Clemente C, et al. Serum lipids and biliary sludge during pregnancy. Minerva Gastroenterol Dietol 1993; 39(2): 67-70.
- Maringhini A, Ciambra M, Baccelliere P, et al. Biliary sludge and gallstones in pregnancy: incidence, risk factors and natural history. Ann Intern Med 1993; 119(2): 116-120.
- Murray FE, Stinchcombe SJ, Hawkey CJ. Development of biliary sludge in patients on intensive care unit: results of prospective ultrasonographic study. Gut 1992; 33(8): 1123-1125.
- Sitzmann JV, Pitt HA, Steinborn PA, et al. Cholecystokinin prevents parenteral nutrition induced biliary sludge in humans. Surg Gynecol Obstet 1990;170(l):25-31.
- Nzeh DA, Adedoyin MA. Sonographic pattern of gallbladder disease in children with sickle cell anemia. Pediatr Radiol 1989; 19(5): 290-292.
- Michielsen PP, Fiersens H, Van-Maercke YM. Drug induced gallbladder disease. Incidence, aetiology and management. Drug Saf 1992; 7(1): 32-45.
- Shiffman ML, Keith FB, Moore EV. Pathogenesis of ceftriaxone-associated biliary sludge. In vitro studies of calcium-ceftriaxone binding and solubility. Gastroenterology 1990; 99(6): 1172-1178.
- Angelico M, De-Santis A, Capocaccia L. Biliary sludge: a critical update. J Clin Gastroenterol 1990; 12(6): 656-662.
- Fakhry J. Sonography of tumefactive biliary sludge. Am J Roentgenol 1982; 139:717.
- Cann R. Gallbladder and biliary tree. In: Kawamura DM, eds. Diagnostic medical sonography - a guide to clinical practice. Philadelphia: Lippincott Co., 1992.
- Hisami A. Ultrasonic characteristics of tumefactive biliary sludge. J Clin Ultrasound 1986; 14: 289-292.
- Middleton W. Gallbladder. In: Textbook of abdominal ultrasound. Baltimore: Williams and Wilkins, 1993.
- Guma C, Violaq L, Apestegui C, et al. Therapeutic efficacy of ursodeoxycholic acid in persistent gallbladder lithiasis and persistent biliary sludge: preliminary results of a multicenter experience. Acta Gastroenterol Latinoam 1994; 24(4): 233-237.
SonoAce Ultrasound Magazine
Contains current clinical information on ultrasonography and is aimed at ultrasound doctors, published since 1996.
What are the causes of the pathology?
- Liver diseases, liver cirrhosis, viral hepatitis, Gilbert's syndrome and other disorders of bilirubin metabolism.
- Diseases of the cardiovascular system.
- Alcoholic pancreatitis.
- Gallbladder diseases.
- Intestinal pathology: Crohn's disease, prolonged constipation, etc.
- Blood diseases: hemolytic anemia, thalassemia.
- Taking medications (cytostatics, diuretics, oral contraceptives, fibrates, calcium supplements, abuse of laxatives, vitamins, etc.).
- Fast weight loss.
- Diabetes mellitus, pathology of the parathyroid glands, obesity.
- Violation of protein and mineral metabolism.
- Pregnancy.
- Sedentary lifestyle.
13. Limiting fluid intake.
What may indicate a disease
Despite the fact that modern medicine has moved far beyond its initial manifestations, even experienced specialists are not always able to diagnose some diseases in a timely and accurate manner. For example, if you overlook biliary sludge, this will lead to the development of gallstone disease. Therefore, when a patient contacts, in order to exclude/confirm not only this, but also any other disease, the doctor prescribes a series of tests that can reliably show a picture of the state of the body at the moment.
In addition, each of us should also be very attentive to ourselves and notice various changes in our body. If you are bothered by the same symptoms every day (headache, heart pain, abdominal pain, dizziness, nausea, etc.), be sure to call a specialist or go to the nearest clinic.
But what is sludge syndrome? To answer this question, we turned to a medical reference book, which gave the following explanation of this term:
Sludge syndrome is the heterogeneity of bile or its stagnation in the gallbladder, in which formations (calcium salts, cholesterol crystals and protein) are most often observed, which are revealed during echographic/ultrasound examination.
This syndrome, if you are attentive to yourself, can be suspected by the following signs:
- pain in the hypochondrium (mainly manifests itself on the right side). The intensity varies: sometimes it intensifies after eating, sometimes it is paroxysmal, sometimes it is oppressive and constant.
- appetite decreases.
- often after eating food, vomiting occurs, sometimes with an admixture of bile.
- Nausea or heartburn does not stop during the day.
- stool is disturbed.
Symptoms of the disease
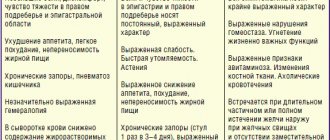
Extensive practical experience as a clinician allows us to assert that clinical manifestations of biliary sludge in some cases may be completely absent in patients, but can also cause complications, including surgical interventions.
The most commonly observed symptoms are:
- pain, heaviness in the right hypochondrium;
- biliary pancreatitis;
- acute cholecystitis;
- disabled gallbladder;
- strictures of the terminal portion of the common bile duct.
Gallstone disease stage II. Causes and factors for the formation of cholesterol stones
Among the reasons contributing to the formation of biliary sludge (BS), there are four main groups of risk factors that characterize gallstone disease.
Factors contributing to the oversaturation of bile with cholesterol:
- Age, often female, during pregnancy the contractile function of the gallbladder often suffers, which contributes to the formation of biliary sludge, heredity.
- Taking oral contraceptives and estrogen-containing drugs during menopause increases the risk of gallstone formation by 2-2.5 times. Calcium supplements increase the risk of developing BS.
- Excess body weight is an important risk factor for BS, contributing to increased cholesterol synthesis and its excretion through the biliary tract. It should be noted that low-calorie diets, which are used for weight loss, in 25% of cases are accompanied by the formation of BS and the formation of stones.
- Nutrition. Foods low in dietary fiber slow down its movement through the intestines, increase the absorption of secondary bile acids and change the quality of bile. Eating fatty foods containing a lot of cholesterol and refined (purified) foods increase the level of cholesterol in the bile. Small doses of alcohol, on the contrary, reduce its content in bile.
- Liver diseases. With viral hepatitis A, B, G, TTV, an opinion is expressed about the possibility of the formation of gallstones. Diseases of the small intestine (celiac disease, resection of the small intestine), Crohn's disease, etc. disrupt all types of metabolism, including the absorption of bile acids.
- Impaired contractile function of the gallbladder is one of the leading factors in the formation of biliary sludge and stone formation.
Thus, supersaturation of bile with cholesterol is a prerequisite for the formation of BS, but not the only one. An important role is played by the disruption of the quality of bile, all its components, the formation of mucus and the deposition of cholesterol crystals, and disruption of the contractile function of the gallbladder.
Treatment of biliary sludge
The treatment regimen is selected by the attending physician individually for each patient, depending on the personal qualities and stage of the disease. It usually includes such drug and non-drug therapies as:
- Diet table No. 5 according to Pevzner constantly.
- Increased physical activity.
- Increasing fluid intake, namely water.
- Correction of the underlying disease.
- Prescription of antispasmodics (duspatalin, odeston).
- Restoration of intestinal microflora (pro- and prebiotics).
- If complications develop, surgical treatment is performed - cholecystectomy.
results
Thrombosis of the main trunk of the GSV against the background of varicose transformation (C2-C4) in 6 cases developed in patients with degree II sludge effect (100%) 3-6 months after the initial detection of the phenomenon. In all cases, there was an ascending nature of the thrombotic process at the femoral level. In 2 patients (33%), the results of dynamic HT revealed floating thrombosis.
In other cases, there is occlusive thrombosis with the apex at the level of the upper third of the thigh (crossectomy was performed in all cases). The growth of identified blood clots began at the level of incompetent valves with a sludge effect. It should be noted that all patients at the time of the initial detection of the sludge effect were using compression garments and also received venotonics and antiplatelet agents.
Literature
1. Bakulin I.G., Sandler Yu.G. Possibilities of using hepatoprotectors in the practice of a general practitioner. Consilium medicum. Gastroenterology. 2010; 8: 72–76. 2. Balakina I.V. Studying the effectiveness of the drug RezalutR in the treatment of non-alcoholic steatohepatitis accompanied by dyslipoproteinemia. Clinic. 2012; 1: 118–119. 3. Ilchenko A.A. Biliary sludge: causes of formation, diagnosis and treatment. Consilium Medicum. Gastroenterology. 2012; 2: 18–21. 4. Ilchenko A.A. A modern view of the problem of biliary sludge. RMJ. Diseases of the digestive system. 2010; 28:1707–1713. 5. Ilchenko A.A., Delyukina O.V. Clinical significance of biliary sludge // Consilium medicum. – 2005. – No. 7. – P. 134–137. 6. Maev I.V., Dicheva D.T., Buragina T.A. Diagnosis and treatment of biliary sludge in patients with peptic ulcer disease. Russian Journal of Gastroenterology, Hepatology, Coloproctology. 2007; 4. 7. Mehdiev S.N., Grinevich V.B., Kravchuk Yu.A., Bogdanov R.N. Biliary sludge: unresolved issues. Attending doctor. 2007; 6:24–28. 8. Chubenko S.S. Microcholelithiasis. Doctor. 2004; 3:23–24. 9. Gallstone Disease; Sphincter of Oddi Dysfunction. https://www.hopkins-gi.org. 10. Jüngst C., Kullak-Ublick GA, Jüngst D. Gallstone disease: Microlithiasis and sludge. Best Pract. Res. Clin. Gastroenterol. 2006; 20:6:1053–1062. 11. Sporea Loan. On the frequency of detection of “bile sludge” using ultrasound. Honey. magazine SonoAce International. 1999; 5; 34–39.