Surely many of us today have heard about such a dangerous bacterium as Helicobacter Pylori. And those who haven’t heard should know that Helicobacter Pylori is a dangerous bacterium that doctors often discover when examining a patient who has serious problems with the stomach and duodenum. It got its name because of its appearance, helico is a screw-shaped bacterium, and pylori is the pyloric section in the stomach, its favorite habitat.
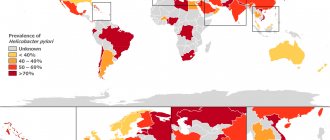
As studies have shown, up to 60% of the world's population is infected with this bacterium. It is one of the main causes of gastritis, as well as most diseases associated with the stomach. Therefore, diagnosis of Helicobacter Pylori is necessary, otherwise serious complications and illnesses may occur.
Gastritis
A morphological concept used to designate inflammatory and dystrophic changes in the gastric mucosa of different origin, course and clinical manifestations. It follows from this that the final diagnosis is valid only through histological examination of gastric biopsies.
It is quite difficult to judge the true epidemiology of chronic gastritis, which is associated with the need for morphological verification and the often hidden course of the disease.
- H.Pylori-associated gastritis accounts for about 85%.
- Autoimmune gastritis 1-5%.
- Special forms of gastritis - no more than 10%.
Contrary to common misconceptions among the population and even among some medical specialists, not everyone has chronic gastritis and is not a “harmless” disease. In some cases, against the background of chronic H. Pylori-associated gastritis, precancerous processes may occur asymptomatically, which cannot be diagnosed without a biopsy of the gastric mucosa. Timely detection and treatment of infections not only prevents their development, but can also reverse these changes.
Precancerous changes and diseases of the stomach, risk of malignancy (according to Baranskaya E.K., Ivashkin V.T. 2002 with amendments)
| Precancerous conditions and diseases of the stomach | Risk | Risk value % |
| Absolute | 70-90 |
| Unconditional | 20-70 |
| Definite | 10-20 |
| Likely | 5-10% |
| Possible | Less than 5 |
* - conditions that cannot be reliably diagnosed without examining gastric biopsies are highlighted in red.
H. Pylori-associated gastritis, as a rule, does not have obvious and specific symptoms, and screening measures for the microorganism are not included in the clinical examination plan in healthcare institutions.
The main method of treatment is antibacterial therapy with mandatory follow-up monitoring.
Why is Helicobacter pylori so dangerous?
Helicobacter pylori is a very dangerous bacterium.
This bacterium is very dangerous for several reasons:
- Firstly, it can survive in a very acidic environment, which was previously considered impossible. It does this by mixing into the mucous membrane with the help of flagella and enhancing ammonia secretion, which, in turn, reduces acidity. Previously, it was believed that bacteria could not survive in an acidic environment.
- Secondly, it is one of the main causes of diseases not only of the stomach, but also of the duodenum, primarily due to reproduction.
- Thirdly, this nasty bacterium is capable of destroying stomach cells, thereby provoking the release of harmful substances, which is what causes gastritis.
It is able to survive and remain in its habitat for many years and even decades. Since the bacterium infects different areas in the duodenum, in addition to gastritis, other diseases such as ulcers, duodenitis and even cancer may appear against the background of Helicobacter pylori.
Peptic ulcer of the stomach and duodenum
Peptic ulcer disease is usually called a disease characterized by the formation of an ulcerative defect that spreads beyond the muscular membrane.
Peptic ulcer disease is one of the most common gastrointestinal diseases. According to clinical observations, about 7-10% of the adult population of the world suffers or have suffered from this disease, while the results of pathological studies give higher figures, which indicates that in a number of patients the disease is hidden. Thus, in clinical practice it often happens that the first symptom of a peptic ulcer is bleeding, which is manifested by vomiting mixed with blood or darkening of the stool. In particular, an asymptomatic course is typical for active smokers.
The frequency of detection of H. Pylori on the surface of the gastric epithelium in patients with duodenal ulcer is quite high and, according to various authors, ranges from 91 to 100%. Moreover, the detectability of bacteria directly depends on the quantity and quality of diagnostic techniques used. In cases where the formation of a defect in the mucous membrane of the stomach and duodenum occurs while taking non-steroidal anti-inflammatory drugs (analgesics), an infection is also most often found.
The formation of an ulcerative defect is caused by the toxic effect of H. Pylori enzymes on the gastric mucosa and is associated with the presence of phospholipases, mucinases, proteases and urease activity in strains on the one hand and the peculiarity of the immune response of the human body on the other, which together can lead to the occurrence of the disease against the background of chronic gastritis.
Diagnosis of peptic ulcer:
Clinical picture (symptoms and signs of the disease). The main clinical symptom is pain in the upper abdomen, the nature of which depends on the size and location of the ulcerative defect, concomitant inflammation of the mucous membrane of the stomach and duodenum, involvement of the serous membrane in the pathological process, and the individual threshold of pain sensitivity.
The leading method for diagnosing the presence of ulcers of the gastroduodenal mucosa is endoscopic examination.
Analysis for H. Pylori is a necessary component of the examination plan for a patient with suspected peptic ulcer disease or with a detected ulcer.
Symptoms and diagnosis of Helicobacter pylori
The bacterium usually begins to become active against the background of a general weakening of the body, which usually occurs after a sore throat and other severe viral diseases. But it can make itself felt as a result of drastic changes in diet.
That is, in many cases, the bacterium may have no effect on the well-being of its carrier and may appear completely unexpectedly in a previously completely healthy person. And a person, not knowing the true cause of the stomach problem, begins to make wrong decisions and undergo treatment for a variety of diseases. At the same time, stomach problems do not go away at all, gastritis or an ulcer remains the same, because it is Helicobacter Pylori that causes them.
Symptoms of Helicobacter pylori:
- Regular constipation or diarrhea
- Severe heartburn
- Nausea
- Feeling of heaviness in the abdomen
- Belching and vomiting
- Allergic reaction
- Poor digestibility of meat
- Increased hair loss
- Bad breath, in the absence of any problems associated with the oral cavity
- Nail diseases such as fungus and brittleness
- Feeling full after eating very quickly
- Abdominal pain that occurs after eating
Helicobacter pylori can be diagnosed using a breath test.
In addition, in some cases, these symptoms can be confused with other diseases, so it is necessary to be diagnosed by professionals. It is better to immediately contact a gastroenterologist who will dispel your suspicions.
Gastric adenocarcinoma
Adenocarcinoma (stomach cancer) represents up to 95% of all malignant tumors of the stomach.
There are two histological subtypes with different epidemiological and prognostic characteristics:
- Intestinal type;
- Diffuse type.
Epidemiology
Currently, there is a worldwide trend of decreasing mortality from stomach cancer. However, despite this, GC is in 4th place in terms of incidence among all malignant neoplasms and in 2nd place among the leading causes of mortality from cancer (Parkin DM et al., 2001; Crew KD Neugut AI 2006). This is largely due to the fact that in the early stages the disease is asymptomatic, and the standard medical examination plan in healthcare institutions does not include either endoscopic diagnosis or testing for H. Pylori infection.
Countries with a high incidence of gastric cancer are simultaneously characterized by a similar level of H. Pylori prevalence in the population. At the same time, the decrease in the prevalence of infection in developed countries parallels the decrease in the incidence of stomach cancer (Crew KD Neugut AI 2006).
*NSAIDs - non-steroidal anti-inflammatory drugs; **ASA-acetylsalicylic acid.
MALT lymphoma
MALT lymphoma is an extranodal marginal zone B-cell lymphoma associated with mucous membranes. It is a non-Hodgkin lymphoma, the substrate of which is sufficiently mature malignantly transformed lymphocytes originating from solitary lymphoid follicles of the mucous membranes.
Currently, H. Pylori is considered as the main causative agent of the disease, but the incidence in the world is low and amounts to 1 case per 30,000-80,000 infected individuals.
Extragastroduodenal diseases and conditions with an established pathogenetic role of infection.
- Iron deficiency anemia of unspecified etiology;
- Idiopathic thromocytopenic purpura;
- Vitamin B12 deficiency.
According to the provisions of the fifth Maastricht consensus, these patients are indicated for diagnosis and treatment of H. Pylori infection. Other extragastroduodenal diseases and conditions in which the pathogenetic role of the infection is being investigated. H. pylori has positive and negative associations with a large number of other extragastroduodenal conditions/diseases.
The etiology of these relationships has not been proven.
H. pylori infection and the cytotoxin-associated gene product CagA(+) of H. Pylori strains are associated with the development of atherosclerosis. A relationship has been identified between H. pylori and some neurological diseases (stroke, Alzheimer's disease, Parkinson's disease). However, these data are insufficient to establish a clear cause-and-effect relationship or relationship with treatment. In a number of populations, an inverse relationship has been found between the frequency of H. pylori infection and the prevalence of certain diseases, such as bronchial asthma and obesity.
Also of considerable interest are the data that revealed that the correlation between H. Pylori seropositivity and preeclampsia was very significant with an odds ratio = 9.22. This association was even more pronounced during pregnancy with both preeclampsia and fetal growth restriction (OR=35.56). At the same time, the highest risk was determined by H. Pylori CagA(+) strains (Cardoropoli S. et al., 2011). Moreover, another study showed that antibodies against CagA can cross-react with the bate-actin of cytotrophoblast cells, hypothetically explaining the above-described clinical association (Franceschi F. Et al., 2012).
Diagnosis of H. Pylori infection
Methods for diagnosing infection can be divided into invasive and non-invasive.
Invasive techniques:
- histological method;
- helpil test (rapid urease analysis);
- bacteriological method;
- cytological method - examination of smears;
- molecular genetic method (PCR in material taken from a biopsy).
Non-invasive techniques:
- serological method - blood testing for antibodies to a microorganism;
- enzyme immunoassay of feces (for the presence of a specific antigen);
- polymerase chain reaction for analysis of nucleotide sequences of microbes in feces;
- urease breath test with 13.14C-urea;
- ammonia breath test (helic test).
A common disadvantage of all invasive techniques is the need for endoscopic examination, which is not indicated in all cases, and sometimes is even contraindicated. The histological and cytological methods have absolute specificity (no false positive result), but not the highest sensitivity (probability of a true negative result), since the microbe may not be present in the biological material being studied. The results of bacteriological research (culture on a nutrient medium) also have high specificity and make it possible to check the sensitivity of a microorganism to antibiotics, however, the sensitivity of this method is even lower, since the microorganism requires special conditions for collecting transportation, the presence of nutrient media and specially trained personnel, which makes this method very expensive.
The most widely used in our country is the rapid urease helpil test, carried out during an endoscopic examination. According to the provisions of the Maastricht Agreement V on the diagnosis of H. Pylori infection, it must be performed during endoscopy and there are no contraindications to biopsy. In the case of a positive test, to clarify the nature of the mucosal lesion, it is necessary to take a biopsy from the antrum and body of the stomach, which is extremely rarely performed in our practical medicine. At the same time, the helpy test performed during endoscopic examination is not recommended for monitoring after treatment, since in these cases it is not informative (has low specificity and sensitivity. The serological method is based on the detection of antibodies to the microorganism in the blood, and has a sufficiently high sensitivity for primary diagnosis However, it is not suitable for monitoring the effectiveness of treatment, since a high level of antibodies can remain for a long period after treatment. In addition, the information content of the method depends on the presence of a particular antigen in the structure of the microorganism, which may not be found in all strains.
In practice, we often encounter patients whose infection was diagnosed incorrectly due to specialists’ ignorance of the applicability of the methods, which gives rise to the false opinion that it is impossible to cure the infection not only among ordinary people, but also among practitioners.
Serological testing of stool for antigen to H. Pylori is highly informative, but depends on the type of microorganism circulating in the region; the polymerase chain reaction method for identifying the nucleotide sequences of the microorganism has demonstrated many false-positive results in a number of observations and is currently not recommended for use.
The rapid urease helix test, which is widespread in our country, is based on recording an increase in the concentration of ammonia in exhaled air in the presence of urease activity of Helicobacter; however, for a number of reasons, in a number of randomized clinical trials it has demonstrated insufficient sensitivity and specificity (probability of true positive and true negative result) and is not currently recommended for diagnosing infection.
According to the first provision of the international recommendations for the diagnosis of H. Pylori (Maastricht V), the 13,14C-urease breath test is the most studied and recommended non-invasive method in the “test and treat” strategy. And according to the 10th provision of the same agreement, this study is the best option for confirming the eradication (successful treatment) of H. Pylori. The technique is actively used in developed countries, but has not yet become widespread in Russia due to the lack of gas analyzers for assessing 13СО2.
The Clinic's doctors specialize in the diagnosis and treatment of H. Pylori - associated diseases, and the hospital's arsenal includes the most modern diagnostic techniques in accordance with international standards, including the 13C breath test. You can get advice on optimal diagnosis and treatment by making an appointment with a specialist. Taking a breath test is possible without first consulting a doctor and is indicated if relatives have H. Pylori-associated diseases or are suspected of having H. Pylori infection. If the test is positive, you will be able to receive treatment recommendations from your doctor.
It is based on the change in the concentration of 13CO2 in the patient’s exhaled air 30 minutes after taking 13C-Urea compared to the baseline concentration of 13CO2 (before taking the test solution). The non-radioactive and stable isotope 13C is used as a label. Carbamide (urea) labeled with this isotope decomposes in the human stomach exclusively under the action of urease, an enzyme that is a waste product of H. Pylori. 13CO2 enters the lungs through the bloodstream, from where it is evacuated with exhaled air. The concentration of 13CO2 directly depends on the number of Helicobacter pylori bacteria in the patient’s gastric epithelium.
Features of the 13C Urea test in the diagnosis of H. pylori infection.
- Lack of radioactivity, can be used by any person, including pregnant women and small children.
- It is a priority method for diagnosing HP in the most advanced and technologically developed countries.
- Highest accuracy, sensitivity and specificity, minimizing the possibility of obtaining false positive and false negative results.
- Non-invasiveness of the technique (no need for endoscopic examination).
- The test method is simple and fast, with a guaranteed test result within three minutes after the end of the testing procedure.
Treatment and prevention of Helicobacter pylori
Treatment of this bacterium involves a complex of therapies and antibiotics.
Treatment of this dangerous bacterium involves a whole range of therapies and antibiotics. Treatment methods for Helicobacter pylori are often the subject of active debate among doctors, since the bacterium is very resistant to the effects of various drugs. For example, if a person has previously taken a certain type of antibiotic, it will probably no longer be effective against the bacteria.
In addition, there is always a great risk of using antibiotics to destroy beneficial microflora in the body, which is quite difficult to restore, and a person’s allergic reaction will be aggravated. Antacids are used to treat Helicobacteriosis.
These substances inhibit the production of gastric juice, but they cannot completely destroy the bacteria. Most of all, doctors around the world are concerned about how highly resistant the bacteria is not only to an acidic environment, but also to all kinds of antibiotics. It is very difficult to cure the disease thoroughly. In most cases, the course of treatment destroys most of the bacteria and, thus, the person is not in danger. But all the diseases that Helicobacter pylori causes, as practice shows, still return over time. Therefore, it takes many years to take medications to completely defeat this disgusting bacterium.
In the fight against Helicobacter pylori, the correct approach to treatment is important; it must be comprehensive. In addition to taking antibiotics or decoctions and traditional medicine, you also need to eat right. The components of traditional medicine should eliminate the cause of the disease, but the selection of ingredients for decoctions should depend on the acidity characteristics in the stomach of a particular person. That is, the selection is carried out individually. Such folk remedies include the following:
Main stages in the study of H. Pylori infection
- 1906, U. Krieiutz first described spiral-shaped bacteria in patients with gastric cancer;
- 1915, E. Rosenow, A. Sanford discovered similar bacteria in patients with ulcerative lesions of the stomach and duodenum;
- 1924, J. Luck, T. Seth demonstrated in their works the presence of urease activity in the human stomach and put forward a hypothesis about its connection with 12-gut ulcer;
- 1923, 1947, G. Konjetzny, based on morphological and clinical data, made an assumption about the inflammatory nature of peptic ulcer and stomach cancer;
- In the second half of the last century, many clinicians in a number of studies noted the positive effect of antibacterial therapy on the healing of peptic ulcers.
- 1984 The Lancet published the results of a study on isolated spiral-shaped bacteria, mainly from the antrum of the stomach and from the area of gastric metaplasia of the duodenal epithelium (Marshall BJ, Warren JR), and subsequently in 2001 they received the Nobel Prize for achievements in the field of medicine for this discovery and physiology.
- 1985 Marshall B, according to Koch's postulates, self-infected himself as part of an experiment to confirm the infectious nature of chronic gastritis.
- 1985-1994, major studies were carried out that established H. Pylori infection as the most important etiopathogenetic factor of chronic gastritis (type B), duodenitis (gastroduodenitis), gastric ulcer and 12-gut ulcer, MALT lymphoma (mucosal-accociated lymphoid tissue) and adenocacinomas of the stomach;
- 1994, experts from the WHO International Agency for Research on Cancer classified H. Pylori as a class 1 carcinogen;
- 1994, the US National Institutes of Health first adopted guidelines for the treatment of H. Pylori-associated peptic ulcer disease;
- 1996-2015, 1-5 Maastricht consensus on the diagnosis and treatment of H. Pylori-associated diseases;
- 2014 Kyoto Consensus, the main provision of which was not only the recognition of H. Pylori-associated gastritis as an infectious disease, but also recommendations for the treatment of all persons infected with this microorganism.
Author of the article: Tryapitsyn Alexander Valerievich (gastroenterologist, candidate of medical sciences)