Acute pain and discomfort in the stomach are common, and such symptoms affect the general condition of the patient. Often, stomach pain is accompanied by nausea, belching, and heaviness. These signs may be permanent, which indicates a chronic process in the body. Let's look at the causes of stomach pain and discomfort and recommendations for eliminating them.
What kind of bacteria is this?
Helicobacter pylori - translated from Latin - is a spiral-shaped bacterium that lives in the pylorus. And indeed the microscopic bacterium looks like a spiral surrounded by hairs. With the help of these hairs - flagella, it quickly moves through the internal organs to its place of permanent residence - the pylorus - the lower tier of the stomach and the initial section of the intestine - the duodenal bulb. The Helicobacter bacterium has refuted the myth that hydrochloric acid in the stomach kills all microbes. On the contrary, the little predator feels at home in destructive acid, thanks to the enzyme urease, which breaks down hydrochloric acid.
How does Helicobacter affect the stomach? Destroys parietal (parietal) cells of the mucous (inner) lining of the stomach, releasing toxic products - toxins. Protective blood cells - neutrophils, lymphocytes and others - pursue the pest, trying to destroy both it and the altered parietal cells - inflammation occurs. The amount of protective mucus in the area where the bacterium resides is noticeably reduced, and hydrochloric acid rapidly affects the altered area, exacerbating the constant inflammation of the mucous membrane. This is manifested by pain in the stomach “in the pit of the stomach,” heartburn, belching, coating on the tongue, bad breath, constant nausea, that is, symptoms of chronic gastritis. Chronic long-term inflammation of the gastric mucosa leads to changes in its cells, including the development of stomach cancer.
How does Helicobacter enter the body? Since Helicobacter lives in the stomach, infection is possible when the bacteria enters the human body through the mouth. This is the habit of taking food or dishes with unwashed hands, and the desire to try food on someone else’s plate or take a bite from an apple or a friend’s sandwich when offered to try - this is how children often become infected. In addition, you can become infected by sharing utensils or through kissing, which is why Helicobacter is often found among members of the same family.
So why now go to a cafe with your own dishes? Fortunately, Helicobacter is not a resistant bacterium and washing dishes in the dishwasher is enough to destroy them. Good restaurants and cafes are of course equipped with such machines, and you can visit them without the risk of infection.
Main stages in the study of H. Pylori infection
- 1906, U. Krieiutz first described spiral-shaped bacteria in patients with gastric cancer;
- 1915, E. Rosenow, A. Sanford discovered similar bacteria in patients with ulcerative lesions of the stomach and duodenum;
- 1924, J. Luck, T. Seth demonstrated in their works the presence of urease activity in the human stomach and put forward a hypothesis about its connection with 12-gut ulcer;
- 1923, 1947, G. Konjetzny, based on morphological and clinical data, made an assumption about the inflammatory nature of peptic ulcer and stomach cancer;
- In the second half of the last century, many clinicians in a number of studies noted the positive effect of antibacterial therapy on the healing of peptic ulcers.
- 1984 The Lancet published the results of a study on isolated spiral-shaped bacteria, mainly from the antrum of the stomach and from the area of gastric metaplasia of the duodenal epithelium (Marshall BJ, Warren JR), and subsequently in 2001 they received the Nobel Prize for achievements in the field of medicine for this discovery and physiology.
- 1985 Marshall B, according to Koch's postulates, self-infected himself as part of an experiment to confirm the infectious nature of chronic gastritis.
- 1985-1994, major studies were carried out that established H. Pylori infection as the most important etiopathogenetic factor of chronic gastritis (type B), duodenitis (gastroduodenitis), gastric ulcer and 12-gut ulcer, MALT lymphoma (mucosal-accociated lymphoid tissue) and adenocacinomas of the stomach;
- 1994, experts from the WHO International Agency for Research on Cancer classified H. Pylori as a class 1 carcinogen;
- 1994, the US National Institutes of Health first adopted guidelines for the treatment of H. Pylori-associated peptic ulcer disease;
- 1996-2015, 1-5 Maastricht consensus on the diagnosis and treatment of H. Pylori-associated diseases;
- 2014 Kyoto Consensus, the main provision of which was not only the recognition of H. Pylori-associated gastritis as an infectious disease, but also recommendations for the treatment of all persons infected with this microorganism.
Author of the article: Tryapitsyn Alexander Valerievich (gastroenterologist, candidate of medical sciences)
How do I know if I have Helicobacter pylori infection?
The presence of insidious bacteria in the body can be detected in different ways. First of all, this is a histological method, when during FGDS (fibrogastroduodenoscopy) - an examination of the stomach, which can be carried out in Chelyabinsk at the All Medicine Clinic - cells of the gastric mucosa are taken for examination. Not only the bacterium Helicobacter pylori is detected, but the condition of the inner lining of the stomach is also assessed - the severity of inflammation and the degree of change in mucosal cells against the background of inflammation. The following methods are breath tests. Helicobacter produces the enzyme urease, which is capable of decomposing urea to form ammonia and carbon dioxide. The essence of the methods is to determine either the composition of carbon dioxide in the patient’s exhaled air (urease breath test) or ammonia (Helic test). The Helic test is quite widely used, especially in pediatric practice, as a simple, non-invasive diagnostic method for the patient. Another common diagnostic method is the detection of specific antibodies of class G immunoglobulins - IgG in the patient’s blood. Helicobacter pylori infection is accompanied by the development of an immune response - the production of antibodies, of which IgG occurs in 95-100% of cases. This is a reliable diagnostic method that allows you to assess the degree of Helicobacter contamination, but not the best way to control the treatment of Helicobacter pylori infection, since the level of IgG antibodies can remain high after the complete death of the microorganism for a long time - 1-1.5 years. In this case, if an antibody test is nevertheless performed, a decrease in their level is assessed no earlier than 2-3 months after the end of treatment. More often, to monitor the effectiveness of treatment for Helicobacter pylori infection, a stool test is performed. It is based on the detection of Helicobacter DNA in feces and is qualitative - it shows whether Helicobacter is detected or not, without assessing the degree of contamination. The method can also be used to diagnose the presence of infection before treatment, for example, in children, as it is simple and painless.
Preparing and conducting analysis
Stool analysis is included in the list of laboratory tests, the purpose of which is aimed at searching for causative agents of various diseases. Thanks to this analysis, pathogenic microorganisms in the gastrointestinal tract are easily identified. To get a more accurate result, you need to properly prepare for the analysis.
It is very important not to take antibacterial or laxative medications a week before the test, and you should also refrain from rectal suppositories. Any medication taken must be agreed with your doctor.
To collect stool, it is important to use a special sterile container (sold in a pharmacy). If you are unable to go to the toilet, you should not use laxatives or do an enema. This can significantly affect the analysis results. The collected material can be stored in the refrigerator for no more than 11 hours, but it is better that it gets into laboratory conditions within five hours.
In the laboratory, the obtained material is studied using the polymerase chain reaction, which refers to molecular genetic diagnostics. Thanks to this technique, even the smallest fragments of parasite DNA can be detected. It is very important that the study is carried out under appropriate conditions and the correct temperature.
I have been diagnosed with Helicobacter pylori – what should I do?
If a positive test for Helicobacter pylori is detected, you should consult a gastroenterologist or therapist. Antibiotics are used to treat infection, and only a doctor prescribes them.
Is it possible to cure Helicobacter by taking the drug de-nol, as shown in advertising, or with folk remedies? You can completely get rid of Helicobacter pylori infection only with certain antibiotics.
Do I need to treat myself with antibiotics if nothing bothers me and the test result for Helicobacter is positive? The infection may not bother you, in 70% of cases this happens, gastritis proceeds “silently” for years, but after a few years, due to low-grade inflammation, atrophy of the mucous membrane occurs and its transition to stomach cancer cannot be ruled out. In each specific case, the decision to carry out treatment is made by the attending physician.
Helicobacter pylori infection is very common among the population, is there any point in treatment if you can become infected again later? Yes, re-infection is possible, but it does not happen often - approximately 6 people out of 100 treated people acquire the infection again if the rules of prevention are not followed. They are very simple - wash your hands before eating, don’t try other people’s food, don’t eat in dubious eateries where you can’t be sure of the correct handling of the dishes, don’t kiss people you’re not very close to. It is also important, when a Helicobacter pylori infection is detected, to test all family members for it, starting from adolescence, and ideally, to treat all infected people at the same time. Children, if nothing bothers them, are treated from adolescence - from 12-13 years. If a child complains of abdominal pain or nausea, then examination and treatment are carried out according to indications at an earlier age.
People very often complain about exacerbation of gastritis. But in many cases it can be cured by getting rid of the bacteria that caused the inflammation of the stomach. If the infection is left unattended, over time, gastritis will turn into atrophic. Then the patient will need to take a biopsy at least once a year in 5-7 places of the stomach in order not to miss cancer.
Gastric adenocarcinoma
Adenocarcinoma (stomach cancer) represents up to 95% of all malignant tumors of the stomach.
There are two histological subtypes with different epidemiological and prognostic characteristics:
- Intestinal type;
- Diffuse type.
Epidemiology
Currently, there is a worldwide trend of decreasing mortality from stomach cancer. However, despite this, GC is in 4th place in terms of incidence among all malignant neoplasms and in 2nd place among the leading causes of mortality from cancer (Parkin DM et al., 2001; Crew KD Neugut AI 2006). This is largely due to the fact that in the early stages the disease is asymptomatic, and the standard medical examination plan in healthcare institutions does not include either endoscopic diagnosis or testing for H. Pylori infection.
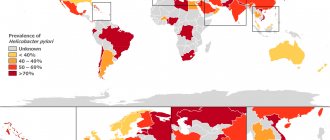
Countries with a high incidence of gastric cancer are simultaneously characterized by a similar level of H. Pylori prevalence in the population. At the same time, the decrease in the prevalence of infection in developed countries parallels the decrease in the incidence of stomach cancer (Crew KD Neugut AI 2006).
*NSAIDs - non-steroidal anti-inflammatory drugs; **ASA-acetylsalicylic acid.
Decoding the results
| Procedure | Confidence level of results | Decoding the research results |
| PCR | High | Positive—Helictobacter pyloriosis has been detected; negative - no type of Helicobacter pylori was detected |
| Bacteriological analysis for sensitivity to antibacterial drugs | Low – for antigen detection High - to determine sensitivity | The number of bacteria is 0 - the result is negative, no bacteria were detected; indicators greater than 0 - helictobacteriosis is determined; R—resistance to a specific antibiotic; I - moderate sensitivity to the antibiotic; S - high sensitivity to antibiotic |
| Immunological methods | Low | Positive—Helictobacter pyloriosis has been detected; negative - no pathogenic bacteria have been identified |