The article was prepared by a specialist for informational purposes only. We urge you not to self-medicate. When the first symptoms appear, consult a doctor.
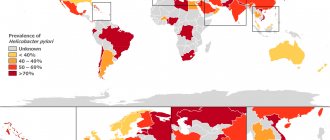
Timely identification and destruction of bacteria such as Helicobacter pylori in modern medicine is considered a priority in terms of preventing serious diseases of the digestive system (stomach cancer and gastric ulcers). The difficulty of diagnosis lies in the fact that in many regions of the country, non-invasive techniques to determine the fact of infection are simply not available to the population. While treatment without a diagnosis confirmed by laboratory methods is prescribed everywhere. This entails an unreasonable selection of antibacterial therapy and an increase in bacterial resistance to it. That is why a high-quality test for Helicobacter pylori is so important, allowing one to establish the presence of the bacterium in the human stomach.
A breath test for Helicobacter pylori is a non-invasive method for detecting infection in a person’s exhaled air. The study is carried out using a specialized respiratory test system. It is used for the initial detection of bacteria, to monitor the treatment and assess the degree of its effectiveness.
In general, the study comes down to taking the air that a person exhales into a test tube or tube. Samples are taken before and after taking the loading solution. Then the diagnostician evaluates the results and determines the degree of infection by the bacterium based on its urease activity. Therefore, this type of study is also called a urease breath test.
Indications for testing for Helicobacter pylori
The bacterium Helicobacter pylori is a gram-negative spiral-shaped pathogenic microorganism that inhabits the antrum of the stomach and intestines. The waste products of the bacteria lead to the fact that the mucous membrane of these organs of the digestive system will become inflamed, ulcers and erosions will appear on it. In the future, if left untreated, this will lead to the development of diseases such as gastritis, stomach ulcers and even stomach cancer. For the discovery of this bacterium, two scientists (Robin Warren and Barry Marshall) received the Nobel Prize.
Helicobacter pylori can be transmitted from one person to another by kissing or by using common household items. Therefore, the bacterium first enters the body most often in childhood. The acidic environment of the stomach is not capable of destroying the microorganism, since it has its own defense mechanisms against it.
Sometimes the disease begins to develop immediately after the infection has occurred, and sometimes after a certain time interval. Often, a bacterium can exist completely asymptomatically in the body for several years and manifests its activity only as a result of a combination of certain factors, for example, after suffering stress or against the background of a sharp decrease in immunity.
A test for the presence of Helicobacter pylori should be done for those people who have symptoms of disorders of the digestive system, including:
- Frequent belching.
- Heartburn with secretion of acidic contents.
- Hiccups.
- Bad breath due to the health of the oral cavity itself.
- Stomach pain, feeling of discomfort.
- Abnormal bowel movements, in which diarrhea may be replaced by constipation.
- Symptoms indicating a failure in metabolic processes: hair loss, dry skin, increased brittleness of nails.
- Rapid saturation with small portions of food, disturbances in its digestion.
- Meat intolerance.
If a person has any of the above symptoms, they should be tested for Helicobacter pylori. Also, all family members should be tested, provided that one of them was found to have this bacterium.
Which doctor should I contact?
If symptoms of Helicobacter pylori infection occur, it is recommended to consult a gastroenterologist. The doctor will not only prescribe all the necessary examination procedures, but will also draw up the correct course of therapy in the presence of pathologies or inflammatory processes in the digestive system.
If you have symptoms related to signs of Helictobacter pylori infection, a visit to a specialist cannot be postponed. The sooner the bacteria is identified, the easier and faster it will be to get rid of it.
The essence of the urease breath test for Helicobacter pylori
The breath test is based on the ability of bacteria to secrete a special enzyme - urease. It is necessary for Helicobacter pylori to prevent human gastric juice from destroying its lining.
In the stomach, urease breaks down urea into ammonia and carbon dioxide. The gas is released into the external environment. This is what the analyzer picks up.
There are several types of urease breath test for Helicobacter pylori, including:
- Breath urease test using isotope-labeled urea. In this case, during the procedure, the subject drinks a solution of urea, which was previously labeled with isotopes.
- 13C-urease breath test. In this case, urea labeled with the stable non-radioactive isotope C13 acts as a loading solution.
- Helic test. When conducting a helic test, they use not urea, but a urea solution.
Regardless of what type of examination is performed on the patient, they all have a high degree of accuracy.
The concept of "gold standard"
As mentioned above, you may hear from your doctor that the 13C breath test is a kind of “gold standard” in diagnosing Helicobacter pylori. Of course, for obvious reasons, domestic test kit manufacturers claim the same thing.
Indeed, European scientists studying Helicobacter pylori infection have organized a series of conferences with the participation of leading experts. Based on the standards of evidence-based medicine and a large number of controlled clinical trials, approaches to the diagnosis and treatment of Helicobacter pylori have been developed. The first conference was held in Maastricht (Netherlands) in 1996.
At the next conference, namely at Maastricht II, held in 2000, very optimistic recommendations were developed for the 13C breath test. The test has been presented as the best of the best for the primary diagnosis of helicobacteriosis, the so-called “gold standard”, with which others simply cannot stand comparison [5].
Almost 20 years have passed since then, and the concept of “gold standard” in relation to the 13C test has never been used again. Thus, at subsequent Maastricht conferences, the same scientists and doctors no longer put this method in first place among the others [6][7][8]. Firstly, this test is intended for primary diagnosis when endoscopy is not possible, and this happens extremely rarely. Secondly, even if it is the “gold standard”, it is exclusively for the control of eradication - the treatment of helicobacteriosis, but not for primary diagnosis [9]. However, in domestic sources the opinion of twenty years ago still prevails.
Preparation for the procedure
Before being tested for Helicobacter pylori, the patient must carry out a number of preparatory measures.
- The study is prescribed no earlier than 3-6 days after taking antibiotics or antisecretory drugs. Also, 5 days before the procedure, you should avoid taking painkillers, antacids and NSAIDs. If a person takes any medications on an ongoing basis, he should consult a doctor about this to clarify the possibility of the procedure.
- At least 3 days before the study, you will need to avoid drinking alcoholic beverages.
- The day before the procedure, you should not eat foods that increase gas formation. It is recommended to remove potatoes, bakery and confectionery products, cabbage, peas and beans from the menu.
- The evening before the test, you should have a light dinner. Meals should take place 2-3 hours before bedtime.
- At least 6 hours must pass between the study and the last meal. The procedure is performed on an empty stomach.
- It is forbidden to eat in the morning; you should refrain from using chewing gum.
- You are not allowed to smoke before the procedure. You need to give up tobacco 3-4 hours before the procedure.
- Before performing the test, you should brush your teeth and rinse your mouth.
- You can drink water for the last time an hour before the test, but its volume should not exceed 100 ml.
If you follow all the suggested recommendations, the test result will be as reliable as possible.
Stool analysis
PCR – what is it? This is a sensitive way to detect infection. It recognizes the DNA or RNA of the pathogen. For PCR, the material for research is feces.
A stool test for Helicobacter antigen is the most convenient test for the elderly, children and seriously ill patients. In this case, the presence of the patient in the laboratory is not required and the procedure is not associated with injury to the body. By the way, we will talk about Helicobacter pylori in children separately.
But detecting bacteria in stool is not easy. In the intestine, the microorganism is exposed to unfavorable conditions for it (bile acids, lack of oxygen). Therefore, active organisms adapt to new conditions, change their shape and their number sharply decreases.
A special method of polymerase chain reaction (PCR) is used, which allows you to determine the DNA fragment of a microorganism. The accuracy of the result is 95-96%.
What not to do before donating stool
It is important to know how to get tested for Helicobacter. Before donating stool, it is not recommended to take a lot of dietary fiber, coloring foods, inorganic salts, or medications that increase intestinal motility for 3-4 days.
Stool after an enema or laxative is not suitable for testing for Helicobacter.
A stool test for Helicobacter pylori is carried out before starting treatment. If the patient has previously taken antibiotic therapy for the treatment of any disease, it is better to prescribe a different method of examination.
Analysis transcript
The test result for helicobacter pylori can be positive or negative. A positive result indicates the presence or past infection. Negative data - about the absence of disease or incorrect conduct of the study.
How is the urease breath test performed with carbon-labeled urea?
The procedure begins with the patient being asked to breathe through a tube. It is located deep in his mouth, the oral cavity itself will be slightly open. You need to breathe calmly and smoothly. At this time, the doctor takes two air samples.
The patient is then asked to drink an isotope-labeled urea solution. After 15 minutes, another 4 air samples are taken. Care must be taken to ensure that the subject’s saliva does not enter the tube. To do this, he can remove it from time to time and smooth out the accumulated liquid. If it happens that saliva does get inside the sample, then the test should be stopped and repeated after an hour. Although modern devices make it possible to protect air samples from saliva.
Violation of gas removal
The intestines normally contain about a liter of gas. It is produced by bacteria and is gradually eliminated voluntarily or involuntarily. Bloating occurs when gas production increases or its elimination is impaired.
In some cases, gas accumulates in the intestines not because a lot of it is produced, but because it is not excreted. The act of releasing gases from the intestines is called "flatus". The lack of gas removal often indicates a serious pathology: intestinal obstruction. This indicates the need to consult a surgeon.
Intestinal obstruction can be obstructive and paralytic.
Obturation is a blockage of the intestines, gases do not come out due to an obstruction (tumor, bezoar). Paralytic obstruction occurs in the absence of peristalsis, that is, contraction and movement of the intestine.
How is the 13C-urease breath test performed?
It is the 13C-urease test that is the most commonly used test for identifying Helicobacter pylori. During the procedure, only two air samples are taken from the subject.
The first sample is obtained in the morning on an empty stomach, and the second sample is taken half an hour after taking a solution of urea labeled with the stable isotope C13. The person exhales air into disposable bags that are specially designed for this procedure.
This type of research has a number of advantages, including:
- The diagnostic accuracy is high, reaching 100%.
- The procedure is safe for health, since no radioactive substances are used during its implementation.
- The research doesn't take much time. In general, 40 minutes is enough to complete it.
Other ways to detect Helicobacter pylori infection
In addition to the 13 CT-urease test, there are alternative methods for diagnosing Helicobacter pylori in the lumen of the gastrointestinal tract. The preferred diagnostic method is selected individually by the attending physician. Alternatives to a breath test include:
- Endoscopic techniques. We are talking about performing esophagogastroduodenoscopy. This method allows you to visually assess the condition of the mucous membrane of the stomach or duodenum by inserting an endoscope tube. Using this method, it is possible to detect erosive and ulcerative changes in the mucous membrane, as well as take a biopsy for histological examination.
- Laboratory analysis of stool. This method is also informative, but in order to avoid errors, 1 week before collecting biomaterial, it is necessary to avoid taking antibiotics. The analysis also allows you to identify signs of dysbiosis.
- Laboratory analysis of venous blood. The purpose of this study is to search for antibodies to Helicobacter pylori.
How is the helic test performed to identify Helicobacter pylori?
The helic test is carried out according to the same scheme as the 13C-urease breath test. The only difference is that instead of isotope-labeled urea, a person receives a solution of urea. Air is taken in 2 samples: before taking the solution and after taking it.
The undoubted advantage of the study is its complete safety for human health. This is the best test for detecting Helicobacter pylori in pregnant women and children. However, a number of experts question the accuracy of the results obtained. Therefore, the helic test is carried out only in Russia.
References
- Ivashkin V.T., Maev I.V., Abdulganieva D.I., Alekseenko S.A., Ivashkina N.Yu., Korochanskaya N.V., Mammaev S.N., Poluektova E.A., Trukhmanov A. S., Uspensky Yu.P., Tsukanov V.V., Shifrin O.S., Zolnikova O.Yu., Ivashkin K.V., Lapina T.L., Maslennikov R.V., Ulyanin A.I. . Practical recommendations of the Scientific Community for Promoting the Clinical Study of the Human Microbiome (NSOM) and the Russian Gastroenterological Association (RGA) on the use of probiotics for the treatment and prevention of gastroenterological diseases in adults. Russian Journal of Gastroenterology, Hepatology, Coloproctology. 2020
- GuevaraB, CogdillAG. Helicobacter pylori: A Review of Current Diagnosticand ManagementStrategies. DigDisSci. 2020
- Choi IJ, Kim CG, Lee JY. Family History of Gastric Cancer and Helicobacter pylori Treatment. N Engl J Med. 2020
Interpretation of the results of a breath test for Helicobacter pylori
A breath test can give two results: positive or negative. The patient either has Helicobacter pylori in the body or has not been infected.
Also, using a special device called a mass spectrometer, the quantitative values of Helicobacter pylori in the body are determined.
The data obtained can be interpreted as follows:
- If the stabilized isotope in the exhaled air contains from 1 to 3.4%, then the degree of infection is mild.
- When the isotope concentration is in the range of 3.5-6.4%, they speak of an average degree of infection.
- Severe Helicobacter pylori infection will be indicated by rates of 6.5-9.4%.
- Extremely severe is indicated by values greater than 9.5%.
As a rule, the accuracy of the test is beyond doubt. It is possible to obtain a negative result only if the conditions for preparing for the study are not observed. Some drugs can reduce the activity of gastric juice production, which will make it impossible to break down urea.
Test results will be available 1-2 days after the test. The storage period for collected samples is 10 days, but no more.
Test kit
Basically, the test kit includes a breath sample container and a load. The load is urea (urea) in powder form, and this powder is dissolved in water, with or without the addition of citric acid. More on this later.
Some researchers recommend using a citric acid solution or citrus juice to dissolve the load to increase the accuracy of the test results. But here, too, doubts arise: researchers have not agreed on whether it is worth dissolving the load in these liquids or whether it is better for the patient to drink these liquids before the procedure [10]. Since there is no single methodology, the point is extremely controversial. Apparently, people conducting this testing are forced to rely only on their intuition.
How do Russian test kit manufacturers answer this question? Today, three manufacturers of this type of product are registered in Russia. The HELICARB set, produced by .
recommends using orange or grapefruit juice in the study, but does not indicate in the instructions that, according to scientists, these drinks should be used with caution when testing patients with diabetes. In addition, many people are allergic to citrus fruits, and even a small amount of such juice can cause a corresponding reaction. Let us also remember that citrus juice has an aggressive effect on the gastric mucosa due to its high acidity. And since the test is taken by people with diseases of this organ, and on an empty stomach, taking an acidic liquid can become unpleasant (and even painful) for the patient. It is sad that the specialists conducting the test are forced to choose between the convenience of the patient and the reliability of the result. Another manufacturer, the creator of the “13C-CARBAMIDE-TEST” kit, even suggests using citric acid in the study, the effect of which on the stomach is also aggressive [11].
Let's figure out what else it offers us.
Dose of 13C-urea: 50 mg.
What does the instructions for the test kit itself say?
It turns out that an adult will take a child’s dose of the drug? The composition, of course, is expensive, and, apparently, this was the reason for the calculation of the dosage by the Russian manufacturer, which distinguished itself with its 50 mg. In the USA and Europe, the minimum dose of urea for this test has been approved, namely 75 mg [13].
Even more suspicious is the manufacturer's attempt to explain its own choice of dosage. Again, let's look at his instructions. Highlight:
“In order to optimize the dose of 13C-urea during 13C-UDT, we carried out a study in 2015... 23 volunteers took part... studied on a Heli View mass spectrometer (South Korea)” [11].
When conducting the study, the manufacturer assumed that the resulting optimal dosage of labeled urea would be used to test thousands, if not millions, of people. But how optimal was the number of subjects? Let me remind you: 23 people.
When conducting such studies, as a rule, the minimum number of patients is 200 people. This can be seen in a number of foreign publications of this kind [14][15][16]. Typically, authors of publications indicate diagnostic methods, with the results of which the results of 13C-UDT are compared. does not do this in his manual.
By the way, samples from these volunteers were examined on a “Heli View” device (South Korea), which is not in the state register of Roszdravnadzor, which deprives the manufacturer of this study of any credibility.
The manufacturer also refers to a Swedish company that produces test kits with the same (50 mg) dosage. However, these tests are produced in the form of tablets, and this eliminates the loss of load on the oral cavity and esophagus, that is, hydrolysis of urea occurs exclusively in the stomach. According to the Swedish manufacturer, this helps minimize false positive results [12]. However, among foreign manufacturers, such a dosage and form of loading is rather an exception. Accordingly, comparison is unacceptable.
What to do if the test is positive?
If the test for Helicobacter pylori is positive, then the patient will need to undergo a comprehensive examination of the digestive system. The patient must be sent for an FGDS, which will provide information about the condition of the stomach and duodenum. He will also donate blood for biochemical and general analysis; other studies may be required.
Helicobacter pylori requires treatment. Depending on the severity and nature of the damage to the inner wall of the stomach, a therapeutic regimen is selected. However, to eliminate bacteria, antibiotics are always used, which are combined with proton pump inhibitors. In this case, two antibacterial drugs will be prescribed. This may be Amoxicillin, Levofloxacin, Metronidazole, Clarithromycin, etc.
During treatment or after its completion, the doctor may suggest that the patient take another test for Helicobacter pylori. This is required to monitor the effectiveness of ongoing therapy or to evaluate treatment already performed. A gastroenterologist treats diseases of the digestive system.
Contraindications
Absolute contraindications:
- Patients with lactose intolerance (intolerance to dairy products, most often in the form of loose stools)
- If there are episodes of a sharp decrease in blood glucose both on an empty stomach and after meals
- Existing fasting hypoglycemia (postprandial hypoglycemia)
- Use of laxatives, in particular lactulose, in the last 4 days
- X-ray examination of the intestine
Relative contraindications:
- use of antibiotics (last 4 weeks before the study)
- colonoscopy performed (during the last 4 weeks before the study)
- X-ray examination of the colon with barium, or irrigoscopy (in the last 4 weeks before the examination)
- X-ray examination of the small intestine (last 4 weeks before the examination)
- ileostomy (surgery on the small intestine in the form of removing part of it through an opening in the abdominal wall to the outside).
Measuring instruments
To determine the 13CO2/12CO2 ratio in selected samples, the following instruments are used:
- mass spectrometers;
- IR spectrometers;
- laser spectrometers.
Mass spectrometers are considered one of the most sensitive and accurate instruments for measuring the 13CO2/12CO2 ratio, however, due to complex maintenance and high prices, they are not used for mass diagnostics.
In this regard, fundamentally cheaper IR spectrometers are offered, for example, an IR spectrometer for breath tests with stable isotopes, approved for use in practical healthcare: “IRIS.Doc” (Kibion/Wagner, Sweden/Germany, Registration Certificate No. FSZ 2008/ 03312 dated December 22, 2008).
This device has been produced in the EU for a long time [17]; it was first registered in the Russian Federation in 2008. No changes have been made to the device since that time, as this would require changes to the marketing authorization. And from the changes in the registration certificate from Roszdravnadzor, one can see only a change in the name of the manufacturing organization and the address of the applicant organization of the medical device in 2015, as well as the OKP code to OKPD2 code in 2022 (however, this is due to changes in the classification system in the Russian Federation) [18 ]. The question is, how does a retro device from 2008 meet modern requirements?
There is also a Chinese device, from which you can learn about the calibration of any IR spectrometer.
The device manufacturer recommends calibration once a month. Apparently, it does not matter at all how many samples will be examined during this period of time. But this is not the worst thing.
The instructions say: "The operator blows into the sampling bag." It’s surprising, because usually special bags and cylinders with a gas mixture are used to calibrate such devices. Is it assumed that the operator, who is usually a nurse or laboratory assistant in a medical facility, has a ratio of gases in the exhalation as constant as in the mentioned cylinders and bags? So, while German instrument manufacturers supply special calibration bags filled with a gas mixture, in our country the exhalation of a nurse will be used as a standard. Interesting, isn't it? Will it be the same person who “breathes as a standard”? What if this particular nurse or laboratory technician gets sick and does not come to work on the day of calibration? What now, will another person calibrate (if, of course, such a term can be used in relation to this at all)?
Diagnosis of infection: symptoms and methods
It is necessary to be examined for the presence of Helicobacter pylori if problems occur in the digestive system:
- belching or heartburn;
- heaviness in the stomach;
- lack of appetite;
- pain in the epigastric region;
- unstable stool (diarrhea and constipation);
- general weakness because nutrients are not fully absorbed.
These symptoms are a good reason to visit a doctor. The presence of existing diseases (lymphoma, ulcer, gastritis) or stomach cancer in close relatives increases the risk of infection in the body.