Gastric hyperemia is characterized by reddened and swollen lesions on the mucous membrane of the organ. This disease is a consequence of overcrowding of blood vessels. A red gastric wall means the initial stage of development of the inflammatory process. Similar manifestations are often diagnosed with gastritis, peptic ulcers and other lesions of the gastrointestinal tract.
The gastric mucosa is hyperemic
Normally, the gastric mucosa has a light pink color, which becomes brighter closer to the pyloric region. In some patients they have a yellowish tint, which is not a pathology. During examination, the epithelium reflects the light of the endoscope, so it appears shiny. Numerous folds of the mucosa have a thickness of 6-10 mm. Their size gradually increases closer to the antrum. When air is introduced into the stomach cavity, the folds of the mucous membrane are smoothed out, and this allows you to examine the entire surface.
If the diagnostician notes that the gastric mucosa is hyperemic, what does this mean? External signs of hyperemia are redness and swelling of the folds of the stomach. The color change is due to blood flow.
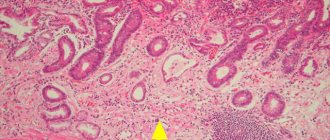
The mucous and submucosal layers of the wall have a branched capillary network, with numerous anastomoses between them. Therefore, an increase in blood inflow and a decrease in blood outflow causes the filling of capillaries, which shine through the epithelial layer, changing the color of the mucous membrane.
Diagnostic measures
If any suspicious symptoms appear (for example, nausea, bloating, heartburn, belching, pain), it is very important to visit a gastroenterologist in a timely manner. One of the main methods for studying the condition of the mucosa is a procedure called esophagogastroduodenoscopy. It is performed using an endoscope - a special probe with a camera at one end to view the internal state.
Using this method, you can accurately assess the condition of the body and the internal walls of the stomach, take a piece of tissue for analysis (biopsy), visualize the presence of a pathological process, and prescribe the correct course of therapy.
A competent specialist will easily determine the presence of pathology in hyperemic epithelium, since healthy tissue looks shiny and produces mucus normally. During the examination, when inflated with air, the folds are straightened, the surface is smooth, the epithelial cover is intact and clean, without wounds or ulcerations. The color is pink, there may be a yellowish coating.
As the disease develops, the symptoms worsen, redness of the epithelial layer appears, the folds increase, do not straighten when inflated, and swelling is observed.
Causes of hyperemia of the gastric mucosa
The reasons for changes in blood flow may be associated with neurohumoral regulation of the vascular bed, diseases of the heart, kidneys and other organs. In addition, hyperemia can also be physiological. For example, congestion of the stomach walls occurs during digestion, or when a heating pad is applied to the epigastric region.
Therefore, if we talk about what hyperemia of the gastric mucosa is, we need to take into account the physiological and pathological mechanisms of its development. For example, during an inflammatory reaction of the body, inflammatory mediators are released at the site, causing dilation of blood vessels, increasing blood flow to the affected tissues. This is a protective reaction in which tissue trophism and cell regeneration are enhanced.
First aid and prevention
As soon as discomfort in the gastrointestinal tract begins to bother you, you should immediately make an appointment with a doctor. Until then, here are a few tips to follow. The first tip is to take a horizontal position. This will reduce the pain a little. The second piece of advice is to take 1 tablet of No-Spa or any other antispasmodic. If severe pain bothers you, apply a heating pad to the stomach. There is a year inside it. The cold will reduce tension.
On a note!
It is strictly forbidden to apply heat to the stomach. This will only make the condition worse. There is a high risk of causing complications.
The doctor’s task is to eliminate risk factors that provoke an increase in blood flow to the vessels located near the gastric mucosa. If the patient has chronic diseases, then they should be treated. In other cases, preventive recommendations are targeted. A healthy person should avoid foods that irritate the mucous membrane:
- onion;
- radish;
- radish;
- horseradish;
- mustard;
- spices;
- spices.
Foods that cause constipation are prohibited. The more tension is required during defecation, the higher the risk of increased stress on the blood vessels. A mandatory rule is to refrain from self-administration of medications. Only a doctor can determine whether a particular medicine can be used or not. Some medications are not compatible at all, so you should not risk your health. Other recommendations:
- those with a sweet tooth should moderate their appetite;
- quitting tobacco and alcohol;
- Minimize the consumption of canned food.
Refusal of products containing a large amount of dyes.
Inflammation of the antrum
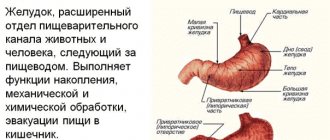
The human stomach consists of 3 sections: upper; middle (organ body); antrum, or antrum (lower section). The antrum is responsible for the production of 3 important substances: bicarbonates, which alkalize it for the smooth passage of food into the intestines; mucus, which protects the stomach from being corroded by hydrochloric acid; the hormone gastrin, which is responsible for the production of hydrochloric acid. Antrum gastritis - what is it? This is a chronic inflammation of the antrum and a violation of all its functions.
The occurrence of type B gastritis (an alternative name for the disease) is possible with untreated acute or catarrhal gastritis. Consequences of chronic inflammation: the normal functioning of the gastrointestinal glands is disrupted; hyperplasia of the gastric mucosa occurs; acidity increases; scars appear on the mucous membrane, which is a sign of antrum atrophy; the passage connecting the stomach with the intestines narrows; the passage of food into the duodenum becomes difficult; the risk of developing esophageal diseases increases.
Causes of acute gastritis
This disease appears suddenly. In rare cases, the cause may be the bacteria Helicobacter pylori entering the body. But usually it does not make itself felt instantly, but is the causative agent of sluggish chronic gastritis.
It is usually not difficult for an adult to determine the cause. It is enough to analyze what he ate and drank several hours before the attack. Inflammation can be caused by:
Infections can also cause an attack. Among the most likely, gastroenterologists identify cytomegaloverus, syphilis, and staphylococcus infection. People with weakened immune systems are more likely to become infected. Another reason for the development of an acute inflammatory process is exposure to bile. This only applies to type C gastritis.
Classification of mucosal hyperemia
Physiological and protective reactions of the body are carried out by regulating vascular tone by the nervous system or bioactive substances. That is, this is active plethora. If there is a disturbance in the outflow of blood, for example, an increase in pressure in the vena cava system or fluid retention in the body due to kidney disease, gastric hyperemia occurs passively.
In both cases, the liquid component of the blood leaks into the tissue, causing swelling. At first, this does not cause serious changes, but if this condition persists for a long time, the metabolism in the cells is disrupted, which makes them vulnerable to the aggressive effects of digestive juices.
There are two types of hyperemia:
- Active . In most cases, it is useful, as it promotes the restoration of damaged cells, for example, when the mucous membrane is exposed to unfavorable factors (malnutrition, pathogenic microflora). But with progression and long-term existence, blood clots form in full-blooded vessels, causing damage and death of epithelial cells.
- Passive . Impaired outflow has an adverse effect on the mucous membrane. Hypoxia and thrombosis cause a decrease in the protective properties of cells, fluid retention in the intercellular space, and swelling.
Based on localization, diffuse and focal hyperemia of the gastric mucosa is distinguished. During FGDS, the diagnostician also indicates the location of the lesion.
Causes in adults, children
Hyperemia of the mucous membranes (catarrh) in children and adults occurs as a result of various reasons. In this case, characteristic clinical signs appear, with which it is important to contact the hospital in a timely manner.
Causes of catarrhal inflammation and hyperemia of the mucous membrane:
| Name | Description |
| Children |
|
| Adults |
|
In old age, the mucous membranes of old people become inflamed, since over time the epithelium wears out and its functional abilities decrease.
There are also numerous provoking factors that contribute to the development of pathological processes:
- allergic reaction;
Tests for allergens in adults are carried out when the causative agent is unknown - treatment with certain medications;
- weakness of the immune system;
- untimely treatment of certain diseases;
- unfavorable environmental conditions.
Genetic predisposition and autoimmune processes also contribute to damage to the mucous layer, even if there is no damage or disease to the epithelium.
Therapeutic measures
For people interested in how to restore the gastric mucosa, it is important to know that when this disease is diagnosed, in most cases no treatment is prescribed, since it is believed that the body independently fights the problem through self-regeneration. During this process, accelerated metabolism occurs, which causes the process of tissue self-healing to enter an active stage.
This condition is a positive phenomenon in the development of arterial hyperemia. In some cases, doctors create an additional flow of blood fluid to stimulate regenerative processes and speed up recovery. If you are interested in how to restore the gastric mucosa in case of other pathologies, you need to contact your doctor with this question.
Treatment of the syndrome
Diet as one of the treatment methods
If a person has been diagnosed with this, it will be necessary to follow all the doctor’s recommendations so that the disease does not progress to a more severe stage, which is not only problematic, but sometimes impossible to treat. Treatment will be as follows:
- Eating only healthy foods
- Avoiding fatty and spicy foods
- Following a special diet
- Taking sedatives that primarily affect the nervous system. And as mentioned above, stress is one of the most common causes of the problem.
- Taking antacids, which will not only reduce the activity of gastric juice and reduce pain that occurs immediately after eating
- Taking activated carbon or decoctions made according to folk recipes in order to reduce gas formation
- Taking medications that will stimulate peristalsis
- Taking enzymes to help digest food better
Maintaining proper nutrition plays a big role in the treatment of irritable stomach syndrome, because if this is not done, then medications are unlikely to have a positive effect and relieve at least pain.
Symptoms
Any type of hyperemia leads to a decrease in barrier function, inflammation, and corresponding symptoms. Patients complain of pain, burning in the epigastric region, and indigestion. As the disease progresses, heartburn, nausea, and vomiting may appear.
If hyperemia of the inner layer of the stomach is caused by somatic diseases (heart disease, kidney disease), the patient may experience:
- swelling;
- high blood pressure;
- difficulty urinating;
- drowsiness, etc.
In such situations, additional examination is required. Hyperemia is often observed in patients with unstable mental health and under stressful conditions.
Diseases due to gastric hyperemia
In gastroenterology, mucosal hyperemia is associated with stomach diseases such as gastritis and peptic ulcers. In various forms of gastritis, in addition to focal hyperemia, the following signs are observed:
- Spicy . It is characterized by severe hyperemia and swelling of the folds, petechiae, erosions, and copious amounts of thick mucus.
- Chronic . The mucous membrane is pale, dull, grayish in color. Sometimes there are thinned areas (atrophy) with translucent vessels. This is the so-called false hyperemia.
- Superficial gastritis is characterized by diffuse hyperemia, the formation of foamy white mucus, swelling of the folds that do not level out when inflated. Submucosal hemorrhages are sometimes observed.
- Hypertrophic gastritis is characterized by thickening and pronounced diffuse hyperemia of the folds; they acquire a cherry color. Proliferative processes (nodules, warts) are revealed on the surface.
Hyperemia is also present in other forms of gastritis (phlegmonous, necrotic), as well as ulcers. It indicates an inflammatory process. When infected with Helicobacter Pylori, hyperemic manifestations are more pronounced.
Diagnostic methods
Hyperemic changes can only be diagnosed using endoscopy. For diagnosis, fibrogastroduodenoscopy or endoscopic video capsule is used. ultrasound , radiography , CT , MRI visually determine the appearance of the inner layer only indirectly, by identifying swelling of the mucous membrane.
Types of gastritis
The largest division of gastritis is acute and chronic. The first occurs immediately after irritating factors come into contact with the gastric mucosa. In case of improper nutrition, it manifests itself in a catarrhal form, in case of poisoning or infection - in a fibrinous form.
Chronic is often caused by the bacterium Helicobacter pylori. The disease is characterized by a sluggish course with periodic exacerbations. Based on the localization of the inflammatory process, the following forms are distinguished:
- antrum - in the lower part of the stomach;
- fundal - in the middle section (sometimes extends to the bottom of the organ);
- reflux gastritis - in the area of the pylorus of the stomach.
The chronic type of the disease is characterized by dysfunction of gastric secretion. Its excessive activity causes increased acidity (this form is called hyperacid). With secretory insufficiency, acidity is reduced (this form is called anacid).
Diagnostics
Having looked at the statistics, we can conclude that almost 90% of people need consultation with a gastroenterologist. To make a correct diagnosis, a specialist prescribes an examination, which is divided into laboratory and instrumental diagnostics.
Laboratory methods include: studies of gastric juice, blood, urine and feces. With their help, you can determine the secretory function, bacterial composition of the gastrointestinal tract, enzyme activity and other important functions. But without instrumental methods, the analysis results are uninformative.
Laboratory methods include: studies of gastric juice, blood, urine and feces. With their help, you can determine the secretory function, bacterial composition of the gastrointestinal tract, enzyme activity and other important functions. But without instrumental methods, the analysis results are uninformative.
- gastroscopy or esophagogastroduodenoscopy (EGDS) is a type of examination that is carried out using special equipment (gastroscope) with a flexible hose, equipped with viewing optics and a camera. Contraindications for manipulation are: heart disease, hypertension, mental disorders, severe respiratory failure. Before performing the procedure, the patient must refuse to eat food no earlier than 8 hours, and water 3 hours before, not take medications, smoke, or even brush their teeth;
- Symptoms of hyperemia of the gastric mucosa The gastric mucosa is focally hyperemic, there is a coating with whitish foamy mucus on the surfaces of the organ in “mucus lakes”, the folds are compacted and are not completely smoothed out with the help of air.
- As cells die, the surface becomes thinner and turns pale. In this case, the foci of the disease do not become hyperemic, and the vascular web is clearly visible.
- In the superficial form of gastritis, the mucous surface of the stomach is hyperemic throughout or only in the body and antrum of the stomach. Sometimes hyperemia is focal in nature or can be diffuse.
- If there is fibrous gastritis, hyperemia is most pronounced, while it is focal and characterized by the presence of pus. This inflammation can be caused by measles or scarlet fever infection. The patient may vomit blood frequently.
- The phlegmous form of the disease can be triggered by trauma to the stomach with sharp objects, such as fish bones. In such cases, this indicates possible hyperemic foci.
- Bulbit is characterized by swelling and redness, thickening of folds in the antrum. Among the reasons are Helicobacter pylori infection of the antrum of the stomach and unhealthy diet.
- Renal dysfunction (various degrees of swelling).
- Depression and permanent stress also provoke hyperemia.
To detect the disease - even if there are almost no problems with the stomach - make an appointment with a gastroenterologist. Gastroscopy is an excellent diagnostic option. Diagnostics involves a procedure carried out by a probe, camera and inspection optics. Using this method, you can assess the condition of organs, take a tissue biopsy, find out the diagnosis and prescribe therapy.
A gastroenterologist will help diagnose the problem. He first examines the patient and collects anamnesis.
After a medical examination, a gastroscopy is performed. It is performed using a special device - an endoscope. It is equipped with viewing optics and a camera.
This diagnosis is an unpleasant and painful procedure, but it allows you to accurately determine the condition of the organ, identify the causes of hyperemia, thanks to which the doctor prescribes the appropriate treatment tactics. In addition, using this method, a biopsy is performed, i.e., tissue is taken for examination.
For preventive purposes, as well as at the slightest suspicion of gastrointestinal diseases, you should seek help from a gastroenterologist. The most accurate and reliable research method is gastroscopy. This procedure involves attaching a camera and optics to the probe, as well as the use of other auxiliary instruments that are inserted deep into the esophagus and stomach.
Gastroscopy allows you to accurately determine the condition of the internal organs of the gastrointestinal tract, identify pathological changes and, if necessary, take a tissue sample for further study.
A doctor can easily notice pathological changes in the epithelium, since in a healthy state they are characterized by transparent mucus, as well as a shiny pink surface. Diagnosis is made on an empty stomach, which allows you to notice the slightest changes not only in the epithelium itself, but also in its thickness.
Gastric hyperemia is characterized by redness of the mucous membrane and indicates the onset of the development of many gastrointestinal diseases. Early diagnosis allows you to determine the cause of its development, as well as eliminate it as quickly and effectively as possible.
Reasons for the development of the pathological condition
Hyperemia of the gastric mucosa occurs in the following diseases.
Reflux esophagitis
A chronic disease of the esophagus, which is characterized by inflammation of its mucous membrane due to the constant reflux of stomach contents into it. Sometimes, when the disease occurs, the pain radiates to the sternum and resembles symptoms of heart disease.
Often, patients mistake pain for angina pectoris, without even thinking about digestive problems. The main signs of pathology include: belching of air or food, nausea, severe heartburn, sour taste in the mouth, regurgitation, prolonged hiccups. The chronic form of esophagitis is characterized by alternating periods of exacerbation and remission.
Gastritis
Inflammation of the gastric mucosa and its dystrophic changes. The form of the disease is determined by the location and nature of the redness and swelling: if the gastric mucosa is moderately hyperemic and there is a slight whitish coating, then we can talk about minor inflammation.
If the redness is severe, the mucous membrane is thinned and blood vessels are visible, then atrophic gastritis is diagnosed. Focal hyperemia is observed during purulent-inflammatory processes, characterizing the fibrous form. If the gastric mucosa is diffusely hyperemic, then perhaps we are talking about superficial gastritis.
..
The clinical picture of the disease includes the following symptoms: pain and a feeling of fullness in the epigastric region, nausea and vomiting, increased salivation, decreased or loss of appetite, frequent belching, bloating, weight loss. The chronic form of gastritis does not have pronounced symptoms, but is characterized by periodic exacerbations with disruption of the gastrointestinal tract.
Peptic ulcer
A pathology characterized by damage to the gastric mucosa and the formation of ulcers in it. Signs of the disease can be different and are related to the size and location of the defects, pain threshold, stage of the disease, age of the patient, etc.: pain that can occur on an empty stomach and go away after eating, and vice versa, heartburn, belching sour or bitter, a feeling of heaviness in the stomach, rapid satiety, flatulence, decreased or loss of appetite.
Of all the pathologies of the stomach, peptic ulcer is the most insidious and can be accompanied by a number of complications. These include penetration, perforation, malignancy, pyloric stenosis and bleeding.
Bulbit
A disease in which there is redness and swelling of the mucous membrane of the bulbar part of the duodenum. The disease can be asymptomatic or have a pronounced acute period. The main signs of bulbitis are:
Stomach problems
- bitter taste in the mouth;
- minor pain in the upper left abdomen;
- attacks of nausea and vomiting;
- often constipation.
In addition, other unpleasant symptoms may appear, such as a whitish coating on the tongue, increased gas formation, cramping abdominal pain on an empty stomach or after eating. If the pathology is not treated in any way, then there is a likely risk of developing gastrointestinal bleeding.
Duodenitis
An inflammatory disease characterized by an inflammatory process in the duodenum. Often the disease is combined with gastritis, which most often affects the antrum of the stomach.
Characteristic signs of pathology are:
- epigastric pain that increases with palpation of the abdomen;
- constant nausea;
- rarely vomiting mixed with bile;
- rumbling in the stomach;
- flatulence;
- loss of appetite and weight loss.
When bile stagnates, yellowness of the skin and sclera of the eyes may appear. In elderly people, duodenitis is often asymptomatic and is diagnosed accidentally during an FGDS. But there are also factors due to which the gastric mucosa is hyperemic:
- mechanical damage to the digestive organ by any object;
- irrational and unhealthy diet;
- infectious diseases (measles, scarlet fever);
- bacterial infection (Helicobacter pylori);
- renal failure;
- prolonged exposure to stress and depression.
Remember! If you experience any discomfort behind the sternum or in the upper abdomen, as well as nausea and vomiting, you should seek help from a specialist as soon as possible.
Treatment methods
Since the gastric mucosa can become hyperemic for various reasons, this means that drug treatment is not always required. Sometimes it is enough to eliminate the impact of adverse factors on the body.
Treatment is carried out in accordance with the diagnosis. Appointed:
The patient must be prescribed dietary nutrition.
Treatment of acidity disorders
If there are signs of low acidity, replacement therapy with enzyme preparations is prescribed. Its main task is to normalize the production of pepsin. Preparations containing acedin-pepsin help with this. Drug stimulation of gastric juice secretion is also necessary.
If the diagnostic results reveal increased acidity, the patient is prescribed antacids. They neutralize acid, weaken the activity of pepsin, and in some cases have an enveloping effect. To eliminate symptoms, medications are recommended that stimulate gastrointestinal motility and relieve spasms of smooth muscles. Additionally, you can use folk remedies - herbs, flax seeds, potato juice.
Clinical manifestations
Patients whose gastric mucosa is severely hyperemic rarely realize this. Some symptoms may not be related to the gastrointestinal tract at all. At the initial stage, the heart rate increases. Drowsiness or problems with urination appear. Depending on where the foci of severe hyperemia are localized, the patient experiences:
- fatigue;
- obesity;
- swelling of the face.
Recommendations for nutrition in pathology
If hyperemic mucosa is detected, the patient is advised to follow a diet. Substances that irritate the mucous membrane should be excluded from the diet: spicy, salty, sour, fatty foods, smoked meats and marinades, alcohol, strong coffee. Fried foods are not recommended. For heat treatment, food should be boiled or steamed.
In the diet you can use:
- chicken, rabbit, turkey, veal, low-fat sea fish;
- a small amount of vegetable fats;
- skim milk, cottage cheese;
- non-acidic fruits and vegetables;
- cereals (rice, oatmeal, buckwheat);
- eggs, no more than 1 per day;
- wheat bread 1-2 grades, crackers.
Meals should be fractional (5-6 times a day), small portions. It is also necessary to observe the temperature regime; the dishes should not be too hot or cold. The optimal temperature is between 15 and 60 degrees Celsius.
How to treat
Arterial hyperemia is not treated in 85% of cases. In such a situation, intensive blood supply to tissues begins as a consequence of independent regeneration of damage. The cells of the stomach receive the necessary amount of oxygen and nutritional components, due to which metabolic processes are accelerated. As a result, cells begin to divide rapidly, and healthy tissues replace damaged structures. In the arterial form of the pathology, doctors only prescribe proper nutrition and help balance the diet.
In the remaining 25% of cases, active hyperemia, as well as venous blood filling, indicate the presence of gastritis. In case of inflammation of the mucous membrane, complex treatment is carried out. The patient must follow a strict diet, take antibiotics to suppress the growth of Helicobacter pylori and other medications to accelerate tissue regeneration. You are allowed to drink herbal infusions and eat honey.
Preventive measures
Since gastritis is now diagnosed not only in adults, but also in children, prevention should begin as early as possible. First of all, you should normalize your diet:
When the first symptoms of inflammation of the gastric mucosa appear, it is important to minimize (or better yet eliminate) the consumption of chocolate, coffee, spicy and fried foods.
Gastroenterologists recommend regularly checking for parasitic infestations. When they are detected, it is important to carry out timely treatment, because they often attack the digestive system.
Possible complications and prognosis
Prolonged irritation and damage to the mucosa are harbingers of gastritis. If you do not pay attention to this in time, plethora leads to the development of microthrombosis, hypoxia and the progression of damage to epithelial cells.
If hyperemia is detected, the patient should be observed by a doctor to avoid the development of chronic gastritis and peptic ulcer. With adequate treatment, the prognosis is favorable, since normally the surface epithelial layer is renewed every 7–10 days.
What does the result mean?
A comprehensive diagnosis and the results obtained are necessary for the attending physician to determine the cause of inflammation and create the most correct treatment regimen.
Considering the results obtained, there are the following degrees of development of catarrhal inflammation:
| Name | Description |
| Moderately hyperemic mucosa | Inflammation provokes swelling of the epithelium and the formation of foamy plaque on the top layer. Uneven damage to the mucous membrane occurs. This is a mild form of inflammation. |
| The mucous membrane is focally hyperemic | The inflammatory process develops on a separate part of the mucous epithelium. |
| Diffusely hyperemic mucosa | Pathological processes affect all layers of the mucous membrane. |
An incorrect diagnosis will lead to the progression of pathological processes, which increases the risk of serious complications.
Forecast
A favorable prognosis is possible only with timely treatment of the pathology. Treatment of the disease is complicated by the characteristics of its causative agent, the bacterium Helicobacter pylori. This microorganism is capable of temporarily stopping its vital activity and going into “sleep mode”. When a provoking factor occurs, activity resumes.
Therapy must be carried out fully. If you stop treatment early, the risk of complications will increase. Hypertension can cause peptic ulcers, large-scale atrophy of the mucous membranes of the digestive tract, and the formation of malignant tumors.
Sources
https://gastrosapiens.ru/zheludok/zabolevaniya-zh/ochagovyj-antralnyj-gastrit.html https://gastroved.com/ochagovyy-antralnyy-gastrit-lechenie.html https://ogastritah.ru/vidy/chto- takoe-ochagovyj-antralnyj-gastrit-i-kak-lechit-eto-zabolevanie.html https://gastrocure.net/bolezni/gastrit/antralnyj-gastrit.html https://medicalok.ru/zheludok/gastrit/antralnyj. html https://gastrotract.ru/bolezn/gastrit/antralnyj-gastrit.html https://zheludokok.ru/gastrit/antralnyj-gastrit-poverhnostnyj-i-ochagovyj.html https://zhkt.expert/gastrit/kak -raspoznat-ochagovyj-antralnyj-gastrit.html https://ogastrite.ru/lechenie-gastrita/ochagovyj-antralnyj-gastrit-prichiny-simptomy-diagnostika-lechenie/ https://gastrit.guru/lechenie/antralnyj-gastrit. html https://vseprogastrit.ru/gastrit/vidy-gastritov/antralnyjj-gastrit/
What do moist integuments look like under normal conditions and with hyperemia?
The mucous membrane is a specific part of the human body's immune system.
Sufficient moisture allows the epithelium to perform its protective functions. A dry mucous membrane is more susceptible to external negative factors and easily allows pathogenic microorganisms to pass through.
Prevention measures
To avoid irritation and inflammatory plethora of the mucous membrane, doctors recommend adhering to the following preventive measures:
- stop smoking;
- limit the intake of alcohol-containing drinks and strong coffee;
- Healthy food;
- avoid stress;
- See a doctor on time and treat chronic somatic diseases.
It is also necessary to exercise and not overwork. This will help boost immunity and ensure protection and rapid restoration of the mucous membrane.