Causes in adults
The etiology of the syndrome is varied. Experts combine them into several groups. Causes of hepatosplenomegaly in adults:
- Infectious diseases, including liver: acute hepatitis, malaria, rubella, schistosomiasis, infectious mononucleosis, cytomegalovirus infection.
- Blood diseases: myeloproliferative tumors, lymphoma, leukemia, pernicious anemia.
- Chronic liver diseases: cirrhosis, fatty degeneration.
- Other metabolic diseases: amyloidosis, Niemann-Pick disease, sarcoidosis, Gaucher disease, hemochromatosis.
- Autoimmune processes: systemic lupus erythematosus.
- Diseases of the cardiovascular system leading to stagnation of venous blood in the vena cava system.
In each case of illness, it is necessary to understand what is happening to the health of an adult: this involves conducting a set of additional examinations. In addition, hepatosplenomegaly in a child is possible.
Cirrhosis of the liver
Preparation for liver ultrasound
As a routine procedure, it is advisable to carry out an ultrasound of the liver after preparation, which consists of abstaining from food for 8-10 hours and preventing intestinal flatulence. Ultrasound of the liver is optimally performed on an empty stomach after an 8-10 hour fast. To ensure such an 8-10 hour period of fasting, you should subtract these 8-10 hours from the time for which the liver ultrasound is scheduled, and from this calculated moment you should not eat. It is acceptable to perform an ultrasound of the liver after at least a 6-hour fast. If the study is carried out not in the morning, but in the afternoon or evening, then in order to avoid too long a fasting period, on the day of the study you can eat dried white bread (crackers without additives, salt, flavor enhancers, flavorings, seasonings, etc.) and drink unsweetened tea .
To eliminate and prevent flatulence, it is necessary for two to three days before the study to stop consuming foods that promote increased gas formation in the intestines, such as carbonated water, whipped cream, nuts, pasta, honey, mustard, fatty meats and fish, alcohol. , vegetables (cabbage, radish, onion, garlic, bell pepper, etc.), fruits (melon, bananas, sweet apples, etc.), brown bread, dairy products, legumes (peas, beans, lentils, etc.) and other types of food containing large amounts of fiber. During the day before the study, you must also stop drinking plant juices.
If a person suffers from diseases of the intestines or other organs of the digestive system, then to exclude flatulence, in preparation for an ultrasound scan of the liver, in addition to following a diet, it is recommended to take medications for two to three days before the study that eliminate excess gas formation in the intestines (Carbolen 3 – 9 tablets per day and enzyme agents (Creon, Panzinorm, Mezim, etc.) 3 – 6 tablets per day). In addition to Carbolen and enzyme preparations, to prepare for an ultrasound of the liver in order to eliminate gas formation in the intestines, you can also take products with simethicone (Espumizan, Disflatil, etc.) 2 capsules 3 times a day, or activated carbon 2 tablets 3 times a day. Products containing simethicone and activated carbon to eliminate flatulence are taken for 2 to 3 days before an ultrasound scan of the liver.
Since an ultrasound of the liver is optimally carried out against the background of a non-bloated and empty bowel, then on the evening before the examination you need to drink a mild laxative (for example, Duphalac, Mucofalk) or in the morning on the day of the ultrasound, give an enema or use glycerin suppositories. When an ultrasound of the liver needs to be performed in emergency, it is done without any preliminary preparation. But if inaccurate data were obtained during an emergency ultrasound, then after some time the study should be repeated as planned with the necessary preliminary preparation.
You need to take paper napkins, toilet paper or a towel with you to the clinic, which can be used to wipe off the gel from the abdomen, which is applied to improve the quality of the image obtained on the monitor of the ultrasound machine. In addition, if hunger is poorly tolerated by a person, then you can take a packed ration with you to have breakfast immediately after the ultrasound. If a person is constantly taking any medications, then there is no need to stop them before performing an ultrasound of the liver. In children, preparation for an ultrasound of the liver consists of abstaining from eating and drinking any food (including water) for three hours before the test. Of course, such preparation of children is carried out only in cases where they can easily tolerate fasting and lack of water.
What diseases occur in children?
Hepatosplenomegaly can be observed both in newborns and at older ages. This condition in a child may have various reasons, both those listed above and additional ones: among the latter, the doctor will assume that it is:
- Hematological diseases: sickle cell anemia, thalassemia (detected during the first screening of the baby).
- Infectious processes in the child’s body: syphilis, tuberculosis.
- Developmental anomalies: biliary tract.
Moderate hepatosplenomegaly in a child may accompany physiological jaundice. Does not require special treatment. It is enough to follow the pediatrician’s recommendations for managing a baby with physiological jaundice: drinking water, walking, sunbathing. Depending on the cause in the child, the pathology may be present for a long time, and rapid regression of hepatosplenomegaly is possible.
How is a liver ultrasound performed?
An ultrasound of the liver is performed in a specially equipped room, in which an ultrasound machine, a couch and curtains are installed. For the examination, the patient must expose his stomach by removing or lifting up his upper part of clothing, and then sit on the couch in the position indicated by the doctor. Typically, an ultrasound of the liver is performed in the supine position, less often - lying on the left side. In some cases, when the patient cannot lie on his back or left side, an ultrasound of the liver is performed in a standing or sitting position.
After taking the required position, the doctor applies a special gel to the skin of the abdomen, which is necessary to obtain the best quality image. Next, the doctor moves the ultrasound machine sensor over the surface of the abdomen, obtaining an image of the liver from different angles, which is necessary for a detailed study of the condition of all parts and departments of the organ. During the examination, the doctor will definitely ask the patient to breathe at a normal rhythm, and also to inhale and exhale as much as possible. Images of the liver in different phases of breathing and against the background of different intensities of respiratory movements allow us to obtain the most detailed information about the state of the organ and its structures. In addition, during the ultrasound examination, the doctor may ask you to take a certain position, which is also necessary for a comprehensive assessment of the condition of the liver or identification of identified pathological changes. After completing the study of the condition of the liver and taking all the necessary measurements, the ultrasound examination is considered complete.
The doctor removes the sensor from the surface of the abdomen, and the patient can get dressed and leave. The procedure for ultrasound examination of the liver is usually short and takes 10 - 20 minutes, depending on the qualifications of the doctor, the type of ultrasound machine and the patient’s body weight. The thinner the patient, the faster the doctor can assess all parameters of the liver’s condition. In obese patients, on the contrary, the examination may be longer, since the subcutaneous fat layer makes it difficult to visualize the organ and forces one to examine the same area several times. After completing the ultrasound examination, the doctor writes a protocol with a mandatory conclusion, which he gives to the patient.
Signs of moderate enlargement of the liver and spleen
Moderate hepatosplenomegaly will have the following characteristics:
- Patient complaints: pain in the hypochondrium, abdominal discomfort, increased gas formation, increased abdominal volume. There may be an increase in temperature and clinical signs of the underlying disease.
- Examination of the patient reveals visual enlargement of the abdomen, sometimes asymmetrical.
- Palpation of the abdomen reveals an increased size of the liver and a change in the nature of its edge. In a healthy state, you can also feel the edge of the liver, while it is located close to the costal arch. In a healthy person it is sharp and even. Also, with an enlarged spleen, its edge is palpated, which is impossible to do in a healthy person.
- A general blood test can show an acceleration of ESR, a change in the ratio of the main blood elements.
- Ultrasound examination of the abdominal organs.
- CT and MRI.
Moderate hepatosplenomegaly in adults can resolve on its own if the cause is infectious diseases.
Ultrasound of the abdominal cavity and retroperitoneal space
What is ultrasound of the abdominal cavity and retroperitoneal space? Modern ultrasound technology (ultrasound) allows us to assess with high diagnostic accuracy the shape, size and location of the abdominal organs (liver, gall bladder, pancreas, spleen, etc.) and identify focal formations in them (liver cancer, pancreas cancer, tumor metastases , abscesses, cysts, hematomas, adenomas, etc.), assess the density and structure of the parenchyma of the liver and pancreas in case of diffuse damage, diagnose even small amounts (100-200 ml) of free fluid in the abdominal cavity, identify stones in the biliary tract , identify changes in large vessels, bile ducts, etc. In recent years, ultrasound has been widely used in the clinic as a method to help select the optimal access for performing liver puncture biopsy, abdominal drainage and other manipulations. Fatty liver degeneration (fatty hepatosis) . The main echographic sign of fatty liver is an increase in the echostructure of the liver in the form of a uniform increase in the number and size of echo signals. This is due to the deposition of fat in the liver lobules, the distance between which and their sizes increase so much that ultrasonic waves are reflected from them. Important but less specific signs include an enlarged liver, an increase in the inferior angle of the left lobe greater than 45°, and a clear outline of the liver and the inability to identify the portal vein. The echographic picture of fatty liver depends on the degree of involvement of liver cells in the process. At the first stage of the disease, the liver is slightly enlarged, the edge is rounded. The echostructure has a variegated pattern, the parenchyma is unevenly compacted into small focal areas. This is the so-called “islet” type of liver damage, which also occurs with hepatitis. At the second stage, the liver is much larger, the lower edge is rounded, the structure of the parenchyma is finely focal, the liver is diffusely and evenly compacted. In the third stage of the disease, the liver is of significant size due to the increase in both lobes. It has a round shape. The structure of the parenchyma is high density (echogenicity), portal vessels are not coded. Cirrhosis of the liver. There are direct and indirect echographic signs of liver cirrhosis. The diagnosis of liver cirrhosis is considered reliable if an ultrasound examination reveals 3 direct or 2 direct and 2 indirect signs of the disease. In most cases, the size of the liver is increased, often predominantly due to the left lobe of the liver. In the final stage of the disease, with a predominance of atrophic processes, the size of the organ decreases. Characterized by significant rounding of the lower edge of the liver and unevenness of its contours. The echostructure of the liver is significantly enhanced due to the appearance of more frequent and larger echo signals, which is associated with a significant restructuring of the architectonics of the liver, characteristic of cirrhosis. During the atrophic stage, the number and size of echo signals decrease. Finally, important signs of cirrhosis are a decrease in the elasticity and sound conductivity of the liver. Indirect echographic signs of cirrhosis are associated primarily with the development of portal hypertension syndrome. Dilation of the splenic vein more than 10 mm and the portal vein more than 15 mm are considered reliable signs of increased pressure in the v. system. porta. An increase in the size of the spleen and an increase in its echostructure are observed in 60-70% of cases of liver cirrhosis, although this sign is not specific only to portal hypertension. Ascitic fluid in the abdominal cavity during ultrasound examination looks like an echo-negative structure that accumulates in the lateral parts of the abdomen, in the pelvis, or (with small amounts of fluid) located around the liver. In these cases, it is advisable to study while changing the patient’s body position (lying and standing). "Congested" liver. In all cases of congestive circulatory failure, an increase in the size of the liver and rounding of its edges are noted. A pathological sign of a “congestive” liver is the expansion of the inferior vena cava and hepatic veins, the branching of the hepatic veins at an angle close to 90°. It is characteristic that the inferior vena cava loses the ability to change its diameter during breathing: it does not narrow at all during inhalation or narrows very little. Focal changes in the liver Ultrasound examination of the liver with focal changes in the liver is more informative than with diffuse lesions. In this case, there is a local decrease or increase in the echostructure, a diffuse or focal increase in the size of the liver and unevenness of its contour with the appearance of a bulge. Volumetric focal processes in the liver can cause compression of the bile ducts with the occurrence of obstructive jaundice. The most common sign of focal changes in the liver is a violation of the normal echostructure of the liver. There are several types of focal disturbances of the echostructure: Foci without echostructure (liver cysts, hematoma, liver abscess, necrotic tumors). Foci with reduced echostructure (metastases of poorly differentiated cancer, sarcoma, malignant lymphoma, hepatocellular cancer, adenoma, hemangioma, abscess, hematoma, etc.). Foci with enhanced echostructure (metastases of highly differentiated cancer, hepatoma, adenoma, hemangioma, scars, foci of calcification). The “target” symptom is a decrease in the echostructure along the periphery of the lesion and its intensification in the center (malignant liver tumor). Thus, the information content of ultrasound examination of the liver is quite high, especially in case of focal lesions of the organ. However, possible false positive and false negative conclusions should be taken into account. Therefore, when analyzing and interpreting study results, it is necessary to take into account the clinical picture of the disease as a whole, as well as data from other laboratory and instrumental research methods. It is important to know: A normal ultrasound picture, including the sagittal dimensions of the liver along the midclavicular line, not exceeding 12-15 cm, does not exclude the presence of a disease of this organ. Diffuse or focal changes in the echostructure of the liver reliably indicate its pathology. The ultrasound picture cannot reliably differentiate various forms of hepatitis, the initial stages of fatty degeneration and cirrhosis of the liver. With diffuse changes in the liver, the final diagnosis should be verified histologically. To clarify the diagnosis of focal changes in the liver, in most cases it is advisable to conduct a targeted biopsy under echographic control for subsequent cytological and histological analysis. Gallbladder and bile ducts Ultrasound examination of the gallbladder and bile ducts has certain advantages over x-ray examination (cholecystography, intravenous cholegraphy, etc.), since it completely eliminates radiation exposure to the patient, allows for examination in children and pregnant women, as well as with reduced liver and kidney functions. The most common indications for examination of the gallbladder and bile ducts are : acute and chronic cholecystitis; cholelithiasis; jaundice; tumor; dropsy and empyema of the gallbladder; condition after cholecystectomy or other operations on the biliary tract. When examining the gallbladder, its position, shape, size, respiratory mobility, condition of the external and internal contours, wall thickness, wall structure, additional inclusions in the gallbladder cavity, and the evacuation function of the organ are assessed. When examining the hepatic bile ducts, their position, diameter, condition of the walls, and the presence of additional inclusions in the lumen are determined. Normally, the gallbladder is detected as an echo-negative structure on the dorsal surface of the right lobe of the liver. The bottom of the gallbladder often protrudes from under the lower edge of the liver by 1.0-1.5 cm. Its length does not exceed 7-10 cm and width 3-4 cm. The gallbladder has an elongated pear-shaped, oval or round shape, clear and smooth contour. Intrahepatic bile ducts are not detected in a healthy person. The diameter of the common hepatic duct does not exceed 3-5 mm, and the common bile duct - 4-6 mm. Acute cholecystitis. Characteristic echographic signs of acute cholecystitis are thickening of the gallbladder wall by more than 4 mm. Its size may remain normal or even reduced, although a slight enlargement of the gallbladder is more common. The echostructure of the gallbladder, primarily its internal contour, is usually reduced. With phlegmonous cholecystitis, the internal and external contours of the bladder are unclear. When pericholecystitis is associated, the gallbladder wall has a double contour with an increase in the echostructure of the outer contour and a decrease in the echostructure of the inner contour. The appearance of a strip of fluid around the gallbladder indicates the presence of local peritonitis. Chronic (acalculous) cholecystitis. During the period of remission of chronic cholecystitis, the size of the gallbladder is reduced or normal. The most reliable signs are thickening of the bladder wall with simultaneous compaction (increased echostructure) and the presence of clear contours. This distinguishes the echographic picture from that of acute cholecystitis. The shape of the gallbladder often changes: bends, indentations of the walls and more pronounced deformation of its walls appear. At the same time, it should be remembered that the diagnosis of chronic cholecystitis cannot be made only on the basis of ultrasound results: mandatory clinical confirmation is necessary. Cholelithiasis. The problem of cholelithiasis (cholelithiasis) occupies a leading place in the pathology of the gallbladder. Ultrasound signs of gallbladder calculus are divided into direct and indirect. Direct signs include the presence in the lumen of the gallbladder against the background of an echo-negative bile structure of an enhanced echo signal corresponding to the location of the stone. The size of the signal is slightly smaller than the true size of the stone. When examining the patient in a horizontal position, the stones are located mainly on the dorsal surface and in the neck of the gallbladder. An important sign of calculus is the displacement of stones when changing body position. In a vertical position, the stones “roll” to the bottom of the gallbladder. The echo structure coming from a stone whose size exceeds 4 mm always forms behind itself a shadow path - an acoustic shadow resulting from the absorption of ultrasonic waves by the stone. One of the indirect signs of gallbladder calculosis is an increase in its size by more than 5 cm in diameter and up to 10 cm or more in length, as well as thickening of its wall and uneven contour. The echographic picture in the presence of stones in the hepatobiliary bile ducts resembles that of calculosis of the gallbladder. Stones larger than 3-4 mm in diameter give an amplified echo signal. If the diameter of the stone exceeds 5 mm, an acoustic shadow is determined behind its dorsal wall. Small stones are usually not detected by ultrasound. In these cases, an indirect sign of calculosis is the expansion of the duct proximal to the place of its obstruction. Differential diagnosis of mechanical and parenchymal jaundice. Echolocation turned out to be one of the most informative and valuable methods for the differential diagnosis of obstructive and parenchymal jaundice. It should be borne in mind that one of the main echographic signs of obstructive jaundice is dilation of the bile ducts. Differential diagnosis is based on the following principles. If the intrahepatic and extrahepatic ducts are not dilated and the size of the gallbladder is not increased, the obstructive cause of jaundice is in doubt. In these cases, it is most likely a consequence of diffuse liver damage (hepatitis, cirrhosis, etc.). If the intrahepatic ducts are significantly dilated, and the gallbladder and extrahepatic ducts are of normal size, the cause of jaundice should be considered in high obstruction, for example, at the level of the common hepatic duct. If the sizes of the extra- and intrahepatic bile ducts, as well as the gallbladder, are significantly increased, and these sizes do not change with the use of choleretic drugs, the most likely cause of jaundice is obstruction of the distal common bile duct (“impacted” stone, cancer of the sphincter of Oddi, carcinoma of the head of the pancreas glands, etc.). It should be borne in mind that compression of the common bile duct due to a tumor of the head of the pancreas is often accompanied by Courvoisier’s symptom (an increase in the size of the gallbladder against the background of obstructive jaundice). In the presence of a stone in the common bile duct, dilation of the ducts is determined, but the gallbladder is often not enlarged. Ultrasound examination of the pancreas Echography makes it possible to visualize the pancreas in different projections and assess its condition in the dynamics of the development of the pathological process, although due to the peculiarities of the anatomical structure and location of the pancreas, the study is associated with certain difficulties.
Indications for ultrasound examination of the pancreas are: any recurrent or long-lasting pain in the epigastric region; palpable formation in the epigastric region or pain on palpation; verified acute or chronic pancreatitis for the purpose of timely detection of complications (formation of cysts, abscess, necrosis); suspicion of a cyst, abscess, hematoma, pancreatic cancer; deformation of the posterior wall of the stomach during gastroscopy; change in the shape and contours of the duodenal loop during X-ray examination. Ultrasound examination of the pancreas begins with the patient in a horizontal position using sagittal scanning. The sensor is installed longitudinally in the epigastric region to the left of the midline. Examination of the pancreas is preceded by the identification of large vessels of the abdominal cavity - the aorta, inferior vena cava, splenic and portal veins, superior mesenteric arteries and vein, which serve as landmarks for finding the pancreas, as well as the celiac trunk. At the same time, the position of the vessels, their diameter, external and internal contours, pulsation, changes in diameter during inhalation and exhalation, and the presence of intraluminal inclusions are determined. The body of the pancreas is adjacent to the dorsal surface of the left lobe of the liver, and the head is adjacent to the duodenum. The pancreas is examined at the height of maximum inspiration, when the left lobe of the liver descends into the abdominal cavity. The study continues with a transverse position of the ultrasound sensor, which is gradually moved downwards until the splenic vein is visualized. With transverse scanning, it is often possible to visualize the entire pancreas. If necessary, research; They are also carried out in other positions: with the patient positioned on the right and left side, in an upright position. When examining the pancreas, its position relative to the “landmark vessels” and the spinal column is studied, the shape, contours and dimensions of the organ, the state of the pancreatic duct, the echostructure of the gland are determined, and the presence of focal changes in it is determined. The pancreas is located retroperitoneally across the posterior abdominal wall at the level of the I and II lumbar vertebrae. Although its shape can vary, the head is always the largest part of the gland. For practical purposes, it should be taken into account that the size of the head over 35 mm, body over 25 mm and tail over 30 mm reliably indicate an enlarged pancreas and associated pathology. Normally, the echostructure of the pancreas is similar in intensity to the echostructure of the liver. Small echo signals predominate, which are evenly distributed throughout the gland. With age, due to fibrotization and fat deposition, the echostructure of the pancreas intensifies. With various pathological processes in the gland, its echostructure changes significantly. Acute pancreatitis is characterized by a significant decrease due to swelling of the gland, and in chronic pancreatitis and cancer - intensification and heterogeneity (due to the development of fibrosis and scar changes). Normally, the diameter of the Wirsung duct does not exceed 1.5-2 mm. After intravenous administration of secretin, its diameter increases to 2.5-5 mm. In chronic pancreatitis, dilation of the pancreatic duct is often detected (up to 2.5-3.5 mm). After the administration of secretin, the diameter of its lumen almost does not change, which is an important diagnostic criterion for chronic pancreatitis. Spleen : the most appropriate ultrasound examination of this organ is if there are suspected malformations (complete absence, abnormal location, wandering spleen, change in shape, presence of accessory spleens), as well as for injuries to the spleen, which occur in 22% of cases of all injuries to the abdominal organs. In addition, enlargement of the spleen is diagnosed in case of inflammatory lesions and liver diseases, cysts, calcifications, infarctions, abscesses, tumors (hemangiomas, lymphangiomas, lymphomas, sarcomas, metastatic lesions), changes in systemic blood diseases (leukemia) are determined. Retroperitoneal space: assessment of lymph nodes. Vessels : assessment of the location of the main and intraorgan vessels, their sizes, the state of the lumen, the speed of blood flow in them.
How is the procedure for ultrasound of the abdominal cavity and retroperitoneal space performed? Research technique. Echography of the liver is usually carried out from subcostal and/or intercostal access in real time. The liver examination is carried out while holding the breath while inhaling, when the liver moves down slightly and becomes more accessible for visualization. For longitudinal scanning in the epigastric region, the sensor is placed 2 cm to the left of the anterior midline; for transverse scanning, the sensor is moved to the navel. The so-called “oblique” liver scanning technique is also used, when the ultrasound sensor is located parallel to the right costal arch and at an angle of 45° in the cranial direction, and other sensor positions. In this way, it will be possible to visualize the right and left lobes of the liver, the gallbladder, the common hepatic and common bile ducts, the anatomical structures that make up the hilum of the liver, and the head of the pancreas. The study ends with a scan of the abdominal cavity to detect free fluid.
How to prepare for an ultrasound of the abdominal cavity and retroperitoneal space? 3 days before the study, the patient is recommended to exclude from the diet milk, brown bread, fruits and vegetables, sweet juices and other foods that contribute to gas formation in the intestines. If you are prone to flatulence, enzyme preparations (festal, panzinorm, etc.) and adsorbents (activated carbon, chamomile paste, etc.) should be prescribed. The evening before the examination and in the morning immediately before the examination, two cleansing enemas are given. However, this procedure is not mandatory if the patient does not have flatulence. If emergency ultrasound examination is necessary, special preparation of the gastrointestinal tract is not carried out. It should be remembered that it is advisable to carry out an ultrasound examination of the abdominal organs no earlier than 2 days after an X-ray examination of the stomach with contrast or esophagogastroduodeposcopy and 3-5 days after laparoscopy or pyumoperitopeum.
What are the normal indicators (interpretation) of ultrasound of the abdominal organs and retroperitoneal space? Analysis and interpretation of research results Normal ultrasound picture of the liver In a healthy person, the sagittal dimensions of the liver along the midclavicular line are, on average, 10.5 ± 1.5 cm with fluctuations from 9 to 12 cm, and along the anterior midline - 8.3 +1.7 cm. The diameter of the liver is 20-22.5 cm. The lower angle of the liver, formed by the dorsal and ventral surfaces of the organ, is sharp: in the area of the left lobe it does not exceed 45°, and in the area of the right lobe - 75°. Normally, the contours of the liver are clear and even throughout almost its entire length. The liver has a homogeneous structure with a uniform distribution of signals of equal intensity and an image of echo structures (vessels, ligaments, ducts). The inferior vena cava is constantly located in the form of a ribbon-like echo-negative formation with a diameter of up to 15 mm. The portal vein, after its formation from the superior mesenteric and splenic veins, flows into the portals of the liver, which are located in the transverse and sagittal position of the probe. Viutripscheic ducts are normally difficult to trace, their lumen increases from the periphery to the gates of the liver. Unlike veins, intrahepatic ducts have no walls. Thus, a normal ultrasound picture of the liver is characterized by the presence of small, low-intensity, relatively far apart echo signals, resulting in echo-negative spaces remaining between them. The echohyals are homogeneous in size and evenly distributed throughout the liver. Portal vessels can be traced along the periphery of the liver; the echostructure of their walls is more pronounced than the echostructure of the surrounding liver parenchyma, the sound conductivity of the liver is completely preserved; sagittal size is 9-12 cm; the liver is elastic and has a smooth, clear contour. Diffuse liver diseases The most common diffuse liver lesions include hepatitis (acute and chronic), fatty degeneration and cirrhosis of the liver. The correct diagnosis by ultrasound depends on a number of objective and subjective reasons. The first of them include the type of device, its sensitivity, resolution, the presence of factors that worsen the image (obesity, gas formation in the intestines, etc.). The experience of the specialist and the thoroughness of the research are of great importance. The greatest difficulty is in the diagnosis of the early stages of fatty degeneration and cirrhosis of the liver. In acute and chronic hepatitis, the echographic picture is very nonspecific. Usually, the liver is enlarged due to one or both lobes and its edges are rounded. The echostructure is often normal and weakly echogenic. Only with a long course of the disease does the echostructure of the liver become “variegated” and alternating areas of weak and high echogenicity are observed. In some cases, in particular with the development of portal hypertension, an enlargement of the spleen and dilation of the splenic and portal veins can be detected.
Which doctors should I contact for consultation on ultrasound of the abdominal cavity and retroperitoneal space?
Gastroenterologist Ultrasound Doctor
Keywords diagnostics, ultrasound
Severe symptoms
Signs of hepatosplenomegaly in its severe stage will be slightly different from the moderate syndrome:
- an increase in the size of the abdomen, a significant enlargement of the liver makes it asymmetrical;
- change in the size of the liver and spleen, which is revealed by palpation;
- a blood test will reveal leukopenia, thrombocytopenia, erythrocytopenia, which is associated with their increased destruction in the spleen;
- increased liver transaminases, bilirubin;
- changes in biochemical blood parameters in the form of increased liver transaminases, bilirubin, alkaline phosphatase.
- changes on ultrasound, CT and MRI.
Sometimes the pathology does not make itself felt for a long time. The patient can walk with hepatosplenomegaly, which reaches a significant size. This is due to the lack of pain receptors in the liver tissue.
Normal liver ultrasound
Liver ultrasound indicators
During the ultrasound examination, it is necessary to determine the size and contours of the liver, assess the condition of the echo structure (homogeneous, heterogeneous), intrahepatic bile ducts, and large vessels. In addition, the presence of any inclusions and formations that are uncharacteristic of the normal echostructure of the liver is detected.
In more detail, based on the results of an ultrasound scan of the liver, the following parameters must be assessed:
- shape, contours and anatomical structure of the organ;
- the size of the entire liver and each of its lobes;
- structure and echogenicity of the liver;
- the state of the vascular pattern of the organ as a whole;
- assessment of the condition of large vessels and intrahepatic bile ducts;
- identification of focal changes and pathogenic formations;
- distinguishing various pathological changes from each other with the assumption of which pathological process is taking place in a particular case.
Normally, the main indicators assessed during ultrasound should be as follows:
- the angle of the lower edge of the left lobe of the liver is less than 45 o;
- the angle of the lower edge of the right lobe of the liver is less than 75 o;
- oblique vertical size of the right lobe of the liver – up to 150 mm;
- thickness of the right lobe of the liver – up to 140 mm;
- craniocaudal size of the left lobe of the liver – up to 100 mm;
- thickness of the left lobe of the liver – up to 80 mm;
- liver width – 230 – 270 mm (23 – 27 cm);
- liver length – 140 – 200 mm (14 – 20 cm);
- transverse size of the liver – 200 – 225 mm (20 – 22.5 cm);
- portal vein (measured at a distance of 20 mm from the confluence of the mesenteric and splenic veins) – 10 – 14 mm;
- hepatic veins (measured at a distance of 20 mm from the mouth) – 6 – 10 mm;
- inferior vena cava (measured at the level of the caudate lobe of the liver) – 15 – 25 mm;
- hepatic artery (measured at 20 mm from the porta hepatis) – 4 – 6 mm;
- lobar bile ducts – 2 – 3 mm;
- common bile (hepatic) duct – 4 – 6 mm;
- the edges of the liver are normally smooth and clear;
- the structure of the parenchyma is normally fine-grained, homogeneous, consisting of many evenly distributed small point and linear structures;
- echogenicity – normally the same or slightly higher than the echogenicity of the renal cortex;
- sound conductivity is normally high (deteriorates with diffuse changes in liver tissue, for example, with fibrosis, fatty inclusions with hepatosis, etc.).
Liver size by ultrasound
Normally, the total width of the liver is 23 - 27 cm, length - 14 - 20 cm, and diameter - 20 - 22.5 cm. The thickness of the left lobe of the liver should not exceed 8 cm, and the right lobe - 14 cm. If the size of the liver is increased, then such an enlargement of the organ is called hepatomegaly, which indicates pathology. It is possible to understand what kind of pathology we are talking about in a particular case by taking into account the results of other parameters of liver ultrasound.
Normal ultrasound picture of the liver
The echogenicity of the liver is normally uniform, and is somewhere between the echogenicity of the pancreas (which is higher) and the echogenicity of the spleen (which is lower). In addition, the echogenicity of the liver is normally the same as or slightly higher than the echogenicity of the renal cortex.
Echosigns
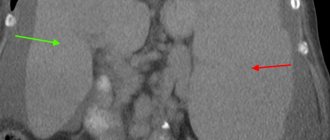
During an ultrasound examination, a specialist identifies echo signs of hepatosplenomegaly:
- increase in liver size;
- increase in the volume of the spleen;
- echogenic homogeneity of the liver tissue may indicate fatty degeneration;
- the presence of anechoic areas – cyst formation;
- rough structure – fibrous changes.
An experienced specialist can make a presumptive diagnosis as a result of ultrasound, but the final cause will only be determined by the treating gastroenterologist after a series of additional studies.
Interpretation of liver ultrasound
What do changes in various liver ultrasound parameters indicate?
Below we will look at which pathologies are characterized by changes in one or another ultrasound parameter of the liver. Increased size with a uniform fine-grained echostructure. When the liver is large, but its structure is normal and homogeneous, this may indicate the following pathologies:
- heart failure - in this case, additionally, ultrasound will reveal dilated hepatic veins, which are normally not visible. The diameter of the inferior vena cava does not change depending on inhalation and exhalation;
- acute hepatitis - usually no other specific changes other than an increase in the size of the organ are detected on ultrasound during acute hepatitis. The overall picture is quite normal;
- tropical hepatomegaly - additionally, ultrasound also reveals a significantly enlarged spleen (splenomegaly);
- schistosomiasis - in addition to an increase in the size of the liver, with this disease, ultrasound shows a thickening of the portal vein and its large branches, and their walls and surrounding tissue are very bright. In some cases, an enlarged splenic vein and the spleen itself are also visible. When infected with Schistosoma mansoni or Schistosoma japonicum, ultrasound may also show fibrosis of the tissue around the portal vein.
Increased size with a heterogeneous echostructure. An enlarged liver with a heterogeneous structure may indicate the following pathologies:
- if the liver is enlarged, has a heterogeneous structure, but no focal formations are identified in it, then this may be a sign of cirrhosis, chronic hepatitis or fatty hepatosis. With these pathologies, ultrasound, in addition to an increase in the size and heterogeneous structure of the liver, shows an increase in its echogenicity (hyperechoic parenchyma) and a decrease in the number of visible branches of the portal vein. In some cases, sound conductivity is significantly reduced, as a result of which the deep-lying parts of the liver are not visible at all;
- if the liver is enlarged, has a heterogeneous echogenic structure and multiple or single focal formations of any shape, size and echostructure are visible in it, then this is a sign of macronodular cirrhosis, abscesses, metastases, lymphoma or hematoma. In macronodular cirrhosis, an altered vascular pattern, normal stroma and numerous formations of different sizes are additionally visible on ultrasound. In case of abscesses, ultrasound additionally detects increased echogenicity and multiple or single formations with unclear contours are visible. With metastases, ultrasound additionally shows formations of various shapes, sizes and echostructures. In lymphoma, multiple hypoechoic (light-colored) structures with unclear contours and without distal acoustic enhancement are additionally visible. With hematomas, ultrasound shows formations with unclear contours and distal acoustic enhancement.
A decrease in liver size may be characteristic of micronodular cirrhosis. At the same time, ultrasound additionally records an increase in echogenicity and deformation of the organ due to scarring (overgrowth) of the portal and hepatic veins. In this case, the portal vein is usually normal or collapsed inside the liver and enlarged outside the liver. Sometimes numerous structures representing blood clots are visible inside the portal vein. Micronodular cirrhosis may be associated with ascites (fluid in the abdominal cavity), portal hypertension (increased pressure in the portal vein of the liver), dilatation and varicose veins of the splenic vein, and splenomegaly (enlarged spleen).
Cystic formations in the liver can be different, as they are provoked by different reasons.
Thus, in the liver, ultrasound may show a solitary cyst, which is an anechoic (light) round formation with clear or uneven contours and a diameter of less than 30 mm. Such cysts usually do not cause any clinical manifestations and are congenital, and therefore harmless. But, unfortunately, a solitary cyst cannot always be distinguished from a parasitic cyst, therefore, if such a formation is detected in the liver, it is recommended to perform a biopsy. Also, ultrasound can reveal multiple liver cysts, which usually look like anechoic (light) formations of various diameters with a clear contour and acoustic amplification. Typically, such multiple cysts are a manifestation of congenital polycystic disease, and are very often combined with cysts in the kidneys, spleen and pancreas. If the cysts become complicated, hemorrhages or suppuration occur in them, then on ultrasound such formations are visible as abscesses or disintegrating tumors. Finally, Some of the most difficult from a diagnostic point of view are parasitic (echinococcal) cysts, which are formed as a result of the penetration of parasites into the liver. Any parasitic cyst on ultrasound may have various echogenic signs, depending on the stage of development of the parasite and the condition of the cystic walls and cavities. Thus, a parasitic cyst may look like a simple light-colored formation with a clear contour and distal acoustic enhancement, similar to a solitary cyst.
In other cases, the cyst may have a double wall contour. In the third variants, “parasitic sand” or a septum is visible inside the cystic formation, freely moving in the cavity of the cyst. In fourth cases, multiple small cysts and blisters are visible inside the large cyst, which usually indicates the presence of a living parasite in the liver. When the parasite has already died, the cyst can acquire a clear outline due to calcification (calcification) of its walls. A single solid formation in the liver can be a hemangioma, abscess, festering cyst, metastasis, hepatoma. Unfortunately, it is very difficult to distinguish these formations based on ultrasound results, therefore, if a serious disease is suspected, a biopsy is recommended. Most often, single solid formations in the liver are represented by hemangiomas (up to 75% of cases).
How to treat this syndrome at home?
The patient's management tactics depend on the diseases that cause hepatosplenomegaly. That is, in each case of the disease etiotropic therapy should be carried out:
- viral infections – antiviral therapy;
- parasitic – antiparasitic drugs;
- cardiovascular diseases - treatment with diuretics, beta blockers, sartans, etc.;
- autoimmune lesions - the use of corticosteroid and immunomodulatory therapy;
- Oncological diseases of the blood - radiation therapy, chemotherapy.
Drugs for treatment are prescribed by specialists
. In addition, specialists, if necessary, prescribe symptomatic treatment:
- for spastic abdominal pain, antispasmodics are recommended: drotaverine, papaverine, platyphylline;
- to maintain liver function, hepatoprotectors are prescribed: Essentiale, Heptral, Karsil, Riboxin, etc.;
- pre- and probiotics: Hilak-forte, Bifiform, Bifidumbacterin, etc.
If an adult patient asks what hepatosplenomegaly is and how to treat it at home, then there is only one answer to this question: follow all the doctor’s recommendations!
What is liver ultrasound - a brief description
Ultrasound of the liver is a study of the organ using ultrasonic waves emitted and perceived by special devices called ultrasound scanners. The essence of the study is that an ultrasonic wave with an oscillation frequency of more than 20,000 Hz is capable of penetrating into tissues to a small depth, passing through them, and then part of the waves is absorbed by cells, and the other part is reflected with or without refraction. It is these reflected waves that come back to the ultrasound scanner sensor, are captured by it, converted into electrical impulses and create a picture on the monitor. The doctor sees on the monitor an image of the organ created by reflected and refracted ultrasonic waves passing through the thickness of the tissue.
To obtain an ultrasound image, the monitor uses a single sensor that simultaneously emits and detects ultrasound waves. To assess the condition of various organs, it is necessary to use sensors that emit waves of different frequencies, penetrating to different depths. To conduct an ultrasound of the liver, sensors with different frequencies of emitted ultrasonic waves are used, as this is necessary for the best visualization of the organ and the detection of its pathology.
Thus, currently for liver ultrasound they use 3.5 - 5 MHz sensors, which make it possible to see objects with a diameter of 1 - 3 mm. Sensors with a frequency of 3.5 MHz allow you to obtain images of tissues and organs located at a depth of 12 - 28 cm from the surface of the sensor. That is why such sensors (3.5 MHz) are used to examine adult patients of normal and obese physique. And sensors with a frequency of 5 MHz provide images of objects located at a depth of 4 - 15 cm from the sensor surface. Therefore, 5 MHz sensors are used to perform liver ultrasound in adolescents and thin patients.
The image obtained using reflected ultrasonic waves on the monitor allows you to evaluate the size, structure, location of the liver and its parts, identify the presence of various additional formations (cysts, tumors, etc.), inflammatory changes, etc. Based on the appearance, size, structure of the organ, the presence of inflammation or additional formations in the liver, as well as the condition of the surrounding tissues, lymphatic and blood vessels, the doctor can diagnose various pathologies, such as hepatitis, cirrhosis, hepatosis, cysts, hemangiomas, adenomas, cancer, liver metastases. Ultrasound of the liver is a painless, safe, not uncomfortable, but informative study that is easily tolerated by patients, since to carry it out the doctor does not have to insert any instruments into various parts of the body.
Since ultrasound is a safe, non-discomforting and well-tolerated examination method, it can be performed without any restrictions on pregnant women, children and the elderly. Liver ultrasound can be performed both to diagnose existing organ pathology and as one of the methods of preventive examination. For diagnostic purposes, liver ultrasound is prescribed when a person has any symptoms indicating liver pathology, such as pain in the epigastric region (in the middle of the abdomen, between the ribs), on the right or left under the ribs, yellowness of the skin or sclera of the eyes, unexplained itching of the skin, elevated body temperature, and high levels of amylase and bilirubin in the blood. In addition, to diagnose liver damage, ultrasound is prescribed when there has been an abdominal injury.
It is mandatory that an ultrasound of the liver is carried out at certain intervals for already identified liver diseases to assess the condition of the organ and monitor the course of the disease, as well as to determine the effectiveness of the therapy. As one of the methods of preventive examination, ultrasound is usually performed once a year. For preventive purposes, ultrasound is especially recommended for people who have a high risk of developing liver diseases, for example, due to alcohol abuse, taking toxic medications, etc.








![Rice. 1. Biopsychosocial model of the genesis of functional gastrointestinal diseases [1].](https://zakam.ru/wp-content/uploads/ris-1-biopsihosocialnaya-model-geneza-funkcionalnyh-zabolevanij-zhkt-1-330x140.jpg)