An ulcer is painful, disgusting and dangerous. In the recent past, doctors could not find the root cause of this pathology. They blamed it on stress, poor nutrition and treated it almost blindly experimentally.
At the end of the 19th century, German scientists discovered a spiral-shaped bacterium that lived in the stomach and duodenum. It was given the name Helicobacter pylori. In 1981, the connection between this microorganism and the appearance of ulcers in the stomach and intestines was scientifically proven, for which in 2005 the discoverers of the medical significance of the bacterium, Robin Warren and Barry Marshall, were awarded the Nobel Prize in Medicine.
What kind of bacteria is this? How to destroy a pathogenic microorganism and cure erosion of the gastric mucosa once and for all? How to treat Helicobacter pylori?
Helicobacter pylori: general information about the microorganism and route of infection
Helicobacter colonizes areas of the mucous membrane.
Helicobacter is a spiral-shaped gram-negative microorganism. Its dimensions are only 3 microns. This is the only microorganism capable of surviving and multiplying in the acidic environment of gastric juice.
Under favorable conditions, Helicobacter colonizes areas of the mucous membrane. The negative effect on the stomach occurs due to the complex properties of this microorganism:
- The presence of flagella allows for rapid movement in the mucous membrane of the gastrointestinal tract.
- Adhesion to stomach cells. This creates inflammation and the body's immune response.
- Produces enzymes that break down urea into ammonia. This neutralizes the hydrochloric acid in the gastric juice, and the bacterium receives an environment favorable for development. Ammonia additionally burns the mucous membranes. This causes an inflammatory process.
- The microorganism produces and releases exotoxins that destroy mucosal cells.
Scientists have proven that Helicobacter strains in patients with ulcers are more aggressive than in patients with gastritis and other inflammatory processes in the stomach or intestines.
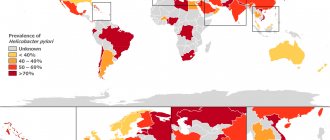
Infection with this microorganism occurs asymptomatically in 70% of cases. Doctors call possible routes of infection oral-fecal or oral-oral - through kissing, sharing utensils, in canteens and cafes, during medical procedures.
You have been diagnosed with a polyp in your stomach - what to do?
The detection of epithelial formations or “polyps” during gastroscopy is currently a common finding that worries patients with its unknown nature. There are polyps of the fundic glands, hyperplastic and adenomatous polyps. It is important that hyperplastic polyps larger than 1 cm and adenomatous ones have a high risk of malignancy. Therefore, correct assessment of size and making an accurate morphological diagnosis are especially important when detecting polyps in the upper gastrointestinal tract. A biopsy to clarify the type of formation is mandatory. It should be emphasized that polyps of the fundic glands and hyperplastic polyps less than 1 cm have a low risk of malignancy, however, if the endoscopist suspects their malignant nature, a biopsy is also performed without fail.
Helicobacter: diagnostic measures
To diagnose Helicobacter, you need to undergo tests.
Diagnostic procedures begin with interviewing and examining the patient. Then special studies are carried out to confirm or refute the preliminary diagnosis. Tests for Helicobacter pylori:
- Non-invasive procedures - blood for specific antibodies, breath test, stool and saliva analysis
- Invasive techniques - endoscopy with collection of material for histological examination
- To determine the microorganism in biological media, PCR analysis is carried out.
- For breath tests, the patient takes a solution of urea with labeled carbon atoms. The microorganism breaks down urea, and the labeled atoms are found in the air exhaled by a person. Additionally, an analysis is carried out to determine the concentration of ammonia in exhaled air.
The most accurate results are provided only by invasive examination methods.
Diagnosis of atrophy of the gastric mucosa according to OLGA
The “gold standard” for diagnosis for suspected atrophy of the gastric mucosa during endoscopic examination is the collection of at least 5 biopsies from different parts of the stomach with further assessment by a morphologist using the OLGA visual analogue scale. Using this scale, histological signs of the severity of inflammation and atrophy in different parts of the stomach are determined. Based on the results of the OLGA study, the attending physician will select the most effective treatment and determine the frequency of observation and endoscopic examination in your particular case.
Know that performing a histological examination is no less significant in the diagnosis of precancerous conditions than endoscopy itself.
If there are changes similar to atrophy of the gastric mucosa, metaplasia/dysplasia of the epithelium, or suspicion of early cancer, a biopsy from these areas is mandatory. It is the biopsy that in these cases confirms the diagnosis and determines further tactics of observation and treatment.
Long courses of treatment with NSAID drugs
There are 2 methods of treating Helicobacter pylori infection.
Treatment is carried out comprehensively. According to the WHO methodology, any drug regimen must meet the following criteria:
- Efficiency and speed
- Safety for the patient
- Convenience – use long-acting drugs, short course of treatment
- Interchangeability - any drug must be interchangeable with a complete analogue or generic
Currently, 2 methods have been adopted for the treatment of Helicobacter pylori infection. It is not recommended to use them simultaneously. If 1 scheme does not give a positive result, then the second one is used and vice versa. This prevents Helicobacter from developing immunity to drugs. Treatment regimens:
- Three-component method - 2 antibacterial drugs and 1 agent to reduce the acidity of gastric juice
- Four-component method - 2 antibacterial drugs, 1 - to reduce the secretion of hydrochloric acid, 1 - bismuth compounds
There is a 3rd treatment regimen for combating the microorganism. It is used when the first 2 did not have the desired effect. In this case, they speak of a resistant Helicobacter strain.
In this case, a preliminary endoscopic examination is carried out with the collection of material for a biopsy. In the laboratory, drugs for the treatment of Helicobacter pylori are individually selected. And only after that the doctor develops an individual course.
Antibacterial drugs
Macmiror destroys the parasite's genetic material.
The choice of antibacterial drugs that can cope with Helicobacter is small. This is "Trichopol" or "Metronidazole", or "Makmiror".
Trichopolum and Metronidazole are complete analogues. The main active ingredient of the drug, metronidazole, penetrates the microorganism and breaks down, releasing toxic substances.
They destroy the parasite's genetic material. The main active ingredient of Macmiror is nifuratel. It simultaneously inhibits the growth of bacteria and prevents the proliferation of microorganisms.
The peculiarity of this drug is that nifuratel does not reduce the patient’s overall immunity, but, on the contrary, improves the body’s defenses. Macmiror is a second-line drug. It is prescribed if treatment with metronidazole does not give the expected result. This medicine is used in the treatment of peptic ulcers in children.
Bismuth preparations and proton pump inhibitors in the treatment of Helicobacter
De-nol is a bismuth-based medicine.
A bismuth-based drug, De-nol, was used even before the discovery of the pathogenic microorganism. It has an enveloping effect, forming a film on the gastric mucosa.
It protects the walls from the aggressive effects of hydrochloric acid. After the discovery of Helicobacter, it turned out that bismuth subcitrate has an inhibitory effect on the bacterium. It is able to penetrate into the deep layers of the mucous membrane, where the pathogen likes to settle.
Proton pump inhibitors - Omez, Omeprazole, Pariet - block areas of the mucosa responsible for the production of hydrochloric acid. This promotes the healing of erosions, reduces the acidity of gastric juice and allows the antibiotic molecules to be preserved in an acidic environment.
Helicobacter pylori. How to do without antibiotics?
There is no effective treatment regimen for diseases associated with Helicobacter without the use of antibiotics. Only in some cases, without symptoms of an inflammatory process in the gastrointestinal tract and with a low contamination of bacteria, is it possible to remove Helicobacter pylori from the body.
All treatment regimens place a serious strain on the body. If carriage is detected without signs of inflammation, it is recommended to use more gentle methods.
Traditional medicine and Helicobacter
Traditional medicine recipes should not be used without consulting a doctor.
What does traditional medicine offer for the treatment of Helicobacter? Recipes are often contradictory:
- Raw chicken eggs. It is recommended to drink 1 raw egg before breakfast. This should normalize the normal microflora of the stomach.
- St. John's wort, calendula and yarrow are mixed in equal proportions. Make a decoction - 250 ml of water per 5 g of mixture. Take the infusion 0.5 cups 3 times a day for a month.
- It is recommended to consume 1 teaspoon of rosehip syrup per month.
- Flaxseed decoction. For 1 tablespoon of seed you will need 1 glass of water. Simmer over low heat for 20 minutes. Strain the broth and take 1 tablespoon before each meal.
The use of traditional medicine recipes should only be started after consulting a gastroenterologist. Otherwise, within a month of treatment you risk getting a perforated ulcer with all the ensuing consequences.
Preparing for a gastric biopsy
Preparation is required, because visualization of the mucous membrane needs to be improved. For this purpose, the study is carried out on an empty stomach (break after eating for at least 8 hours, after drinking for at least 4). A couple of days before the procedure, a diet of easily digestible foods is recommended, and on the day of the examination you should not smoke, chew gum, and stop taking medications.
You can get a consultation, find out the price of a gastric biopsy and sign up for an examination with the doctors of the Kuntsevo Medical and Rehabilitation Center by leaving a request on the website or by calling the clinic.
Diet for the treatment of Helicobacter pylori infection
Modern techniques allow you to be cured in a matter of weeks.
There is no specialized nutrition to combat Helicobacter. During treatment, you should adhere to the diet recommended for patients with gastritis, ulcers and other diseases of the stomach and intestines.
Food should be light, pureed and not irritate the mucous membranes. Heavy, spicy, fried and fatty foods are prohibited.
An ulcer is a dangerous disease. The cause of this pathology has now been identified. Helicobacter pylori should be treated under the guidance of a gastroenterologist. Modern techniques make it possible to get rid of this microorganism in a matter of weeks.
Biopsy during esophagogastroscopy, why is it necessary?
Endoscopy department
Endoscopist Sirotkina A.A.
Endoscopist Sidorenko AN
In the modern world, a huge number of people suffer from pain and discomfort in the abdomen, complain of heartburn, nausea, weakness, allergic reactions, and describe many other symptoms that require medical intervention. To determine the causes of the disease, the attending physician often refers to a study such as esophagogastroscopy.
Today, every person knows what it is and why a stomach examination is performed, so we will not consider in detail all the possibilities of the method, but will only dwell briefly.
Esophagogastroduodenoscopy is a study that allows you to look at the esophagus, stomach and duodenum using a special device - an endoscope, evaluate the lumen and mucous membrane of these organs, and identify a huge number of pathologies. The doctor gets the opportunity to examine each fold, monitor how the organ under study works, which departments do their job and which are not able to do this.
But the human eye, even enhanced by a modern device, is still imperfect, therefore, during esophagogastroscopy, patients, in the absence of contraindications, undergo a biopsy of the gastric mucosa, and, if necessary, the duodenum and esophagus. So why is this necessary? To what extent should it be carried out and how should we approach this kind of intervention?
A biopsy is the removal of a tiny piece of tissue followed by a thorough examination of its tissue and cellular composition under a microscope at high magnification. Examination of the resulting sample confirms tissue changes with an accuracy of more than 95% and allows us to determine:
- activity, severity and type of gastritis;
- presence and degree of contamination with Helicobacter pylori (Hp);
- the tumor or polyp is benign or malignant;
- precancerous conditions of the mucous membrane (colon type of metaplasia and dysplasia).
A biopsy is a very accurate research method, but its result directly depends on the quantity and quality of the material taken.
Endoscopic forceps open only 5-6mm; when taking a biopsy, a piece of tissue up to 2-3mm is taken, while the total area of the stomach is 500-800cm3. It's like cutting out a piece the size of a notebook square from the surface of a soccer ball. But the wall in different parts of the stomach also differs in its structure and functions. It is easy to understand that one or two pieces taken from the antrum (the outlet of the stomach) will not provide any information about the condition of the upper mucosa. They will not allow us to judge the prevalence and nature of inflammation, the degree of mucosal atrophy. Or, for example, there is a large ulcer in the stomach. A piece taken from only one edge will not completely exclude a malignant process that may develop on the opposite side. Therefore, for a high-quality and complete histological examination, multiple biopsies are necessary, and to assess the spread of the process, tissue sampling in all parts of the stomach is necessary.
Unfortunately, due to ignorance and lack of awareness, many patients, in order to shorten the examination time (and in the case of examination on a paid basis to save money), object to an extended biopsy, thereby limiting the diagnostic capabilities of the examination
To illustrate, let's give another example.
A study is being conducted on a patient with chronic gastritis. The same thing that “everyone has today.” However, to make a diagnosis of chronic gastritis, which sounds quite banal these days, a gastroenterologist needs a voluminous block of information, and the final result of treatment will directly depend on the scope of the study.
Indeed, according to the international Houston classification, the following types of gastritis are distinguished:
1. Autoimmune gastritis (gastritis type A), which occurs as a result of the fact that the body begins to perceive the mucous membrane of its own stomach as foreign. The development of atrophy may also be the result of long-term chronic gastritis or ulceration with destruction of the mucous membrane, which leads to the loss of gastric glands with their replacement by intestinal-type mucosa or fibrous tissue. Thus, this serious disease can lead to severe B12 deficiency anemia and cancer.
2. Non-atrophic (gastritis type B). The leading etiological factor in the development of Helicobacter pylori associated gastritis. The localization and prevalence of infection is important. It has been proven that when the infection is localized in the antrum, 1% of patients annually develop duodenal ulcers, but do not develop stomach cancer. With fundal and multifocal (multifocal) gastritis, 1% develop stomach cancer annually and duodenal ulcers are practically not found.
3. Atrophic multifocal (type A+B gastritis), mixed gastritis, where the cause, in addition to the above factors, is malnutrition and environmental factors.
Special forms:
4. Chemical (gastritis type C) is caused by chemical irritants, drugs and bile.
5. Radiation – radiation damage.
6. Lymphocytic – gastritis associated with celiac disease.
7. Granulomatous - occurs in systemic diseases such as sarcoidosis, Wegener's granulomatosis, Crohn's disease, etc.
8. Eosinophilic – allergic, occurs with food allergies and other allergens.
9. Other infectious diseases - bacteria, fungi, parasites can also cause gastritis.
10. Giant hypertrophic – Ménétrier’s disease.
As can be seen from the classification, the causes, and therefore the approach to the treatment of gastritis, are very diverse, so it is very important to make the correct diagnosis.
To do this, it is necessary to rely on 4 leading signs: localization of the pathological process, histological, macroscopic changes in the mucous membrane detected by endoscopy, etiological factors.
For the diagnosis and treatment of atrophic gastritis in 2008, a group of experts proposed a new OLGA system, which uses the assessment of histological signs of the severity of inflammation and atrophy of 5 gastrobiopsy samples (1 from the angle of the stomach, 2 from the body and 2 from the antrum) with subsequent determination of the degree and stages of chronic gastritis. Such a system is designed to provide a sufficient description of gastritis and reflect the dynamics of the process, forming a prognosis for the development of cancer. This means that the risk of cancer is higher. The more pronounced the atrophy and the larger the volume of the lesion. Based on the information obtained from one or two pieces, it is impossible to make any of this.
From all of the above, it is clear that for a correct diagnosis and, accordingly, for the optimal choice of treatment, an adequate and complete examination is necessary, including esophagogastroscopy with multiple and targeted biopsies, which requires patience and a conscious approach from the patient to the upcoming study. If the patient behaves restlessly, it is extremely difficult for the endoscopist to carry out a full examination with the collection of the required amount of material, as well as to take it precisely from strictly defined areas. In the process of making a diagnosis, the doctor and the patient have the same goal. And her name is Health.