Detailed description of the study
Helicobacter pylori is a spiral-shaped bacterium common among humans. This microorganism lives on the gastric mucosa due to its resistance to acidic environments.
It is assumed that infection with this infection occurs at an early age. The most likely route of infection is considered to be the fecal-oral route of infection when living with an infected person in the same house, as well as during a long stay in a large group.
In addition, the oral route of transmission of infection through saliva and kissing has been recorded. There have been suggestions about the possibility of Helicobacter pylori infection during fibrogastroscopy if the study is carried out using an endoscope that has been insufficiently treated with disinfectants.
After penetration into the stomach, Helicobacter pylori colonizes its mucous membrane, causing inflammation of the antrum of the stomach - gastritis. The bacterium has a protective mechanism against exposure to an aggressive acidic environment. It is capable of releasing ammonia to neutralize acid. However, the metabolic products of Helicobacter pylori negatively affect the gastric mucosa.
As a result of Helicobacter pylori entering the body, the immune system forms antibodies - immunoglobulins - to this bacterium. During infection, antibodies of class A and M are initially formed; they are soon replaced by immunoglobulins of class G.
In most cases, the body is not able to completely defeat Helicobacter pylori, which predetermines the preservation of a high level of class G antibodies to it. Class A antibodies are produced 2-3 weeks after infection. It is believed that their concentration in the blood depends on the intensity of inflammation: the more pronounced this process is, the higher the level of immunoglobulins A.
When combined with other unfavorable conditions, such as stress, poor diet, and infection with this bacterium, it leads to the formation of erosions and stomach ulcers. The following symptoms are noted:
- Pain in the upper abdomen (mainly on an empty stomach);
- Nausea;
- Belching air.
Some people are asymptomatic when infected with Helicobacter pylori. Long-term exposure of the bacterium to the gastric mucosa leads to the development of atrophy and decreased acid production. The risk of developing stomach cancer and lymphoma increases. A particularly high risk of developing cancer is observed in those whose relatives suffered from it.
Determining the presence of Helicobacter pylori infection in the body is important for early diagnosis of gastric pathology. This test is prescribed in conjunction with the detection of other AT antibodies (IgG, IgM) and other laboratory and instrumental diagnostics, for example, after or before FGDS. It is necessary to donate venous blood for analysis.
Tests for Helicobacter pylori. Which is the most effective?
In modern laboratory diagnostics, several methods are used to detect the presence of Helicobacter pylori in the body: using a blood test, stool test, breath test or biopsy. Why is analysis needed? A simple example: if a person has a clinical picture of gastritis, then you need to first understand the reason for its appearance and development, and only then prescribe treatment.
The main indications for testing for Helicobacter pylori:
- gastritis;
- constant heartburn;
- stomach pain after eating;
- frequent diarrhea and constipation;
- lack of appetite;
- flatulence, rumbling in the stomach.
Enzyme immunosorbent blood test for Helicobacter (ELISA)
Most often, gastroenterologists refer the patient for a blood test. However, you need to understand that there is no helicobacter bacteria in the blood. Using an enzyme immunoassay, antibodies to the presence of Helicobacter are detected in the blood, which are produced by the immune system in response to infection. This analysis cannot be called 100% accurate. The reason is that a person’s immune response can change at different points in life. For example, a patient had a sore throat, took a course of antibiotics, his immunity decreased due to the illness, the production of antibodies was impaired... In this case, the analysis will be false negative.
Stool analysis for Helicobacter
Using this simple analysis, Helicobacter pylori DNA can be detected in human biomaterial. The analysis is highly accurate – up to 95%. Suitable for young children, elderly people and those for whom biopsy is contraindicated. The study itself is carried out using the PCR (polymerase chain reaction) method. Research in the laboratory is carried out as follows: a section of DNA is isolated from the biomaterial, after which it is duplicated on a cycler. This makes it possible to determine whether the sample contains a genomic fragment characteristic of the Helicobacter bacterium.
Shortened rapid test for Helicobacter
The principle of the breath test is that bacteria are located in the submucous membrane of the stomach and during their life processes they release a large amount of urea. This urea is picked up by the breath test and gives a positive reaction. Before the procedure, the patient must take a special solution, after which 4 air samples are taken within an hour. The test result is visible immediately.
However, the test is also not 100% sensitive. It is worth noting that a shortened test for Helicobacter in Sochi can only be found in large medical institutions.
Culture for Helicobacter
This is the most sensitive method giving an accurate result. However, the study itself is quite complicated, since the material for the biopsy, which is a section of the gastric mucosa, is taken during gastroscopy. There is a need for prompt communication between the endoscopist and the LHC laboratory so that the biomaterial can be sent for examination immediately after the procedure.
The decision to prescribe a particular diagnosis is made by a gastroenterologist, depending on the clinical picture of the disease and the patient’s condition. Sometimes several tests will be needed to confirm the presence of bacteria in the body. Note that most often a blood test is prescribed. Less often - bacterial culture for Helicobacter. The most accurate would be bacterial culture, but from the point of view of the complexity of the procedure and comfort for the patient, this study is less preferable.
“According to the recommendations of the Austrian community of gastroenterologists who study Helicobacter, stool analysis and a breath test are prescribed to those patients who have already been treated for Helicobacter for control purposes,” explains Vladimir Kadushev, gastroenterologist at the ELISA Medical Center. – That is, primary diagnosis is carried out using enzyme immunoassay. But the bacteria's antibody titers, in other words their memory, can persist throughout life. For this reason, blood is not used for control testing.
Do I need to be tested for Helicobacter pylori again?
Yes, after a course of treatment it is necessary to take a repeat test for Helicobacter to assess the effectiveness of therapy.
How to test for Helicobacter pylori?
In order for the result of the study to be as accurate as possible, it is necessary to properly prepare for the analysis and follow the rules when submitting biomaterial.
- Preparing for stool donation
You should not take antibiotics at least a month before donating the biomaterial. Three days before going to the laboratory, do not eat so-called “coloring foods”: black currants, beets, grapes and others. The ban also applies to products with coarse fiber: carrots, radishes, cabbage, bran. A gastroenterologist will remind you of the need to stop taking medications that stimulate gastric motility. To collect biomaterial, you need to purchase a special container from the pharmacy. Try to deliver the biomaterial to the laboratory promptly, since the shelf life of the biomaterial is no more than 10-12 hours.
- Preparing for a blood test
On the eve of the blood test, exclude fatty and fried foods from your diet, do not smoke, do not drink alcohol, and avoid strenuous physical activity. Blood is donated in the morning on an empty stomach.
- Preparing for a breath test
You should not eat before taking a breath test. If you take the Helicobacter test in the morning, then your last meal should be no later than 22.00. 3 days before the test, remove from your diet foods that increase gas formation - apples, legumes, cabbage, baked goods. Avoid liquids that increase CO2 concentrations in your exhaled breath, such as carbonated water. The ban also applies to cigarettes, alcohol and chewing gum.
- Preparing for a biopsy
Before FGD with biopsy, you must refrain from eating for 12 hours. Also, 2 hours before the test you should not smoke or drink.
References
- Ivashkin, V.T., Maev, I.V., Abdulganieva, D.I. etc. Practical recommendations of the Scientific Community for Promoting the Clinical Study of the Human Microbiome (NSOM) and the Russian Gastroenterological Association (RGA) on the use of probiotics for the treatment and prevention of gastroenterological diseases in adults. Russian Journal of Gastroenterology, Hepatology, Coloproctology, 2022. - T. 30.
- Guevara, B., Cogdill, A. Helicobacter pylori: A Review of Current Diagnostic and Management Strategies. Dig Dis Sci., 2022. - Vol. 65(7). – P. 1917-1931.
- Choi, I., Kim, C., Lee, J. Family History of Gastric Cancer and Helicobacter pylori Treatment. N Eng l J Med., 2022. - Vol. 382(5). — P. 427-436.
- Materials from the test system manufacturer.
Helicobacter pylori (Gag A) toxigenic strain (total) IgA, IgM, IgG
Helicobacter pylori infection is relevant in modern society for patients of any gender and age. Infection with the toxigenic strain of Helicobacter pylori (GagA) is very high, which is associated with an easy transmission mechanism (fecal-oral). Helicobacter pylori causes gastritis, gastric and duodenal ulcers in almost 100% of cases. Also, it can cause stomach cancer (as a result of malignancy of an ulcer or an atrophic process in the intestine).
To determine the presence of infection, as well as the activity of the process, the most popular method is the detection of antibodies of various classes to Helicobacter pylori (total antibodies). Total antibodies of Helicobacter pylori are antibodies of the IgG, IgM and IgA classes. Each of these classes has a specific function and helps in the correct interpretation of the stage of the disease.
IgA to Helicobacter pylori is a class of antibodies that are responsible for local immunity. IgA to Helicobacter pylori is found on the mucous membrane of the gastrointestinal tract. Their quantity is the least informative, but an increase in titer to significant numbers indicates severe inflammation of the mucous membrane.
IgM to Helicobacter pylori are responsible for an acute infection that occurred no more than 2-3 months ago. If IgM antibodies to Helicobacter pylori are detected in the singular, then the infection occurred recently - 2-4 weeks ago. If IgG is also present, then the infection lasts no more than 2-3 months. The absence of IgM to Helicobacter pylori GagA, in the presence of IgG, confirms a long-term chronic infection. The reappearance of IgM antibodies to Helicobacter pylori GagA allows one to judge about re-infection or relapse of infection.
IgG to Helicobacter pylori GagA is produced at 2-3 weeks of infection and remains for a long time. Their concentration slowly decreases during eradication therapy, but they completely disappear only a few months after complete elimination of the pathogen.
Determination of all types of antibodies to Helicobacter pylori - total antibodies, allows you to evaluate the entire spectrum of protective immunoglobulins and make a correct diagnosis.
To identify Helicobacter pylori, the total antibody test is not the only one; invasive techniques and a breath test are often used. But taking the test for antibodies to Helicobacter pylori GagA is the most optimal in terms of speed of execution and minimal invasiveness (blood drawing).
Quantitative determination in the blood of specific immunoglobulins (immune antibodies) of class A to bacteria of the Helicobacter pylori species by enzyme immunoassay for the purpose of diagnosing the infectious process caused by this pathogen in the wall of the stomach and/or duodenum.
Synonyms Russian
IgA class antibodies to H. Pylori, class A immunoglobulins to the causative agent of helicobacteriosis.
English synonyms
IgA H. pylori Antibodies, IgA, Quantitative.
Research method
Enzyme-linked immunosorbent assay (ELISA).
Units
IU/ml (international unit per milliliter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
Do not smoke for 30 minutes before the test.
General information about the study
Helicobacter pylori (Helicobacter pylori), IgA, are specific immunoglobulins (immune antibodies) of class A to the bacteria Helicobacter pylori. Test for Helicobacter pylori, IgA (quantitative), is a laboratory test of blood serum using an enzyme-linked immunosorbent assay, which is carried out to detect infection caused by Helicobacter pylori in the wall of the stomach and duodenum based on the IgA titer to this type of pathogen.
Helicobacter pylori is a type of microorganism that can infect the mucous membrane of the stomach and/or duodenum and, under certain circumstances, can cause gastritis, duodenitis, gastric and duodenal ulcers, and gastric malignancies. The name “Helicobacter pylori” literally translates as “spiral-shaped bacterium that lives in the pylorus of the stomach.”
The importance of Helicobacter pylori in the development of diseases of the stomach and duodenum has been proven relatively recently. For a long time it was believed that bacteria could not exist in the acidic environment of the stomach. Intensive research in this area began in the early 80s of the 20th century. To date, a large amount of data on this problem has already been accumulated, and the treatment of gastritis and peptic ulcers by eliminating helicobacteriosis is a generally accepted practice.
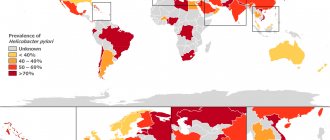
Helicobacteriosis is the most common infection worldwide. It is believed that 60% of the world's population are carriers of Helicobacter pylori. However, in developing countries the prevalence of this infection is much higher (up to 100% of the adult population) than in developed countries (20-65%), which is associated with the influence of sanitary and hygienic living conditions of people.
Infection in most cases occurs in childhood, the pathogen is transmitted from person to person. The presence of infection in parents is a factor of increased risk of infection in children. However, only a small proportion of infected individuals may develop overt symptoms of the disease, and this may occur over a significant period of time (months and years) after infection.
After entering the stomach, Helicobacter pylori penetrates into the layer of mucus covering the wall of the stomach and penetrates deep into the mucous membrane cells. There, bacteria begin to produce ammonia and enzymes that break down stomach mucus. Ammonia reduces the acidity of gastric juice, which reflexively increases its formation and secretion by the stomach. The destruction of mucus leads to disruption of the layer that protects the mucous membrane from self-digestion, resulting in chemical damage to the gastric wall. In addition, Helicobacter pylori produces specific toxins that cause an immune response from the body, as well as structural changes and cell death in the wall of the stomach and/or duodenum. The combination of all these factors leads to inflammation, and in more severe cases, ulcers.
However, there is no clear relationship between the presence of infection and the severity of the disease, and in many cases there are no signs of health problems at all. Currently, this is explained by the fact that Helicobacter pylori comes in several varieties, which have different abilities to cause disease - from very aggressive to almost harmless. In addition, various additional factors are important that can contribute to the weakening of the body and the creation of favorable conditions for the development of the disease: dietary habits, decreased immunity, chronic fatigue, etc.
The disease can manifest itself as pain, a feeling of heaviness in the stomach after eating, nausea, heartburn, an unpleasant and/or sour taste in the mouth and/or bad breath, and sour belching.
The development of the infectious process is accompanied by an immune response from the body. One of the manifestations of immune defense is the accumulation of specific immunoglobulins (antibodies) in the blood: IgA and IgG. Laboratory analysis of blood serum for these antibodies is used in the complex diagnosis of helicobacteriosis.
IgA is detected 2-3 weeks after infection and possibly for several subsequent years. Thus, the detection of IgA indicates infection with Helicobacter pylori. The absence of a decrease in IgA titers over time is a sign of non-declining activity of the infectious process. In addition, IgA is responsible for immune protection directly at the site of the infectious process (local immunity). In this regard, it is believed that the level of IgA depends on the severity of inflammation in the wall of the stomach/duodenum. Successful treatment is accompanied by a decrease in IgA levels, which makes it possible to judge the effectiveness of the therapy by analysis. The results of the analysis are given in quantitative form in the form of antibody titer values. The antibody titer reflects the intensity of the infectious process.
What is the research used for?
- For the diagnosis of Helicobacter pylori, among other research methods, for symptoms of gastritis and/or gastric ulcer.
- To determine the severity of infection and/or inflammatory process in the wall of the stomach and/or duodenum caused by helicobacteriosis.
- To evaluate the effectiveness of treatment measures carried out for Helicobacter pylori infection.
- For the diagnosis of helicobacteriosis in high-risk groups for the purpose of preventive treatment.
When is the study scheduled?
- For symptoms of gastritis, duodenitis and/or peptic ulcer of the stomach or duodenum: pain, heaviness in the upper abdomen after eating, nausea, heartburn, unpleasant and/or sour taste in the mouth and/or bad breath, sour belching.
- When it is necessary to assess the severity of the inflammatory/infectious process caused by Helicobacter pylori.
- If during the treatment of helicobacteriosis there is a need to evaluate the adequacy of therapeutic measures or their final results.
- During preventive examinations of persons at increased risk of developing gastritis and/or gastric ulcers in order to take measures to prevent the disease.
What do the results mean?
Reference values
Result: negative.
Concentration: 0 - 13.5 IU/ml.
The results of the analysis are given in quantitative form in the form of an antibody titer, which reflects the degree of intensity of the infectious process. The obtained data are evaluated relative to the specified reference values.
Reasons for the positive result:
- Helicobacter pylori infection.
Reasons for negative results:
- early period of infection (less than 2-3 weeks);
- successful treatment/recovery;
- no infection.
What can influence the result?
A negative result can be obtained if less than 2 weeks have passed from the onset of the infectious process to the study.
Confirmed facts about Helicobacter pylori (Hp)
Established facts about HP infection and its properties:
- Helicobacter pylori (Hp) is a non-invasive bacterium (spiral-shaped microaerophile) with 4–5 unipolarly located flagella, which allow it to move in the epithelial gastric mucus in search of optimal conditions for life (pH, osmolarity, etc.).
- HP were able to adapt to the sharply acidic environment of the stomach due to their small genome size and the ability to undergo rapid mutations in unfavorable conditions for their existence, occupying their ecological “niche.”
- Recently, it was found that HP is a relatively young bacterium, whose “age” does not exceed 50 thousand years.
- HP infection is widespread among people in the world. Thus, in developed countries of Western Europe and North America it occurs in 35-50% of the population, and in developing countries of Asia, Africa and Latin America - in 90% or more, on average in 60% of the world's population.
- There is an opinion that before the widespread introduction of antibacterial therapy (ABT) - in the 50s of the 20th century - the prevalence of HP infection reached 80%, but in subsequent years it decreased to 60%.
- In unfavorable conditions for existence, HP are transformed from a spiral shape (helical-like) to a coccoid-like shape, in which metabolism is sharply reduced and reproductive ability is lost, but resistance to adverse environmental factors is increased. Once in favorable conditions, the coccoid forms of bacteria again turn into spiral forms, undergoing reversion.
- At later stages of evolution, part of the HP acquired a “pathogenecity associated island” (PAI), located on a section of chromosomal DNA. It is believed that its appearance is associated with the horizontal transmission of the “island” from some other microbe.
- When studying the “pathogenicity island”, “cytotoxicity genes” were identified: cagA (cytotoxin-associated gene A); vacA (vacuolating-associated cytotoxin A); iceA (induced by contact with epithelium); babA (blood-group associated adhesion). The main marker of the “pathogenicity island” is the immunodominant cytotoxin (protein) CagA, encoded by the cagA gene.
- The “virulence determinants” of Hp were established: urease (ureA1 gene), adhesion factor (hpaA gene), superoxide dismutase (sodA gene), vacuolating cytotoxin (vacA gene) and catalase (catA gene). Urease acts as a toxin, destroying urea in food. This produces ammonia, which damages the epithelial cells of the stomach.
- The main reservoir of HP infection is humans, and the main route of infection is oral-oral and fecal-oral. It has not yet been possible to detect HP in the environment (soil, water).
- HPs are distinguished by a special tendency to variability - genetic polymorphism, and therefore they are often called a “chameleon”.
general characteristics
The pathogenic microorganism H. pylori, causing gastritis, duodenitis, gastric ulcer (in 70% of cases) and duodenal ulcer (in 90%). Recent data indicate a close connection between Helycobacter pillory and the development of cancer. Determination of the level of immunoglobulins is the most reliable (specificity 91%, sensitivity 97%), the most accessible, least invasive method for diagnosing Helicobacter pylori infection. These antibodies appear 1-2 weeks after infection and are indicators of an acute process. Used to diagnose the acute period of Helicobacter pylori infection. Women are characterized by higher serum IgA levels. An increase in the proportion of IgA in the IgA/IgG ratio is a prognostic sign in the development of gastric cancer.
Interpretation:
- Positive result (>20 U/ml): acute stage of the disease.
- Negative result (<15 U/ml): absence of infection, period of seronegativity (up to 1 week after infection). Note. For primary screening it is necessary to determine IgA, IgG. 4 months after the end of treatment, it is necessary to determine the control level of IgG in the patient’s blood. Negative readings indicate complete recovery. 15-20 U/ml is doubtful.
Sample result (PDF)