To correctly assess the functioning of the esophagus, it is very important to carry out appropriate diagnostics, such as manometry. In this way, errors in treatment can be eliminated and the patient’s recovery can be accelerated. An instrumental examination, which is prescribed by the attending physician, is very necessary, since physical methods do not allow us to see the full picture of the disease. Moreover, nowadays diseases of the intestines and stomach are the most common. In a healthy person, the esophagus is practically not subject to irritation, while in a patient with stomach problems, frequent spasms are observed, an inflammatory process appears, narrowing, etc.
For what symptoms is an esophageal examination prescribed?
Manometry as a method for studying the stomach and esophagus
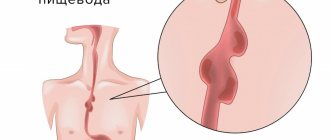
When a patient complains of pain during or after eating, then it is necessary to undergo an appropriate examination of the esophagus to determine the cause of the discomfort. If a person complains of pain when swallowing, namely when eating solid food, then this indicates carcinoma of the esophageal membrane.
Pain when eating any food indicates that the patient has impaired motility of the esophagus, the patient has a burn of the esophagus, various injuries due to caustic acids or alkalis, the esophagus is affected by infections, etc. The development of cancer or reflux - esophagitis is indicated by severe pain when eating in the sternum area.
Diseases of the esophagus require diagnosis. The doctor may prescribe different tests, depending on the symptoms the patient feels. Thus, diagnostics are carried out using the following methods:
- using esophagofibroscopy;
- using x-ray examination;
- using computed tomography or spiral tomography;
- endoscopic ultrasound is performed;
- using esophagoscopy using a rigid esophagoscope;
- using pH-metry and esophagotonokymography.
Among all possible studies of the esophagus and stomach, special attention should be paid to esophagomanometry.
2. How to prepare and how is the procedure performed?
How to prepare for an esophageal examination?
If the doctor has prescribed you one of the examination procedures, then you need to do the following:
- Do not drink alcohol, smoke or take antacids (acid neutralizers) for 24 hours before the examination;
- Do not eat or drink 8-12 hours before the examination;
- Tell your doctor if you have any known esophageal problems, such as varicose veins or heart failure.
How are esophageal examinations performed?
The test is performed while sitting. You will be given a local application of anesthesia to the nasopharynx. Each test requires insertion of a thin, flexible tube through the nose or mouth. This is not a very pleasant procedure and you may gag. To get rid of this feeling, try to breathe slowly and measuredly, concentrate on your breathing. Your pulse and blood pressure will be monitored during the examination.
pH-metry of the esophagus
A special probe is attached to a tube that is inserted into the esophagus, which measures the acidity in the esophagus. For long-term monitoring, the probe may be left in the esophagus for 24 hours to obtain more complete information. You will need to wear a recording device. It is attached to the wrist or shoulder.
During long-term daily pH measurements, it is not recommended to consume highly acidic foods, such as fruit juices.
Esophageal manometry
Esophageal manometry requires special instruments that are attached to a tube. Sometimes you will be asked to swallow or hold your breath. You will also need to drink water.
Visit our Gastroenterology page
Manometry - detailed examination of the esophagus on an outpatient basis
An outpatient test called manometry measures how strongly the muscles of the esophagus contract and how they interact with each other during the swallowing process. Depending on the type of damage to the stomach and esophagus, the symptoms, the first signs of the disease may differ or, on the contrary, have great similarities; only with the help of manometry can an accurate diagnosis indicating a specific disease be established.
This study allows us to evaluate the functioning of certain parts of the esophagus, including the part responsible for swallowing, the lower and upper parts of the esophageal sphincter, and the esophagus itself. Manometry allows you to correctly plan antireflux surgical operations and keep the patient’s condition under control in the postoperative period. Esophagomanometry is prescribed to the patient when:
- the swallowing process is impaired;
- in case of systemic diseases, dysphagia is observed;
- a preparatory stage is necessary before surgery;
- it is necessary to monitor the patient in the postoperative period;
- Before pH testing, it is necessary to assess the functioning of the lower esophageal sphincter.
Despite the fact that diagnostics can achieve accurate and correct results, the study has some limitations. It is not suitable for everyone; there is a category of patients for whom manometry is contraindicated. Thus, it cannot be performed on people suffering from mental disorders, as well as those who have certain diseases of the esophagus, including ulcers, varicose veins, etc. It is also prohibited to carry out the study on patients who have poor blood clotting, patients suffering from an esophageal tumor, or a risk of developing one is suspected.
Performing esophageal manometry procedure
Manometry does not require any anesthesia. During the procedure, the patient is in a lying position. A special probe is inserted through his nose, and a special gel is injected into the mucous membrane of the nose and throat, which neutralizes sensitivity and also suppresses the gag reflex. During the process, the patient is asked to perform swallowing movements and also drink a small amount of water. The results of the diagnostic procedure are displayed on the computer screen and subsequently analyzed by diagnosticians. Typically, esophageal manometry takes about 20-30 minutes.
Additional services for foreign patients
The Elite Medical clinic offers each patient a completely new approach to medical tourism in Israel. Now, in addition to diagnostic and therapeutic services, our clinic offers to purchase a set of additional services that will completely relieve you of all everyday problems and allow you to concentrate exclusively on the process of treatment and diagnosis.
The complex includes the following services:
- ordering air tickets;
- meeting the patient at the airport and booking a hotel room;
- purchasing a local SIM card;
- support by an experienced curator with a medical education;
- support by a qualified translator;
- translation of all medical documents;
- transportation support, which includes transfers from the airport to the hotel, as well as from the hotel to the clinic for the necessary procedures.
The complex costs $400, and this amount is paid once: if you need to stay in Israel for a longer period, no additional expenses are required.
Manometry method
Manometry is carried out using special equipment
Manometry is carried out using special equipment - a catheter, which requires appropriate maintenance. A catheter is placed in the esophagus to measure contractile pressure. The equipment is equipped with capillary tubes whose internal diameter is 0.8 mm. The most commonly used catheter for testing is a catheter that has eight capillary tubes that surround a centrally located tube with a slightly larger diameter. All capillary tubes are individually connected to pressure sensors.
Traditional water-perfusion manometry has replaced traditional water-perfusion manometry in the diagnosis of patients with symptoms associated with impaired motor function of the esophageal tube. Studying the motor function of the esophagus using MVR allows one to obtain accurate quantitative and qualitative data on intraluminal pressure, coordination and motility of the esophageal muscles. Manometry is of particular importance for differential diagnosis between primary and secondary disorders of esophageal motility, which may be accompanied by heartburn, dysphagia, non-coronary chest pain and other symptoms characteristic of gastroesophageal reflux disease (GERD). Impaired esophageal motility may be a major cause of dysphagia and chest pain. Esophagomanometry is currently the gold standard in assessing esophageal motility.
Traditional water-perfusion manometry has replaced traditional water-perfusion manometry in the diagnosis of patients with symptoms associated with impaired motor function of the esophageal tube. Studying the motor function of the esophagus using MVR allows one to obtain accurate quantitative and qualitative data on intraluminal pressure, coordination and motility of the esophageal muscles. Manometry is of particular importance for differential diagnosis between primary and secondary disorders of esophageal motility, which may be accompanied by heartburn, dysphagia, non-coronary chest pain and other symptoms characteristic of gastroesophageal reflux disease (GERD). Impaired esophageal motility may be a major cause of dysphagia and chest pain. Esophagomanometry is currently the gold standard in assessing esophageal motility.
History of the method
The first measurements of esophageal motor function were made using water-perfusion catheters with one or more side holes. Subsequently, catheters with 4–8 side holes became common for esophageal manometry. Measuring lower esophageal sphincter (LES) pressure remained challenging. This is because the LES tends to move upward during swallowing, moving the focal point sensor away from the high pressure area. During the study, the focal probe was pulled through the sphincter several times.
In 1977, a sleeve sensor catheter was introduced, which added a six-centimeter sensor to continuously measure LES pressure.
In the early 1990s, MVR was developed, which allowed an increase in the number of pressure sensors. This contributed to reducing the distance between the corresponding sensors to 1 cm. As a result, it became possible to measure pressure along the entire length of the esophagus, starting from the upper esophageal sphincter (UPS) and to the LES. This study provided a complete image of the motor function of the esophagus. In addition, the short interval between transducers allowed the software to measure pressure readings between the probe sensors. A significant refinement of the method made it possible to evaluate the change in pressure in a three-dimensional plane. This played an important role in the topographical approach to displaying the study data. At the same time, different colors corresponded to high and low pressure values. As a result, it became possible to display manometric data in the form of a continuous pressure graph, in which the amplitude is expressed in color shades. The result was a clear and easy-to-interpret picture of the contractile function of the esophagus.
The introduction of the topographic method led to the emergence of new indicators and parameters for analyzing the data obtained. There was a need to re-evaluate the classification scheme, which was originally developed for traditional manometric measurements.
In 2008, after a study of patients and healthy volunteers, the first official classification for MVR was developed, the Chicago Classification of Esophageal Motor Disorders. A second revision of the classification was published in 2012. In 2015, the classification was updated, the third version was published in the journal Neurogastroenterology and Motility. MVR is becoming an increasingly popular method and is now the global standard for the clinical assessment of esophageal motility disorders.
The main advantages of MVR are: accuracy of measurements, simplicity of the procedure and clarity of research results. Directly during the research process, the software synthesizes a holistic picture of the motor activity of the esophagus. Thus, an image of the functional activity of the esophagus is displayed on the screen in three dimensions in real time.
We have been diagnosing esophageal diseases using the MVR method using a solid-state catheter since 2016. For this purpose, at the Minsk Scientific and Practical Center for Surgery, Transplantology and Hematology, a room for functional diagnostics of esophageal diseases was opened, where MVR and daily intraesophageal pH impedance measurements are currently performed. The studies are performed on medical equipment from Medtronic (GivenImaging system). Includes the ManoScan HRM module (A120), a reusable 36-solid-state sensor (transducer) probe providing 432 pressure measurement points in the esophagus from the pharynx to the stomach, and Manoview software.
Advantages of MVR compared to water-perfusion manometry:
- the screen simplifies the positioning of the catheter in the esophagus and reduces the likelihood of incorrect placement of the catheter within the esophageal tube;
- simultaneous assessment of the pressure structure in all parts of the esophagus is carried out, which eliminates the need to re-position the probe;
- the time for conducting a manometric study is reduced in comparison with traditional manometry using water-perfusion catheters;
- shorter intervals between pressure sensors guarantee the safety of relevant information, and high resolution leads to greater reliability of the study; this provides a more detailed assessment of pressure measurements and a more objective analysis of esophageal motility disorders;
- Finally, a standardized display method and additional computer algorithms provide more objective information than the linear graphs obtained with traditional manometry.
Indications for MVR:
- dysphagia (after excluding organic causes) - for the diagnosis of esophagospasm, achalasia, ineffective motility of the esophagus;
- non-coronary chest pain - for the diagnosis of distal esophagospasm, hypercontractile esophagus, esophageal achalasia, hiatal hernia (HH);
- preoperative examination of patients with achalasia cardia - to confirm the diagnosis and clarify the type of achalasia;
- preoperative examination of patients with GERD who are planning antireflux surgery - to exclude ineffective motility of the esophagus, achalasia, and clarify the size of the hiatal hernia;
- preoperative examination of obese patients who are planning bariatric surgery;
- monitoring the effectiveness of surgical treatment of achalasia cardia and GERD;
- determining the distance to the LES before installing a pH-impedance probe;
- dysphagia after antireflux surgery.
Study protocol
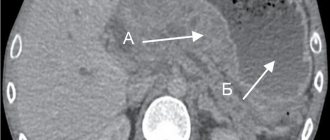
Carrying out MVR consists of two stages: analysis of motility at rest and during a swallow. The resting analysis includes assessment of the location of the UHL and LES, as well as the resting pressure in the sphincters (see Fig. 1a) . At this moment, the patient does not swallow and breathes calmly. Determination of the contractile and evacuation functions of the esophagus is assessed in response to ten sips of water, 5 ml each. At the time of swallowing movements, the ability of the UPS and LES to relax, the intensity of contraction and peristaltic activity of the thoracic esophagus are assessed. In addition, attention is drawn to the presence of all required segments of the peristaltic wave. Normally, there is synchronous relaxation of the UPS and LES, increasing duration and strength of peristaltic contractions as the wave moves in the distal direction. The transition zone between the proximal (striated muscles) and middle (smooth muscle) parts of the esophagus is clearly visualized (see Fig. 1b) . The interval between sips should be at least 30 seconds.
Rice. 1. MVR results are normal
a) pressure of the UHL and LES at rest
b) the peristaltic wave of the esophagus is normal
In addition to performing the standard protocol, some researchers recognize the importance of additional diagnostic tests, such as swallowing solid foods (bread, dry biscuits) and multiple rapid sips of liquid (five sips of 2 ml, followed by intervals of 2-3 seconds). This allows a more objective assessment of latent disorders and reserve capabilities of the motor function of the esophagus.
Data interpretation
According to the Chicago classification, the analysis and interpretation of MVR are carried out in two stages in accordance with the scheme presented in table. 1 . First, each specific pressure graph of a sip of water is assessed and classified separately, then the totality of identified changes is considered. For this purpose, an integral indicator was introduced - the distal contractile integral (DCI, distal contractile integral), which reflects both the strength and speed of contraction of the smooth muscle of the esophagus. This indicator is calculated based on the contraction time, length and pressure amplitude of the peristaltic wave (mm Hg / cm/s) (see Fig. 2) . Depending on the strength (intensity) of the contraction, the Chicago classification divides contractions into the following types:
- normal force reduction: 450
- hypercontraction: DCI>8,000 mmHg. Art. / cm/s. The contraction becomes excessively intense and is accompanied by severe chest pain;
- ineffective contraction: DCI<450 mm Hg. Art. / cm/s.
- In addition, ineffective contractions are divided into failed contractions (DCI<100 mmHg/cm/s) and weakened contractions (100
Table 1. Chicago classification of esophageal motor dysfunction
The next indicator is distal latency (DL, distal latency). It is represented by a period of time extending from the moment the opening of the UHL begins until the contraction deceleration point (CDP) (see Fig. 2) . Normally, the duration of the DL interval is at least 4.5 seconds. This indicator was included in the analysis in order to identify the so-called. premature contractions that occur with diffuse (distal) esophagospasm or type 3 achalasia. From a pathophysiological point of view, the appearance of premature contractions indicates dysfunction (or death) of inhibitory neurons of the myenteric plexus.
With normal peristaltic activity of the esophagus, intrabolus pressure (IBP) should exceed intragastric pressure, but should not be higher than 30 mm Hg. Art. In the presence of obstruction to advance the bolus, with preserved peristaltic activity of the thoracic esophagus, intrabolus pressure increases. According to the Chicago classification, there are several types of increased intrabolus pressure:
- total increase in intrabolus pressure - an increase in intrabolus pressure (more than 30 mm Hg) in the esophagus throughout the entire length from the LES to the UPS. Most often observed in type 2 achalasia;
- segmental increase in intrabolus pressure - an increase in intrabolus pressure from the peristaltic wave of the thoracic esophagus to the area of the esophagogastric junction. This manometric picture is observed with mechanical obstruction of the cardia (stricture, hernia) or with type 3 achalasia;
- increased intrabolus pressure in the area of the esophagogastric junction (EGJ).
Rice. 2. Basic parameters of esophageal peristalsis
Disorders caused by PVC obstruction
The introduction of MVR has led to new research directions to improve the analysis and quantification of LES relaxation and esophageal motility. These elements are important in assessing disorders caused by PVC obstruction. According to the research algorithm recommended by the Chicago classification, the first indicator studied is the total relaxation pressure (IRP, integrated relaxation pressure). Lack of adequate relaxation of the LES, accompanied by an increase in IRP of more than 15 mm Hg. Art., is observed in several forms of impaired motor function of the esophagus.
Achalasia of the esophagus. The analysis of each new sip begins with calculating the effectiveness of relaxation of the LES using a special integral indicator - the total relaxation pressure. IRP is a mathematical value that is calculated by the analysis program in a 10-second interval starting from the moment the IPS opens. The IRP is represented by the sum of the areas with the lowest residual pressure over 4 seconds. Normally, IRP does not exceed 15 mmHg. Art. Using IRP, esophageal achalasia can be identified more accurately than with traditional manometry. In addition, MVR allowed, depending on the detected changes in peristalsis of the thoracic esophagus, to identify three main types of achalasia.
All three types of achalasia are characterized by incomplete relaxation of the LES:
- achalasia type 1 - an increase in the total relaxation pressure of the LES (IRP≥15 mmHg), accompanied by a complete absence of contractions in the thoracic esophagus (DCI<100 mmHg) ( see Fig. 3a );
- achalasia type 2 - an increase in the total relaxation pressure of the LES (IRP≥15 mm Hg), accompanied by the absence of peristaltic contractions, however, the preserved tone of the esophageal walls causes a total increase in intrabolus pressure ( see Fig. 3b );
- achalasia type 3 - an increase in the total relaxation pressure of the LES (IRP≥15 mm Hg), accompanied by premature (spastic) non-peristaltic contractions of the thoracic esophagus (DCI>450 mm Hg, DL<4.5 s), ( see Fig. 3c ).
This classification option turned out to be significant for predicting the effectiveness of treatment. Some researchers show differences in response to treatment between the three types of achalasia. Studies have shown a positive response to treatment, primarily in patients with type 2 achalasia. An unsatisfactory response was recorded in patients with type 3 achalasia. This classification allows you to choose an individual and more effective treatment method for a particular patient.
Obstruction of the esophagogastric junction. MVR identified a group of patients with incomplete relaxation of the LES in combination with preserved peristalsis, but this did not meet the criteria for achalasia. In the previous classification of MVR, this disorder was called functional obstruction. The use of MVR in these patients revealed an increase in intrabolus pressure. Currently, such changes are defined as obstruction of the esophagogastric junction.
Rice. 3. Types of esophageal achalasia: a) type 1; b) type 2; c) 3rd type.
Significant disturbances of peristalsis
They never occur in healthy people and do not occur with obvious clinical symptoms. These abnormalities are associated with marked changes in DL and DCI scores. At the same time, the average IRP values are preserved.
Lack of contractility. A rare phenomenon, diagnosed in patients with a normal IRP and failed peristalsis (DCI<100 mmHg/cm/s). This disorder is often observed in patients with systemic connective tissue diseases (systemic sclerosis) and predisposes to the development of GERD. Detection of lack of contractility is clinically important in patients undergoing surgical treatment (fundoplication, bariatric surgery). In patients with a lack of contractility, surgical interventions are contraindicated due to the high likelihood of developing postoperative dysphagia.
Distal esophagospasm. Distal spasm of the esophagus is better known as diffuse esophagospasm. It is diagnosed by premature contraction of the thoracic esophagus (DL<4.5 s) and normal mean IRP values. Premature contractions with DL less than 4.5 s are associated with symptoms such as dysphagia and chest pain. Thus, distal latency is the most important indicator in the diagnosis of esophagospasm.
Hypercontractile esophagus ("jackhammer" esophagus). In traditional manometry and in early versions of the Chicago classification, there were several different diagnosis formulations for increased amplitude esophageal peristalsis, such as “nutcracker esophagus” and hypercontractile esophagus. However, an isolated increase in the amplitude of the peristaltic wave is usually not associated with symptoms and can be detected in healthy people. For this reason, a new parameter was introduced to measure the force of peristalsis of the thoracic esophagus - the distal contractile integral (DCI). Initially DCI≥5,000 mmHg. Art. / cm/s was identified as a variant of motor impairment. However, the results of the study showed that DCI≥5,000 mmHg. Art./cm/s, but <8,000 mmHg. Art. / cm/s also occurs in healthy people. These contractions are spastic in nature. They are accompanied by severe chest pain and dysphagia. Thus, hypercontractile esophagus was defined as an increase in DCI≥8,000 mmHg. Art. / cm/s at normal average IRP values. The most effective treatments for hypercontractile esophagus are surgical interventions used to treat achalasia.
Minor disturbances of peristalsis
May be detected by MVR in asymptomatic patients. Characterized by a decrease in intensity (DCI<450 mm Hg / cm/s) or a violation of the structure of peristaltic waves. Minor disturbances of peristalsis are of clinical importance for patients with GERD, since in most cases they lead to impaired esophageal clearance. In addition, minor disturbances of peristalsis can serve as predictors of postoperative dysphagia in the case of antireflux operations.
Ineffective esophageal motility. Ineffective esophageal motility is characterized by DCI<450 mm Hg. Art. / cm/s at normal average IRP values. This is often accompanied by a decrease in LES pressure. These characteristics are more common in patients with GERD. However, the predictive value of these results for the diagnosis of reflux disease is insufficient. As with absent contractility, ineffective motility is important for selecting patients for antireflux surgery.
Fragmented peristalsis. MVR visualizes the contractile activity of the entire esophagus, this makes it possible to detect zones in the peristaltic wave with a lower amplitude - the so-called. pressure changes. Fragmented peristalsis is characterized by esophageal contractions with large peristaltic breaks (>5 cm) with normal DCI and IRP values. A peristaltic rupture is an area on the peristaltic wave where contractions of the muscular wall of the esophagus are absent or occur with an amplitude of less than 20 mm Hg. Art. Normally, the length of the peristaltic gap does not exceed 5 cm. Larger peristaltic gaps are associated with a more severe form of GERD.
To assess peristaltic reserve in case of ineffective motility and fragmented peristalsis of the esophagus, it is advisable to conduct additional tests: with multiple rapid sips of water (MRS, multiple rapid swallow), with solid food and voluntary drinking of 200 ml of liquid. The significance of the test with multiple quick sips is that normally, during the period of taking several sips in a row, relaxation of the UPS and LES occurs. At the same time, peristalsis of the thoracic esophagus is inhibited, but with a subsequent powerful total contraction at the end of the act of swallowing. Effective contraction of the esophageal body in this case indicates peristaltic reserve (see Fig. 4 ). The absence of peristaltic contraction after a series of sips indicates a marked decrease in peristaltic reserve, ineffective motility of the esophagus, impaired esophageal clearance and is a unique predictor of the development of dysphagia in the case of fundoplication.
Rice. 4. Assessment of peristaltic reserve of the esophagus
When performing MVR in healthy people without hiatal hernia, the legs of the diaphragm and the LES are located within the same high-pressure zone. In some patients, two separate zones of high pressure are displayed (separation of the pressure zone of the LES and crura of the diaphragm greater than 2 cm). At the same time, traditional water-perfusion manometry does not allow distinguishing between the pressure zones of the LES and the crura of the diaphragm due to low resolution. In this regard, MVR is reliable in detecting the hiatal hernia and determining its size ( see Fig. 5 ).
Rice. 5. Impaired motility of the esophagus with hiatal hernia - bifurcation of the pressure zone of the esophagogastric junction and a decrease in pressure in the LES
conclusions
- MVR is the gold standard in the diagnosis and evaluation of esophageal motor dysfunction.
- Allows you to obtain accurate quantitative and qualitative data on intraluminal pressure, coordination and motility of the esophageal muscles.
- Directly during the study, the software synthesizes a holistic picture of the motor activity of the esophagus in the form of a continuous pressure graph.
- Esophagomanometry is the main research method in the diagnosis of esophageal achalasia; it allows one to objectively determine the types of achalasia cardia. This makes it possible to predict the effectiveness of treatment and choose a more rational method of therapy for a particular patient.
- With MVR, it is possible to effectively diagnose distal esophagospasm, impaired motor function in systemic diseases, and determine the presence and size of the hiatal hernia. These data must be taken into account when planning surgical treatment of patients.
Operating principle of a water perfusion catheter
9-channel water-perfusion catheter for esophageal and pharyngeal manometry
The principle of operation of the water-perfusion catheter is that it has capillaries that open at certain points on the surface of the catheter (ports). Each capillary is connected to an external pressure sensor and a water pump, which supplies water inside the capillary at a rate of 0.5 ml/min. The change in pressure in the area of the capillary port is transmitted through a column of water to a pressure sensor and then to a recording device for graphic display. The most commonly used catheter is with four or eight capillaries.
One week before the procedure
Ask questions about your medications
You may need to stop taking some of your medications before the procedure.
Anticoagulants (blood thinners)
If you are taking a medicine to thin your blood, such as to treat blood clots or to prevent a heart attack, ask your doctor who prescribed it when you should stop taking it. The following are some examples of blood thinning medications:
|
|
Medicines for diabetes
If you take insulin or other medications for diabetes, ask the doctor who prescribed the medication what you should do the morning of your procedure. You may need to change your dose before the procedure.
to come back to the beginning
Deviations from the norm
Discrepancies with normal values, which are determined during the esophagomanometry procedure, do not always indicate pathologies of the functions of the gastrointestinal tract; sometimes the cause is other diseases. Partial relaxation of the pharyngeal valve can occur in neurological conditions: as a result of stroke, parkinsonism, polio.
Manometry of the esophageal canal is one of the methods of diagnostic examination of the digestive organs, which evaluates the coordination of wall peristalsis with the function of the pharyngeal and cardiac valves, and also measures the pressure in the esophageal cavity.
Manipulation is used to diagnose inflammatory processes, stenoses, frequent spasms, and pain. Among other possible examinations of the esophageal tube and stomach cavity, special attention is paid to manometry, since the procedure helps to examine the organ in detail.
Also, for some diseases of the digestive tube, examinations such as MRI of the esophagus (more details), ultrasound examination of the organ, impedance measurement and other tests are prescribed.
Indications for manometry
Esophagomanometry is performed in patients with symptoms that indicate their connection with esophageal pathology, such as dyspepsia, dysphagia, odynophagia, and non-coronary chest pain syndrome. In addition, a manometric study is indicated for patients before undergoing antireflux surgery and to assess the involvement of the esophagus in systemic diseases such as scleroderma, chronic idiopathic pseudo-obstruction (Table 1).
Table 1.
Main clinical indications for esophageal manometry
| Study of patients with dyspepsia | Abnormalities of the upper esophageal sphincter and pharynx Primary esophageal motility disorders (achalasia cardia, nutcracker esophagus, diffuse esophageal spasm, lower esophageal sphincter hypertonicity) |
| Study of patients with possible gastroesophageal reflux disease | Help in determining the position of the pH probe Lower esophageal sphincter pressure test Assessment of peristalsis defects (especially before fundoplication (from the Latin fundus ventriculi ) |
| Study of patients with non-cardiac chest pain syndrome | Primary esophageal motility disorders Pain response to provocative tests |
| Assessing possible esophageal involvement in systemic diseases | Scleroderma Chronic idiopathic intestinal pseudo-obstruction diabetes mellitus |
| Exclusion of esophageal etiology when anorexia nervosa is suspected |
Complications
Like any other examination, manometry can lead to some complications:
- bleeding from the nasopharynx or varicose veins of the esophagus;
- penetration of the catheter into the trachea;
- vomiting;
- fainting;
- bronchospasm;
- infectious aggravations;
- perforation of hollow organs.
We recommend: When is it possible to treat a hiatal hernia without surgery and how is it done?
Deviations that are indicated at the time of the study do not always indicate intestinal diseases. They can cause other pathologies. Inadequate relaxation of the upper sphincter often indicates a neurological disorder. This happens due to Parkinson's disease, polio and other things. And yet, the study is carried out for accurate diagnosis and subsequent correct therapy.
Features of carrying out for children
Esophagomanometry of the esophageal canal in children compared to adult patients is done less frequently. However, the increase in morbidity of the gastrointestinal tract in childhood made such a procedure possible.
- The child must be at least 4 years ;
- up to the age of ten, the examination is carried out under general anesthesia;
- the probe is inserted only orally due to the small size of the nasal passages;
- The diameter of the capillary tubes should not exceed 0.4 mm .
In children, the esophageal wall is much thinner than in adult patients, and the esophagus itself is much smaller in diameter. For this reason, insertion of a catheter into the esophageal cavity should be done with extreme caution to avoid damage to the epithelium, bleeding, and perforation of the wall.
Conducting research
The volume of the sensor in the balloons is regulated by the doctor; changing the volume changes the pressure in the esophagus up or down, the data is recorded by the sensors. Esophageal manometry helps the doctor assess the functioning of the smooth muscles of the organ.
Examination of the inferior (cardiac) valve
The sphincter is fixed in a calm state. Then, after swallowing a small volume of water, the residual pressure is assessed, sedation is assessed, and so on. At rest, the pressure is at its maximum. In order to record relaxation, the patient is injected with 5 ml of liquid . They check residual effects, the stage of relaxation, and so on.
Esophageal wall manometry
- duration of muscle contraction;
- amplitude of contractile movements, purity of compression;
- the speed of peristalsis from the upper sphincter to the lower.
Upper valve examination
- calm down time;
- pressure at rest;
- percentage of relaxation.
Sometimes during the procedure the vomiting receptors in the stomach or upper part of the esophageal tube are irritated. If anesthesia is not enough, the patient experiences a state of nausea and vomiting is possible. When such complaints appear, it is better to interrupt the study.
The procedure is performed on an outpatient or inpatient basis. Depending on the type of lesions of the esophagus and stomach, the first signs of the disease may be similar. Manometry helps to make an accurate diagnosis that indicates a specific disease.
Decoding the results
The result is recorded in the following phases: distal part, middle part, proximal part, in addition at 3 cm, 8 cm, 13 cm, 18 cm up from the cardiac valve.
Norm:
- proximal area - 2.4-3.6 cm/sec;
- distal area - 2.6-4.4 cm/sec.
The duration is fixed in seconds up from the bottom valve:
- at 3 cm – 3.9-5.1
- at 8 cm – 3.0-4.8
- at 13 cm – 2.8-4.2
- at 18 cm – 2.1-3.7
Amplitude is measured in millimeters Hg. Art.
- at 3 cm – 64-154
- at 8 cm – 50-130
- at 13 cm – 38-102
- at 18 cm – 33-90
- middle section – 60-140
Manometry - description of the procedure
Esophagomanometry is a well-known instrumental study carried out for various ailments of the esophagus, designed to determine the pressure inside the organ. The procedure is needed to establish the motor-evacuation functioning of the esophageal tube, namely the possibility of its contractions and relaxations at the required time. The manipulation is slightly traumatic - the integrity of the skin and other tissues is not damaged, the introduction of a special probe causes a person only a short-term feeling of discomfort.
This event makes it possible to establish contractile performance and the relationship of different parts of the digestive tract - from the pharynx to the lower sphincter.
A detailed study of esophageal motility through manometry becomes mandatory in preparation for surgical intervention in relation to GERD, hernias in the diaphragm, and disorders of sphincter function.
Evaluation of results
Evaluating the results of high-resolution manometry takes significantly less time than the results of traditional manometry due to good data visualization (closed loop and color indication of pressure). The result of the assessment can be both a final diagnosis and the detection of the first phenomena of pathology, such as the loss of small segments of contraction or a slight increase in pressure in the lumen of the organ.
High-resolution manometry allows for a short period of time (the procedure lasts on average 15 minutes) to conduct a highly informative diagnosis of motor function and help the doctor begin the necessary (for pathology) timely treatment. At the Research Institute of Surgery and Emergency Medicine of the First Medical University named after Academician I.P. High-resolution Pavlovian manometry is performed by experienced doctors using modern Dutch Medical Measurement Systems equipment using disposable and reusable probes from Mui Scientific, which guarantees you the accuracy, quality and safety of the study.
Manometry of the lower esophageal sphincter
With LES manometry, resting pressure is measured and its relaxation is assessed during the process of swallowing a small amount of water (percentage of relaxation, residual pressure, duration of relaxation). In addition, the location of the LES is determined (the distance to the LES from the entrance to the external nasal passage) and the total length of the LES. The normal values of these parameters are given in table. 2.
Normal values for the study of the LES.
table 2
| Parameter | Norm |
| LES resting pressure | 6-25 mmHg |
| at the end of the inhalation | 40±13 mmHg |
| average | 24±10 mmHg |
| at the end of exhalation | 15±11 mmHg |
| NPC relaxation duration | 5-12 s |
| NPC relaxation | More than 90% |
| total length | 20-40 mm |
| Location | 38-48 cm |
LES resting pressure
- the point of highest pressure of the LES, identified during manometry.
Assessment of LES relaxation
- this study is usually carried out while swallowing 5 ml of water at room temperature, since a “dry swallow” does not cause sufficient relaxation of the LES. After swallowing, LES pressure usually decreases to approximately the level of baseline gastric pressure, followed by a rise.
This evaluates:
- duration of relaxation
. - percentage of relaxation
- the % decrease in LES pressure during relaxation is estimated relative to the LES level at rest, which is 100%. - residual pressure
(the difference between the lowest pressure achieved during relaxation and the basic pressure of the stomach). Residual pressure is considered a better indicator of LES function than percent relaxation because it is independent of resting LES pressure levels. Normally, the residual pressure should be 8 mmHg. Art. and below.