Atresia (fusion, obliteration) of the intestine is a congenital pathology of the development of the child’s gastrointestinal tract, consisting in the absence of a lumen in one of its sections.
Depending on the location of the pathology, several types of atresia are distinguished:
- pyloric – located directly after the stomach;
- duodenal atresia - located at the very beginning of the small intestine;
- jejunal atresia - the area is located between the upper and lower parts of the small intestine;
- ileal atresia;
- colonic atresia - diagnosed in the area of the rectum and anus.
In a child with anal atresia, there are various variants of structure or anatomy.
- The anus may be too narrow and not in its usual place, which leads to painful emptying of the rectum and persistent constipation.
- The anus may be absent from the outside, but inside the rectum has an opening connecting it to another organ in the pelvic area - the urethra, vagina or bladder. In such cases, infections or intestinal obstruction develop. The communication between the rectum and other organs is called a fistula or fistula.
- The anus may be absent, and the rectum is connected to the organs of the urinary and reproductive systems, forming a single canal or cavity called the persistent cloaca, through which both stool and urine are excreted. Cloaca - the most complex malformation disrupts the functioning of all connecting organs and leads to infectious complications.
Causes
The main change occurs between the 5th and 10th week of embryonic life. Until the 5th week, the small intestine is a well-defined cavity lined with squamous epithelium. Subsequently, the epithelium begins to rapidly proliferate and the cavity of the digestive tube from the pylorus to the bauginian valve becomes obliterated, filled with epithelial growths and forms a solid cord. Later, individual vacuoles begin to appear between the epithelial growths, which soon connect with each other and by the 12th week the intestinal lumen is restored. One or another form of developmental arrest in the 2-3rd month of intrauterine life leads to atresia or intestinal stenosis. Stenosis appears as a result of insufficient restoration of the intestinal lumen, and atresia due to the persistence of one of the septa.
How does anal atresia manifest?
At birth, obstetricians always examine the baby and make sure that the anus is present and in its place. Newborns have their first stool within 48 hours of birth, so the presence of internal bowel abnormalities becomes apparent during this time. With rectoperineal fistula in boys and girls and in girls with rectovestibular fistula, the anomaly may be missed at birth, so the diagnosis is made late when examined for constipation.
Pathological anatomy
There are 2 forms of intestinal atresia in newborns: in some cases, only one internal diaphragm or membrane remains, which closes the intestinal lumen, and in other cases, the intestine ends in a blind sac and the intestinal tube is interrupted.
The distended proximal cord lies separately from the collapsed intestinal loops, or is connected to them by a fibrous cord. Sometimes there are multiple atresias and isolated blind areas of the intestine, connected to each other by thin cords, reminiscent of tied sausages. Proximal to the site of obstruction, due to severe dilatation of the small intestine (reaching 2-3 cm in diameter), local ischemia develops. This condition is accompanied by the risk of developing necrosis and perforation. If the obstruction is not resolved by the 3rd or 4th day, death usually occurs.
The small intestine collapsed distal to the site of obstruction, with a diameter of no more than 4-6 mm, contains some mucus and cellular elements of the mucous membrane. A collapsed colon rarely exceeds these dimensions.
What examination and when is carried out for atresia of the anus and rectum?
If any signs of intestinal abnormality are detected, an examination is carried out, including:
- An X-ray examination of the abdominal cavity shows where the rectum ends and allows us to understand whether there is an anomaly in the development of the lower parts of the spine;
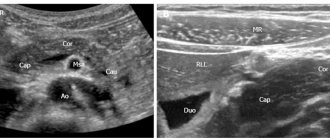
- Ultrasound examination (ultrasound) of the abdominal cavity and retroperitoneal space shows disturbances in the outflow of urine from the kidneys and bladder or abnormalities in the structure of the kidneys;
- Ultrasound examination of the spine performed during the first 3 months of life allows us to evaluate deformations and accretions of the spinal cord, which can lead to subsequent neurological disorders during growth. If ultrasound reveals abnormalities in the structure of the spinal cord, then magnetic resonance imaging (MRI) of the spine is performed. After 3 months, the information value of ultrasound for assessing the spinal cord decreases;
- Echocardiography to detect heart defects.
The duodenum is classified as a vital organ, the study of which in normal and pathological conditions is relevant for solving the problems of modern gastroenterology. Congenital malformations of the digestive system occur with a frequency of 3.4 cases per 100 perinatal autopsies, accounting for 21.7% of all developmental anomalies [3, 5]. Taking into account the anatomical, physiological and embryological characteristics of various parts of the intestinal tube, geneticists, pediatricians and surgeons consider duodenal atresia separately from atresia of other parts of the small intestine [2].
It is known that from the 4th week of intrauterine development, as a result of proliferation of the endoderm, the lumen of the duodenum is completely obliterated. As a result, the hollow tube of the primary intestine loses its lumen and turns into a cord. Later, the process of vacuolization begins: in certain areas between the epithelial cells, vacuoles appear, which merge, the process of recanalization occurs, as a result of which by the end of the 8th week the lumen of the duodenum becomes completely free [4]. If the recanalization process is disrupted, complete or membranous atresia is formed. Sometimes atresia can simultaneously occur in different places in the intestinal tube. The most common localization of atresia is in areas of “complex” organogenesis: the esophagus, duodenum, distal ileum, the junction of the small intestine into the large intestine, and the rectum.
The purpose of the study was to study the characteristics of intrauterine development, pheno- and genotypic characteristics of the ABO system and the Rh factor in newborns with duodenal atresia.
Materials and methods
68 case histories of newborns with duodenal atresia were analyzed. Observations of the membranous form of atresia were not included in the study. Medical records of newborns with Down syndrome were also excluded from the study. All newborns were operated on. 24 children died between the ages of 7 days and 2 years; pathological data were also analyzed in these observations. An analysis of the main anthropometric indicators at birth (body weight, height, head and chest circumference) and associated malformations was carried out based on laboratory data and autopsy reports. The control group was a representative sample of 607 newborns in a non-specialized maternity hospital. In 61 patients, the blood group was studied according to the ABO systems and the Rh factor. The control group consisted of data from a study of a sample of 513 apparently healthy newborns. In addition to the distribution by blood groups and determination of gene frequencies, phenotypic combinations of blood groups according to the ABO and Rh factor systems were analyzed. To determine the blood group according to the ABO system, an agglutination reaction was used using anti-A and anti-B polyclones, and to determine the blood group according to the Rh factor system, an agglutination reaction was carried out using isoimmune anti-Rh sera.
The obtained data were processed by methods of variation statistics and special genetic methods. The “relative risk frequency” indicator was also calculated - X, which was expressed in fractions of a unit. This indicator was determined by comparing the frequency of two markers (M1 and M2) in the group of patients (b) and healthy children (h):
The X value is equal to 1 if there are no differences between the compared groups; an increase or decrease in the indicator characterizes the magnitude of the risk of developing a given phenotype.
Results and discussion
Among the study group of patients there were 31 (45.5%) boys and 37 (54.4%) girls, sex ratio 0.8:1. The mean maternal age was 27 years, and the mean gestational age was 37 ± 3 weeks. Pregnancy proceeded with the threat of termination in 56% of cases. Polyhydramnios was noted in 24% of cases.
Children were admitted to the hospital at the age of 1 to 3 days of life with a clinical picture of high intestinal obstruction. When examining the newborn, a severe general condition, signs of intoxication and dehydration were noted. All children were operated on. In most cases, the site of duodenal atresia was localized near the major duodenal papilla. The part of the intestine located above the atresia and the stomach are significantly dilated; the underlying sections of the small intestine are collapsed, often significantly shortened. At various times after surgical treatment, 24 children aged from 7 days to 2 years died. The cause of death was multiple concomitant malformations and multiple organ failure.
The analysis showed that the intrauterine development of sick children is impaired. As can be seen from table. 1,
all anthropometric indicators (body weight, height, head and chest circumference) were reduced (p <0.05), which indicates intrauterine growth retardation in children with duodenal atresia. The correlation between anthropometric indicators is high (0.84-0.80), this confirms that intrauterine growth retardation is uniformly reflected in all anthropometric indicators. The variation of these signs is increased, body weight varies to a greater extent, and head circumference varies to a lesser extent.
When analyzing protocols of pathological examinations and medical histories, the presence of concomitant malformations of various organs and systems was established in 57.3% of patients. The average number of concomitant malformations in sick children was 2.02 (from 2 to 5 malformations). The presence of concomitant malformations in the majority of newborns with duodenal atresia also indicates a deviation from the normal processes of intrauterine development.
Associated developmental defects have been identified in various organ systems. Most often, duodenal atresia was combined with congenital heart defects, central nervous system defects, and various gastrointestinal defects (Table 2).
Among the heart defects, the most common were ventricular and atrial septal defects, patent ductus arteriosus, and pulmonary artery stenosis. Defects of the abdominal cavity, combined with duodenal atresia, are mainly hypoplastic in nature - pancreatic hypoplasia, absolute shortening of the small and large intestine. In 2 newborns, duodenal atresia was combined with atresia of other localizations - the colon and anus. Most of the defects in other localizations were also defects of hypoplastic origin (agenesis of the spleen, hypoplasia of the thymus, kidneys, etc.).
When studying the distribution of developmental defects according to the principle “from cranial to caudal” end of the body (see Table 2)
the largest number of defects was noted in the abdominal cavity (59.6%), more than 1/4 - in the chest area (28.1%). Defects in the head (6.8%), pelvis (4.8%) and extremities (0.6%) were less common. This distribution of defects indicates their greatest number in the cluster zone of the abdominal cavity.
When considering the genetic structure of sick and healthy children in terms of the frequency of ABO system genes, a significant increase in the frequency of the O gene and a significant decrease in the frequency of the A gene among sick children were noted (Table 3).
Also in the group of patients there was a decrease in heterozygosity (p <0.05). There were no differences in the Rh system.
Phenotypic analysis revealed a significant predominance of O (I) blood group, a decrease in A (II) blood group, as well as a tendency towards a decrease in AB (IV) blood group. When calculating the “relative risk frequency”, a high association of duodenal atresia with blood group O(I) was revealed (O:A - 2.41; O:B - 1.59; O:AB - 4.02).
For a more detailed study of the characteristics of phenotypic traits, a combination of blood groups according to the ABO and Rh factor systems was analyzed. The frequency distribution of phenotypes in the group of healthy children corresponds to theoretically expected, while in the group of patients with duodenal atresia there is a significant deviation due to an increase in the frequency of the ORh+ phenotype and a decrease in the frequency of the ARh+ phenotype (Table 4).
Thus, the data obtained indicate a significant disturbance in the intrauterine development of children with duodenal atresia, which is confirmed by a decrease in all anthropometric indicators at birth and a large number of concomitant developmental defects. A high association of duodenal atresia with blood group O (I), an increase in the frequency of the ORh+ phenotype and a decrease in the frequency of the ARh+ phenotype were also revealed.
Intrauterine growth retardation in children with this pathology was also noted by other authors; according to their data, the average birth weight is significantly reduced - 2380 g (σ = 988), while the more proximal the atresia is located, the lower the birth weight [7].
Combined developmental defects are hypoplastic in nature. It should be noted that the organs with the majority of concomitant malformations (see Table 2)
, as well as the duodenum, are derivatives of the endoderm (trachea, lungs, liver, pancreas, thymus). According to some authors, duodenal atresia is often combined with an anomaly of the pancreatic bud and terminal part of the biliary tract [5, 9]. A high incidence of concomitant malformations in children with duodenal atresia (up to 76%) was also noted by other authors [1, 7, 10—13].
Immunohistochemical studies were performed on samples from the proximal and distal duodenum of neonates with duodenal atresia in comparison with controls. It was revealed that in the proximal direction of the duodenum the number and size of nerve cells decrease, and hypoplasia of the inner muscle layer is noted [6]. Another independent study also revealed signs of hypoplasia of the muscular layer of varying severity in a similar group of patients, more pronounced in the proximal areas of duodenal atresia [8].
Conclusion
Analysis of case histories and autopsy reports of children with duodenal atresia revealed a high frequency of concomitant malformations of a predominantly hypoplastic nature. A violation of the intrauterine development of children with duodenal atresia was revealed, which is expressed in a decrease in anthropometric indicators and the presence of concomitant developmental defects. Geno-phenotypic analysis of the distribution of blood groups according to the ABO system and the Rh factor indicates an association of duodenal atresia with blood group O (I), an increase in the frequency of the ORh+ phenotype and a decrease in the frequency of the ARh+ phenotype.
How is atresia of the anus and rectum treated?
Anal atresia will always require specialized surgical treatment, but the choice of a specific operation depends on the type and severity of the defect, as well as on concomitant diseases and the general condition of the child. Usually, to unload the intestines and ensure good healing of the sutures in the place of the anus formed by the surgeon, after the birth of a child or before reconstructive surgery, a colostomy is applied. A colostomy allows you to prepare the child for reconstruction of the anus and rectum, provide care for the anal area after surgery, and can be closed after 2 to 6 weeks.
X-ray examination
With careful clinical observation, a diagnosis can be made within the first 24-48 hours. X-ray examinations should confirm the diagnosis and help locate the defect. X-rays show a dilated duodenum or a loop of small intestine. No granular matter is visible, as with meconium ileus. If there are clinical and radiological data indicating the presence of obstruction, it is necessary to immediately perform laparatomy, without specifying the level of localization of the obstruction.
Giving a contrast mixture carries a certain risk: if the mixture thickens, it can close the intestinal lumen, and if vomiting occurs, aspiration may occur. Therefore, it is given in a liquid solution, after the examination it is removed, and the stomach is washed with a urethral catheter. In atresia, the proximal loops of the small intestine are swollen, and the distal portions of the intestine contain neither gas nor contrast agent. With low-lying atresia of the small intestine, there are a large number of distended intestinal loops and it is impossible to differentiate this obstruction from obstruction of the large intestine.
Irrigoscopy should not be performed before laparatomy, and 2-3 days after it - after ileostomy to check the patency of the large intestine. Free fluid found in the peritoneal cavity during radiography may be a consequence of intestinal perforation or exudation of the serous surface of a blocked intestine.
If the intestine ruptures before birth and the hole is closed, sterile peritonitis may develop with small calcifications scattered throughout the abdominal cavity.
Is it possible to completely restore intestinal function with surgery?
Obviously, with a successful combination of circumstances, which include a favorable form of the defect, the experience and skills of the surgeon, the equipment of the clinic, careful preparation for the operation and scrupulous postoperative care, the likelihood of a favorable result will be high. It should be taken into account that in order to achieve maximum results, the surgeon must solve the problem efficiently and on the first try. It has been proven that each subsequent reconstructive operation performed after a failed first one will have a less favorable prognosis. However, even with successful restoration of a number of intestinal functions after the first operation, important nerves and muscles responsible for the urge to empty the rectum and allow for retention of intestinal contents may be absent. Therefore, after the operation, they begin a rehabilitation program for intestinal functions, which includes elements of training and education that help children become neat.
How should you teach your child to be neat?
Developing neatness skills begins at the most appropriate age for this - about 3 years. Children born with anal atresia achieve neatness more slowly than their peers. Depending on the type of abnormality and the nature of the surgery performed, some patients have difficulty achieving bowel control and require a special training program to teach cleanliness skills. Each child has individual characteristics and therefore restorative techniques are selected taking into account these characteristics.
Folk remedies
Atresia cannot be cured using traditional methods. The only way to preserve the health, and often the life of the patient, is surgical intervention, often performed as an emergency. Refusal of treatment proposed by a doctor, delay and attempts to use folk remedies can lead to serious consequences.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
What is the prognosis for reconstructive surgery for atresia of the anus and rectum?
Good fecal retention even with a strong urge to empty the rectum (up to the appearance of constipation) is observed in children who had such anomalies as recto-perineal fistula (recto-perinal), low recto-urethral fistula (recto-bulbar) or recto-vestibular fistula fistula (recto-vestibular).
Patients with more complex anorectal anomalies, such as rectoprostatic fistula, rectovesical fistula, or cloacal anomalies, often require a rehabilitation program to help children achieve continence and tidiness.