The role of the intestines in the functioning of the human body
Many people are interested in where the human intestines are located.
?
With the help of this organ, the body gets rid of toxins and waste. All antibodies secreted by organs and organ systems are eliminated through the gastrointestinal tract during life. All digested unnecessary substances are excreted from the body along with feces. Here are the main functions of the human intestine
.
Small intestine
Anatomy of the human intestine
- read on. The section of the gastrointestinal tract that goes immediately after the stomach and is the longest section of the intestine. Due to the presence of a large number of villi, it is in the small intestine that further digestion and absorption of all useful substances that are needed to build the cells of the body take place. It also synthesizes a large number of hormones and vitamins. One of them is cholecystokinin. It is the most important hormone necessary for controlling appetite, giving a feeling of fullness and a good mood.
Colon
An important section of the gastrointestinal tract, it does not have loops, but it goes around the small intestine. It is important that there is a valve between the sections of the intestine. It is he who prevents the food bolus from returning from the large intestine back to the small intestine. The large intestine does not absorb useful nutrients; it absorbs water, electrolytes and vitamins. The main function of this section of the intestine is the formation and removal of undigested substances.
The nuances of lactase deficiency
author: T. Yu. Grozdova, MD, Vice President of the National Association of Clinical Nutrition, Head of the Editorial Board, Scientific Editor of the journal “Practical Dietetics”
Modern medicine is developing by leaps and bounds, conquering more and more new heights. Discoveries such as the development of unique drugs aimed at treating viral diseases, organ transplants, and the treatment of a number of oncological diseases recently seemed unattainable to us. However, with the rapidity of progress, automation and informatization, we forget that everything that happens to the human body is not necessarily a disease and not all symptoms of diseases need to be treated with medications. The school of domestic medicine has always been based on consistency when considering the causes of changes in the condition of a particular patient and deciding whether it is worth intervening in this process or whether it is enough to understand what happened to the body and how not to interfere with its being healthy. One of these patient conditions is the development of lactase deficiency. Before making a diagnosis, prescribing treatment and diet therapy, it is necessary to answer one very important question: is lactase deficiency a chronic disease, features of the functioning of the body as it grows, or something else?
In order to answer the question we have posed, it is necessary to consistently consider everything related to disorders of the membrane digestion (hydrolysis) of milk sugar - lactose. Particular attention should be paid to the basis for making a diagnosis - a correctly collected anamnesis (the patient’s attitude towards a particular nationality, hereditarily established lifestyle, the state of the organs and systems of the body). And yet, we should never forget that the nature of the life activity of the human body is much more complex than what we know about the processes occurring every second in the human body.
In this article we will answer many questions: why does a person need lactose so much, why exactly membrane digestion makes it possible for the born organism to quickly grow and develop, when in addition to the digestion processes at the level of membrane complexes of glycocalyx enzymes, cavity digestion comes. It is important to know the answers to them in order to make the right decision about the need to use medications and correctly prescribe diet therapy.
From the history of medical issues
In the last century, the Russian scientist, academician of the USSR Academy of Sciences A. M. Ugolev made an epoch-making scientific discovery that changed the strategy and tactics of diagnosis and treatment in gastroenterology. He discovered membrane digestion - a universal mechanism for breaking down nutrients into elements suitable for absorption. A. M. Ugolev’s work “Parietal (contact) membrane digestion” was awarded the State Prize and was included in the register of discoveries of the USSR under No. 15 of December 1958. For his scientific work, the academician was awarded the Order of the Red Banner of Labor and the gold medal named after I. I. Mechnikov, received the prize named after. I. P. Pavlova of the USSR Academy of Sciences (1963), nominated for the Nobel Prize in Physiology and Medicine. Thus began the development of a new direction in medicine - the study of disorders of parietal membrane digestion. One of the forms of violation of parietal membrane digestion is lactose intolerance. In the International Classification of Diseases ICD10, this disease is listed under code E73.
Class: diseases of the endocrine system, nutritional disorders and metabolic disorders.
Block: metabolic disorders.
E73. Lactose intolerance:
E73.0. Congenital lactase deficiency.
E73.1. Secondary lactase deficiency.
E73.8. Other types of lactose intolerance.
E73.9. Lactose intolerance, unspecified.
Lactose intolerance is a condition caused by a decrease or complete blocking of the breakdown of lactose (milk sugar) in the small intestine due to a decrease in the activity (or complete absence) of the enzyme lactase-phlorisin hydrolase in the enterocytes of the mucous membrane of the small intestine and manifested by malabsorption syndrome. Malabsorption syndrome is understood as a complex of clinical manifestations resulting from disorders of cavity and parietal membrane digestion, transport mechanisms and the absorption process in the small intestine, leading to changes in metabolism. Concepts such as “maldigestion”, “malabsorption” and “malnutrition” are combined into a single term - “malabsorption”. Various pathological processes can lead to the development of this condition.
Lactose is important for our body. If at an early age this carbohydrate remains the main donor of energy for the body, then such functions as ensuring effective absorption of calcium and other minerals in the intestine, creating favorable conditions for the reproduction and functioning of lactic acid bacteria in the intestine, indicate the need for milk sugar in food composition. products consumed by a person in the process of his life.
Lactose (from Latin lac, gender lactis - milk) - milk sugar, C12H22O11, a disaccharide formed by residues of D-galactose and D-glucose;
exists in the form of a- and b-forms. Lactose is present in the milk of all mammals in free form (2-8.5%), and is also part of oligosaccharides, glycolipids, and glycxproteins; found in pollen tubes of some plants. Source: “Great Soviet Encyclopedia”, M., 1969-1978.
Lactose and food
Lactose is the main source of energy for children in the first months of life. In breast milk, this carbohydrate accounts for over 80% of the total amount of carbohydrates. Lactose covers 40–45% of a child’s daily energy needs.
In the daily diet of children of older age groups and adults, dairy products make up at least 30%.
Lactose is found in many natural and processed foods. Lactose obtained from whey using membrane technology and drying is used to improve the taste of products in the dairy industry, in the production of baby food products, and in the confectionery industry to improve the quality of the base of caramel, marmalade, glaze and sweets. The addition of lactose to sweets and marmalade leads to their increased viscosity, causing a pleasant chewing sensation. Lactose added to biscuits, jams, and chocolate acts as a flavoring agent and flavor enhancer. To obtain a golden crust and increase the volume of the product, lactose is added to baked goods. In the production of meat products, lactose is used to increase shelf life and reduce unpleasant tastes. Even in the alcohol industry, lactose has found use to enhance and at the same time soften the taste of an alcoholic drink and reduce the negative consequences of an overdose.
This carbohydrate is also used in large quantities in the pharmaceutical industry. Lactose is used as a base for many medications, particularly in the production of laxatives such as lactulose.
Lactose is also added as a filler in the production of biologically active additives (BAA) to food, including those used for the prevention and treatment of dysbiosis.
When forming the diet of a patient with lactase deficiency, as well as when prescribing medications and dietary supplements, the doctor is obliged to pay attention to the composition of food products, confectionery products and the composition of medications, dietary supplements!
In order for lactose to be quickly and efficiently absorbed by our body, the enzyme lactase is necessary. With its help, lactose is broken down into simple sugars - glucose and galactose - and in this form is quickly and easily absorbed in the membrane digestion system. Various forms of lactose deficiency are associated with the presence of congenital or acquired enzyme deficiency or with decreasing activity of the lactase enzyme with age.
It was discovered that in higher animals, in addition to the previously known types of digestion (cavity and intracellular), there is digestion on the outer surface of intestinal cells - parietal (contact) digestion.
The latter is carried out under the influence of enzymes adsorbed from the chyme and intestinal enzymes themselves, fixed on the outer surface of the intestinal epithelium in the brush border formed by microvilli. Parietal digestion occupies an intermediate position between cavity digestion and absorption and is characterized by a number of features compared to previously known types of digestion. Thanks to parietal digestion, the final stages of the breakdown of proteins, carbohydrates, etc. are carried out. Extremely favorable conditions are created for the absorption and sterility of the final stages of the breakdown of nutrients.Source: A. M. Ugolev, 1958
A little physiology
In connection with the discovery of membrane digestion by A.M. Ugolev in the late 1950s. the classical two-phase system of assimilation of nutrients (extracellular digestion - absorption) was replaced by a three-phase system: extracellular digestion - membrane digestion - absorption.
In the small intestine, there are two types of digestion - intracavitary and parietal (contact, membrane). The process of hydrolysis of nutrients begins with intracavitary digestion: under the influence of enzymes, mainly from the pancreas, large molecules of proteins, lipids and carbohydrates are hydrolyzed into smaller molecules: polypeptides, oligomers, dimers. Next, the digestion process moves to the stage of parietal digestion, all processes of which occur with the participation of microvilli of the small intestine, which create a large adsorption surface during the hydrolysis of nutrients. Membrane digestion occurs at the boundary of the extracellular and intracellular environments and has a number of features of both extracellular and intracellular digestion. In humans, membrane digestion is carried out mainly in the small intestine by enzymes associated with the structures of the membrane of intestinal cells.
The main problems arising from consuming lactose are related to a deficiency of the lactase enzyme. When this enzyme is inactive or the amount secreted by the intestinal wall is insufficient, then lactose is not hydrolyzed and, accordingly, is not absorbed. At the same time, feeding with milk ensures the maintenance of homeostasis in the body of newborn children, especially in the first time after birth. During this period of life, the penetration of macromolecules of mother's milk into the internal environment of the newborn organism occurs almost unhindered by endocytosis.
Research data
Very interesting data on the prevalence of primary lactase malabsorption in adults among various ethnic groups is presented in reviews of studies by Semeza (1981), Nasrallah (1979), Frolkis (1989).
| Ethnic group | Prevalence of lactase malabsorption (%) |
| People engaged in hunting and harvesting crops | 86 |
| Agricultural people from traditional non-dairy farming areas and their relatively unmixed descendants | 90–97 |
| People engaged in agriculture from traditional areas not associated with dairy farming, but who migrated relatively recently to a neighboring area where they consumed milk | 88 |
| Pastoral people who consumed milk and lactose-rich dairy products over a long historical period and lived under diet-related stress, and their relatively unmixed descendants | 11–18 |
Wisdom of nature
Academician A. M. Ugolev in his work “The Theory of Adequate Nutrition and Trophology” (1991) noted an interesting relationship: “To understand the biological role of milk, it is important to keep in mind that the presence of lactose in it, combined with the presence of lactose in the mucous membrane of the small intestine the corresponding enzyme (lactase), ensures control of the trophic relationship between mother and offspring. This trophic connection is broken when the growing organism reaches a certain degree of maturity and lactase in its intestines is repressed. The result of this is a rapid decrease in milk tolerance and a refusal to consume it. Thus, and this cannot but cause admiration for the wisdom of nature: one of the most perfect food products - milk - also contains a “limiter”, which under natural conditions, as soon as milk ceases to be vital for the mature offspring, interrupts the mechanism that depletes the mother nutrition of offspring. It is now established that repression of lactase is controlled by the hypothalamic-thyroid axis, dysfunction of which prevents repression of this enzyme.”
Epidemiology
According to Yu. G. Mukhina (2007), lactose tolerance is primarily determined by the presence of the activity persistence gene (LCT*P), the frequency of which in humans varies widely depending on the population. In the European population, the highest frequency of the LCT*P gene is observed in residents of Northern Europe (Sweden, Denmark, Ireland). The frequency of lactase deficiency in Russian people is observed in 16% of the population. According to studies, the prevalence of lactose intolerance, for example, in Latvia is 24%, Lithuania - 37%, Mari El - 81%, Karelia - 11.5%.
Most often, lactase deficiency and low frequency of the persistence gene (LCT*P) are observed in the countries of the Middle East, Southeast Asia and Africa, although even in these countries there is heterogeneity of the population for the LCT*P gene.
Peoples who historically led a nomadic lifestyle and engaged in animal husbandry have a significantly higher frequency of the gene for persistence of lactase activity and are characterized by good milk tolerance.
A study by Saavedra and Perman (1989) found that during the transition from milk to mixed nutrition in children, partial or complete repression of the gene that controls lactase synthesis is observed. There is evidence that this is due to the characteristics of a particular ethnic group. At the same time, according to the European Food Safety Authority, regular intake of milk into the human body has a positive effect on the severity of lactase deficiency. When consuming a moderate amount of milk and dairy products (kefir, yogurt, cottage cheese, cheeses), the intestinal bacterial flora adapts, and the digestion of lactose is also greatly facilitated. But this is probably only possible in the absence of a complete block of lactase synthesis, i.e., congenital lactase deficiency.
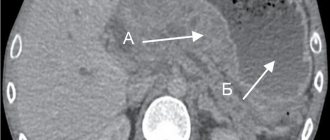
In order to understand the processes occurring in the body under conditions of possible deficiency of the lactase enzyme, knowledge of the anatomy of the small intestine and the physiology of parietal membrane digestion is necessary.
Anatomy of the small intestine
Want more new information on nutrition issues? Subscribe to the informational and practical magazine “Practical Dietetics”!
SUBSCRIBE
The wall of the small intestine is universal. Each lining of the small intestine plays a role in both the digestion and movement of food.
At the same time, the ability of the mucous membrane to gather into a huge number of folds makes it possible to significantly increase the area of absorption and combination of partially hydrolyzed food components. In its structure, each shell is also universally folded:
- The mucous membrane consists of an epithelial lamina, a lamina propria, which has additional depressions in the form of intestinal crypts, further increasing the area of absorption and contact of nutrients with enzymes of the membrane layer.
- The submucosa, which consists of connective tissue, blood vessels and nerves, including the Meissner nerve plexus, located in the thickness of the muscle plexuses, the main function is only the promotion of food and the formation of intestinal peristalsis, keeping the mucous membrane in a compressed state, but also actively participating in the transfer hydrolyzed nutrients into the blood and lymph.
- The muscular coat consists of an inner circular and outer longitudinal layer of smooth muscle, with the Auerbach nerve plexus located between them. The versatility of this structure lies in the fact that due to the presence of longitudinal and circular fibers, active peristalsis is formed and the movement of the remains of food components into subsequent parts of the intestinal tube for further processing under the influence of the microflora of the large intestine.
- The serous membrane is a visceral layer of the peritoneum, consisting of dense connective tissue and covered on the outside with flat epithelium. This structure maintains the integrity of the small intestine, flexibility and increased extensibility.
Scheme 2. Functions of the small intestine
The length of the small intestine ranges from 9 to 12 m. It is divided into three sections: duodenum, jejunum and ileum. The intestinal mucosa has many folds that significantly increase the total surface area. Due to the peculiarities of the intestinal structure, the conditions for the absorption of nutrients are as good as possible.
On the folds of the intestinal mucosa there are special outgrowths - villi no more than 0.1–0.2 mm high. There are, as a rule, 30–40 villi per 1 cm2, the main function of which is the automatic contraction of macrovilli to mix and move food contents through the intestines. In the structure of the villi there are lymphatic formations in the form of lymphoid nodules, which are found only in single form in the duodenum and jejunum; in the ileum they form follicles. Also in the villi there are small blood vessels that form entire choroid plexuses. The entire structure is designed to create the most efficient absorption of hydrolyzed nutrients.
The mucous membrane is covered with microvilli to increase the adsorption surface. The number of microvilli exceeds 2000 per 1 mm2. The structure of microvilli is a porous catalyst capable of adsorbing a large number of enzymes involved in membrane (contact and wall) digestion.
Membrane digestion
Membrane digestion is ineffective in relation to large molecules. Pancreatic enzymes adsorbed on the structures of the intestinal mucosa primarily carry out the stages of hydrolysis of nutrients (carbohydrates, proteins, fats, vitamins, etc.), membrane enzymes - mainly the final stages of their breakdown. Membrane digestion is also integrated with the processes of cavity digestion and absorption. Moreover, intestinal enzymes themselves and membrane transport systems can form enzyme-transport complexes, due to which hydrolysis products receive advantages during absorption. Under certain conditions, membrane digestion becomes the dominant mechanism, which, in particular, is observed in the small intestine of mammals during the period of their milk feeding.Source: “Theory of adequate nutrition and trophology”, A. M. Ugolev, 1991
Physiology of parietal membrane digestion
The process of digestion of food occurs not only in the cavity of the small intestine, but also in the immediate vicinity of the villi (parietal membrane digestion) and inside the cells of the mucous membrane (intracellular digestion).
A number of experimental studies have proven that fairly large parts of protein molecules are absorbed in the intestines and this is a certain protective reaction of the body and constant stimulation of the immune system. Parietal digestion is successfully combined with the processes of absorption of monomers in the intestine, which, being on the membrane of the intestinal mucosa, are instantly transported into the blood and lymph.
Based on the foregoing, it is possible to clearly determine the role played by the state of the small intestine in normal and pathological conditions. The small intestine performs excretory, secretory, motor and absorption functions. The implementation of each of them is completely interconnected, and the violation of one of them entails changes in the functioning of the small intestine and the development of either functional or chronic diseases with the further formation of protein-energy deficiency.
The main disorders in the presence of lactase deficiency and the corresponding clinical symptoms and syndromes develop as a result of changes in the absorption process of lactose (in the absence of its hydrolysis into galactose and glucose, complete or partial).
Suction process
Absorption is a complex biological process of penetration of substances through biological membranes from one environment to another, which is based on various types of transport. The small intestine plays the main role in this process; it receives nutrients necessary for the functioning of the body:
- in the process of absorption of substances from the intestinal cavity into the lymph and blood, an important role is played by macrovilli, which act as micropumps;
- when food enters the intestine, the macrovilli begin to contract rhythmically due to their contractile elements;
- during the contraction of macrovilli, the contents enter the lymphatic and circulatory systems;
- during relaxation of the smooth muscle muscles of the macrovilli, a vacuum is created in their cavity, active absorption of hydrolysis products and other substances from the cavity of the small intestine occurs;
- the valve apparatus does not allow the reverse outflow of contents into the macrovillus from the blood and lymphatic vessels.
If the pressure in the intestinal cavity under the influence of the muscular system increases significantly, the macrovilli, due to the contractile function of the smooth muscle fibers present in them, are pressed against the intestinal wall, and their role in the absorption of hydrolysis products from the intestine is switched off.
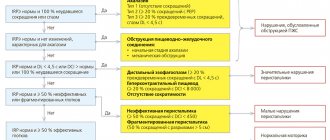
Pathogenesis of the development of the lactase malabsorption symptom complex
With lactase deficiency, undigested carbohydrates accumulate in the lumen of the small intestine, where increased osmotic pressure is quickly created, which leads to excess water entering the intestinal lumen. Macrovilli are excluded from the absorption process, which causes a disruption in the flow of all available nutrients into the blood and lymph.
At the same time, unhydrolyzed lactose is utilized by microflora, and a large amount of organic acids and carbon dioxide is formed. Clinically, this process is accompanied by severe flatulence and intestinal colic. Increased gas formation and accumulation of organic acids enhances the secretory function of the small intestine and the release of water into the intestinal lumen. In parallel, the pH level decreases, approaching the acidic side (pH < 5.5). Within a few hours, watery, foamy stools with a sour, fermentative odor are formed.
The liver and the activity of its enzymes involved in detoxification play a major role in the development of toxic effects. At this stage of development of the entire symptom complex, its further development depends on the activity of compensatory mechanisms: increased activity of membrane, lysosomal and mitochondrial enzymes in the colon and the effectiveness of the liver in neutralizing toxic products from the intestine.
Milk intolerance
Thus, lactase deficiency is a special case of food intolerance, or intolerance. However, unlike other types of intolerance, this one affects hundreds of millions of people. This problem is relevant both in childhood and in older ages. That is why there are two main types of lactase deficiency:
Primary lactase deficiency.
Primary lactase deficiency is associated with a congenital decrease in lactase activity with a morphologically intact enterocyte. The following variants of primary lactase deficiency are distinguished:
- congenital (genetically determined);
- adult type (constitutional);
- transient, observed in premature and immature children at the time of birth.
During the neonatal period, the lactase enzyme, which promotes the absorption of lactose entering the body with milk, is produced in sufficient quantities. The maximum peak of lactase synthesis occurs in the second to fourth month of life. From the first year of life, lactase activity progressively decreases. The main decrease in lactase synthesis activity occurs between the ages of 5 and 12 years and is a natural process.
In practice, when the level of lactase produced by the enzyme decreases with age, the body’s ability to absorb incoming lactose is preserved, only in smaller quantities. In some adults, the lactase enzyme disappears to a greater extent or even completely. This is called primary, or age-related, lactase deficiency. In some cases, this leads to complete lactose intolerance and causes unpleasant symptoms after consuming even small doses of milk or other products containing lactose.
Secondary lactase deficiency.
Secondary (transient) lactase deficiency develops against the background of various diseases of the gastrointestinal tract and concomitant extraintestinal pathology (endocrinopathy, encephalopathy, etc.). It can be caused by external factors, such as food allergies (including to cow's milk protein), or lack of treatment for a disease such as celiac disease.
Timely diagnosis of underlying diseases and lactase deficiency is quite important, since if the influencing factor disappears and the intestinal villi are restored, the ability to produce lactase is also restored.
A peculiarity of the development of lactase deficiency during the aging of the body is that, as a rule, intolerance to milk and a number of other products increases. According to the data presented in the works of Academician A. M. Ugolev, this is associated not only with an age-related decrease in the rate of synthesis of various enzymes, including lactase, but also especially with a weakening of the functions of the liver barrier.
In many cases, therapeutic effects on the liver lead to the restoration of food tolerance. Suppressing the intestinal bacterial flora always prevents lactose intolerance. Interestingly, people with the same lactase deficiency may or may not have milk intolerance. This is often determined by differences in the composition of the intestinal bacterial flora (in some individuals it does not produce toxic metabolites, in others it produces them in large quantities) and the state of the barrier functions of the liver.
Source: “Theory of adequate nutrition and trophology”, A. M. Ugolev, 1991
Therapy
Treatment of patients with lactase deficiency is also based on knowledge of the anatomy of the small intestine, the physiology of absorption processes, as well as knowledge of the pathogenesis of the development of a particular condition. To do this, it is necessary to consider several areas of therapy:
- Complete exclusion from the diet of foods containing lactose. To do this, you need to know the list of products containing this carbohydrate and the list of products that cannot contain lactose.
- Partial exclusion from the diet of foods containing lactose. This applies to cases where there is no complete block for the production of the lactase enzyme. But in any case, a major role in the development of the malabsorption symptom complex is played by the state of the body, the detoxification function of the liver and intestinal microflora. A full examination is recommended to diagnose concomitant pathologies, and at the same time it is mandatory to keep a food diary. When keeping such a diary, it is especially important to record not just the type of product, but also the amount of lactose included in its composition, and the manufacturer. This is necessary to compile a more specific list of food products that can be eaten.
- Use of products after preliminary hydrolysis of lactose. This applies to milk and dairy products, infant formula.
- Adding the enzyme lactase, which breaks down lactose (INN: Laktaza), to the diet when including foods with low levels of lactose. As a rule, these drugs are developed in the form of a dietary supplement to food as an additional source of the lactase enzyme. It is recommended to take the drug with every meal containing dairy products or lactose. The use of the lactase enzyme allows for any type of lactase
Bowel function
What does the intestine do in the human body?
? The process of digesting food begins before it enters the intestines and stomach. The beginning of this process occurs in the oral cavity. This is because food is first processed using enzymes that are secreted in the mouth. After the bolus of food enters the stomach, it is processed by gastric juice. Further digestion takes place in the duodenum. Bile and pancreatic secretions also go there. Bile can neutralize pepsin, which is found in stomach acid.
All necessary nutrients are absorbed in the small intestine. Digestion lasts approximately two to four hours. Then comes the large intestine, where water is absorbed. Then the chyme goes into the colon and only finally enters the rectum.
Food can remain in the colon for fifteen hours. During this time, all the liquid is removed, and only undigested residues remain. It is these residues that become the basis of feces. They gradually enter the rectum and are excreted from the body. Thus, the digestion process ends. Although the end of this process is an abstract concept, because it happens constantly.
bowel functions
Diseases and symptoms
Diseases of the large intestine:
- Chronic non-infectious inflammatory processes of the cecum, colon and sigmoid colon - typhlitis, colitis, sigmoiditis.
- nonspecific ulcerative colitis;
- appendicitis;
- acute intestinal infections;
- helminthiases;
- diseases of the rectum - proctitis, paraproctitis, hemorrhoids, anal fissures;
- cancer of various parts of the large intestine;
- colonic benign tumors, polyps;
- colonic obstruction caused by paralysis of smooth muscles, blockage of the intestinal lumen by a tumor, and other reasons.
Typical symptoms of chronic diseases:
- widespread aching abdominal pain;
- bloating, flatulence ;
- diarrhea, constipation , their alternation;
- pain, feeling of incomplete bowel movement after bowel movement;
- admixture of mucus, blood in the stool;
- dark “cherry” or tarry stools are a sign of intestinal bleeding.
Intestinal obstruction and other acute diseases are characterized by the patient’s severe general condition. Peritonitis (inflammation of the peritoneum) with sharp pain and tension in the muscles of the abdominal wall is possible. Intoxication is accompanied by nausea and vomiting. With intestinal obstruction, vomiting may take on a fecal character.
Chronic diseases of the large intestine, as a rule, occur against the background of dysbiosis with emaciation, anemia, vitamin deficiencies, and decreased immunity.
Differences
The main difference between the two sections of the intestine is the functions they perform. After all, the main function of the small intestine is the absorption of nutrients, and the large intestine is fecal formation. They also have different diameters, in thick ones it ranges from 4 to 9 cm, in thin ones - from 2 to 4 cm.
The color of the large intestine should be grayish, and the small intestine should be pink. The large intestine has outgrowths and protrusions. The large intestine is approximately 5.5 mm thick, and the small intestine is almost 2 times thinner. Based on all of the above, you can understand the principles by which the digestive system works. Now you know where the intestines are in women
, and what functions it performs.





![Rice. 1. Biopsychosocial model of the genesis of functional gastrointestinal diseases [1].](https://zakam.ru/wp-content/uploads/ris-1-biopsihosocialnaya-model-geneza-funkcionalnyh-zabolevanij-zhkt-1-330x140.jpg)