A 37-year-old woman came to Clinic No. 1 ViTerra Belyaevo for an appointment with a gastroenterologist, complaining of a paroxysmal dry cough that worsens in a horizontal position and after eating, a sore throat, a feeling of a lump in the throat, and belching with air. From the anamnesis it is known that the above complaints have been bothering the patient for 3 months.
A 37-year-old woman came to Clinic No. 1 ViTerra Belyaevo for an appointment with a gastroenterologist, complaining of a paroxysmal dry cough that worsens in a horizontal position and after eating, a sore throat, a feeling of a lump in the throat, and belching with air.
From the anamnesis it is known that the above complaints have been bothering the patient for 3 months. Treatment by an ENT doctor, therapist (other LU) - with little effect.
To exclude gastrointestinal pathology, consultation with a gastroenterologist is recommended.
What is Helicobacter pylori?
This is a bacterium that affects the pylorus of the stomach and duodenum. The prevalence of this infection is very wide, almost 50% of the world's population is infected with the bacterium Helicobacter pylori (Helicobacter pylori, Helicobacter pylori infection, Helicobacter pylori).
Bacteria that can survive in the aggressive, acidic environment of the stomach have been known for more than 100 years, but it was only in the 1970s that the connection between these bacteria and gastritis was discovered. A more complete understanding of the influence of these microorganisms on gastrointestinal disease occurred already in the 1980s, when it was possible to isolate and cultivate a bacterium called Campylobacter pyloridis (Campelobacter pyloridis), after studying and final classification called Helicobacter pylori (Helicobacter pylori).
Helicobacter pylori is a spiral-shaped bacterium 3.5 microns long and 0.5 microns wide. In some cases, the microorganism acquires a coccoid shape.
Achalasia cardia
Modern treatment of achalasia cardia is aimed at eliminating the functional barrier in the form of an unrelaxed lower esophageal sphincter and can be carried out conservatively or surgically, and in some cases with the help of medications. And if pharmacotherapy of the present disease has a purely auxiliary value, then the question of the advantage of the first two methods has not yet been resolved in the literature. A number of authors prefer surgical intervention.
Proponents of cardiomyotomy and its modifications cite the following arguments: 1) relatively high efficiency of operations (the average percentage of “good” long-term results is 85; however, it should be noted that in the literature there are no sufficiently developed objective criteria to reliably assess the effectiveness of the surgical method of treating achalasia) ; 2) the possibility of auditing the distal esophagus to identify a malignant neoplasm. The mortality rate from surgery, according to some authors, is 1.2%.
The main arguments of supporters of cardiodilation are the completely satisfactory tolerability of the procedure by the vast majority of patients, its cost-effectiveness and relative safety. The percentage of good long-term results is quite high.
Thus, it is advisable to begin treatment of almost all patients with achalasia cardia with cardiodilation. In other words, the indications for its implementation are both newly diagnosed achalasia cardia of the first and second types, and relapses after primary treatment with this method. Recurrence of the disease after cardiomyotomy requires, first of all, the exclusion of the development of peptic stricture as a complication of the operation, which is preferably carried out in close contact with surgeons. Attempts to compensate for postoperative relapse of achalasia through cardiodilation are also acceptable. And only the ineffectiveness of conservative therapy and pronounced cicatricial changes in the cardia can be the basis for cardiomyotomy.
- Conservative treatment and pneumocardiodilation
Before pneumocardiodilation, it is necessary to conduct a thorough examination of the patient. During the examination, special attention is paid to an objective assessment of his general condition, as well as the condition of the esophagus through x-ray examination and esophagomanometry. In this case, the main parameters are the diameter of the expanded part of the esophagus, its shape, the level of fluid and food retention in it, as well as expiratory pressure in the lower esophageal sphincter, reflecting its tone. Changing these parameters is the basis for assessing the effectiveness of treatment. It is best to begin preparing the patient for cardiodilation by rinsing the esophagus through a probe with a warm 4% solution of sodium bicarbonate or a weak solution of potassium permanganate. Evacuation of stagnant contents significantly improves the patient’s well-being: the feeling of heaviness behind the sternum and regurgitation at night disappear, and the manifestations of congestive esophagitis decrease. The use of a thick gastric tube is a kind of “rehearsal” before cardiodilation and facilitates the introduction of a pneumocardiodilator at the beginning of treatment.
In most cases, intramuscular injections of 0.1% atropine sulfate solution (1 ml), 50 or 25% analgin solution (2 ml) and 1% diphenhydramine solution (2 ml) are used for premedication. The combination of drugs significantly reduces the severity of the gag reflex and salivation, as well as the intensity of chest pain caused by stretching of the cardiac segment of the esophagus during the procedure. In special cases, additional superficial anesthesia of the pharyngeal mucosa with solutions of dicaine and xylestezin is permissible. In case of concomitant diseases of the cardiovascular system, which occur in approximately 15% of all patients with achalasia cardia, premedication should be supplemented with antianginal or antihypertensive drugs according to the situation. Complete anesthesia with narcotic analgesics is impractical, since this increases the risk of not noticing in time the possibility (albeit very rare with qualified cardiodilation) of such a formidable complication of the procedure as rupture of the esophageal wall.
The requirement for maximum safety for patients is met by gradual expansion of the cardia, first with a balloon with a diameter of 30 mm at a pressure of 180 - 200 mm Hg. Art. with a gradual increase in the diameter of the balloon and the pressure in it to 40 - 50 mm and 340 - 360 mm Hg. Art. respectively. The exposure is 1 - 2 minutes. The first procedure is the most important, since the risk of esophageal rupture is greatest. The fact is that in 36.5% of patients during the first cardiodilation there is a sharp increase in pressure in the system, caused by unexpected gagging movements. Such phenomena are caused by a reflex reaction of the cardia in response to its stretching, which can be spontaneously leveled out during subsequent procedures.
Control of the position of the pneumocardiodilator balloon both during its installation and during the procedure itself is carried out radiographically. However, pneumocardiodilation is quite acceptable without X-ray control. In addition, there are situations in which X-ray irradiation of the patient is contraindicated (for example, during pregnancy).
The most important point when carrying out extensions without x-ray control is determining the distance at which the probe should be inserted. For this purpose, an original technique was developed based on the use of esophagomanometry. When removing an esophagomanometric probe from the stomach into the esophagus, in accordance with the nature of the change in the curve, three marks are made on its outer side: the beginning of the cardia from the stomach, the place of greatest narrowing and the transition of the cardia to the thoracic esophagus (length of the cardia). The interval between the second mark (the place of greatest narrowing) and the esophagotonograph balloon is the required distance, which is then laid directly from the middle of the expanding part of the pneumocardiodilator. We have successfully used this method to treat more than 250 patients with achalasia cardia. Excellent and good immediate results were achieved in 95.2% of patients, excellent and good long-term results - in 86.4%.
An important advantage of this technique is the reduction in radiation exposure to the patient by 30.7% of the total dose. This is especially valuable considering that many patients additionally have to undergo cholecystography, irrigoscopy, etc. during the examination.
Pneumocardiodilation without direct x-ray control of the probe position is indicated for type 1 achalasia cardia and in most cases of type 2 achalasia. Severe curvature and atony of the esophagus in advanced cases significantly complicate the introduction of a cardiodilator into the esophagus and the installation of its balloon in the cardia. In such rather rare situations, it is advisable to use the pneumocardiodilation technique under endoscopic control, which allows not only to successfully carry out the procedure, but also to avoid serious complications.
The interval between repeated procedures should be at least 3 - 4 days. If, when removing the dilator, traces of blood are found on it, then this period is increased to 5 - 8 days. In 50% of cases, longitudinal tears were found, disappearing after 6-10 days. This period determines the frequency of procedures.
Under the influence of cardiodilation, a decrease in the tone of the lower esophageal sphincter occurs due to overstretching, and possibly tears, of its circular muscle fibers. As a result, patients note a significant reduction in the symptoms of achalasia. However, the ultimate goal of treatment is not only to achieve an immediate effect, but also to ensure remission for the longest possible period. It has been empirically established that this task is feasible in the case of reduction of expiratory pressure in the lower esophageal sphincter in conventional units to 12-15 mm Hg. Art. or up to 3 - 5 mm Hg. Art. The volume of the balloon sensor significantly affects the tone of the cardiac sphincter. The given figures were obtained under different recording conditions: the first - when using a pressure gauge probe with a volume of 2 cm3 canisters, the second - when using a probe with a 1 cm3 canister volume; they are virtually identical. The lower limit of these intervals is limited by the possibility of developing cardia failure and reflux esophagitis. Maintaining residual pressure in the cardia above the specified values creates the prerequisites for the rapid occurrence of relapse of achalasia.
The effectiveness of treating this disease with cardiodilation depends not only on the degree of reduction of the tone of the lower esophageal sphincter, but also on the condition of the smooth muscles of the thoracic esophagus. As mentioned above, the function of the latter is disrupted under the influence of the immediate cause of the disease, as well as secondarily due to overload with the residual volume of food and excessive work against the cardiac sphincter that does not relax when swallowing. Thanks to cardiodilation, this functional barrier to the food bolus is eliminated, which indirectly helps restore the tone of the smooth muscles of the thoracic esophagus. Radiologically, a decrease in the diameter of the suprastenotic expansion and the appearance of a gas bubble of the stomach are noted. An esophagotonogram demonstrates an increase in the amplitude of contractions in the thoracic esophagus. However, in a number of cases, esophageal atony is not eliminated even as a result of adequately performed cardiodilatations, which is apparently due to the severity of the initial damage to the smooth muscles of the esophagus.
The immediate results of treatment of patients with achalasia cardia type 1 (according to the subjective feelings of patients) are somewhat worse than patients with achalasia cardia type 2, which is explained by the persistence of spastic contractions of the lower part of the esophagus with completely satisfactory patency of the cardia. However, long-term results are better: after a course of treatment, excellent and good long-term results were obtained in 74.7 and 50.7% of patients with achalasia cardia types 1 and 2, and after repeated courses - in 93.1 and 74%, respectively. When comparing the duration of remission with the age of the patients and the duration of the disease, it was found that after 45 years, good and excellent results decrease to 56.5%. The duration of the disease for more than 15 years reduces this figure to 28.6%, which can be explained by cicatricial degeneration of the cardia.
The percentage of good and excellent long-term results of treatment of achalasia cardia using pneumocardiodilation ranges, according to the literature, from 50-80. Our many years of experience indicate that methodically correctly performed pneumocardiodilation, including without direct x-ray control of the probe position, allows us to achieve excellent and good results in 84.4-86.4% of cases. In this case, good and excellent results mean the following: complete disappearance or significant reduction in complaints of dysphagia, reduction in the tone of the lower esophageal sphincter to the above optimal values, good passage of barium sulfate suspension from the esophagus into the stomach during X-ray examination (a short delay of a column of radiopaque suspension with a height of no more than 2-4 cm above the cardia, since its stream entry into the stomach indicates the possibility of gastroesophageal reflux), the presence of a gas bubble of the stomach.
Complications during pneumocardiodilation occur in 2.3% of cases. The mortality rate from them or during the procedure itself is 0-0.1%. Such complications include perforation or rupture of the esophageal wall with the development of mediastinitis, reflux esophagitis, peptic stenosis of the esophagus, bleeding, trauma to the pyriform sinus of the larynx, and fainting. The integrity of the esophagus also depends not only on the absolute value of the pressure in the balloon, but also on the rate of its increase. This provision has great practical significance.
The recurrence rate of severe dysphagia in achalasia cardia ranges from 5.6 to 18%. According to summary statistics, these figures vary over a much wider range - from 3 to 30%.
There are three types of such relapses. In the genesis of relapses of the first type, spastic contractions of the lower third of the esophagus are of primary importance. The second (true) type is caused by a repeated increase in pressure in the lower esophageal sphincter and is most common. Relapse of the third type is observed only in isolated cases and is associated with a progressive disturbance of peristalsis of the esophagus due to atony of its thoracic part, although the pressure in the cardia does not go beyond the limits.
According to various authors, the return of symptoms of the disease may depend on a wide variety of reasons: restoration of cardiac tone due to “depression of the automatism of myoneural connections”; iatrogenic reflux esophagitis and scars in the cardia area; an increase in serum gastrin after a course of treatment with cardiodilation due to periesophagitis and mechanical irritation of the vagus nerves; incompleteness of treatment, i.e. maintaining residual pressure in the cardia above 3-15 mm Hg. Art.
Thus, some authors explain the occurrence of relapses of achalasia by achalasia itself, others by non-compliance with certain therapeutic recommendations. In other words, if the appropriate empirically compiled instructions are followed, a relapse of the disease may not occur. It is difficult to agree with this opinion. Cardiodilation in all cases, even with excellent clinical results, is purely symptomatic. This means that this procedure does not provide a complete cure. It is incompetent to even talk about “cure with a defect.” The symptoms of the disease are eliminated for a certain period of time, depending on strict adherence to methodological recommendations (“adequate treatment”).
In other words, the reason for the resumption of dysphagia after treatment of achalasia cardia with pneumocardiodilation lies in the disease itself and is still unknown to us. Hence the question logically follows: how to deal with these relapses?! In our opinion, the approach to solving this problem should be based on two principles: firstly, on the individualization of treatment tactics when correcting relapses and, secondly, on the organization of dispensary observation of such patients.
The first position is essentially the result of dividing relapses of achalasia cardia into three types, which have practical significance when choosing the optimal method for their correction. Relapses of type 1 dysphagia (spasmodic contractions of the distal esophagus) are an indication for the use of nitrates and calcium antagonists. In some cases, repeated courses of pneumocardiodilation have a significant effect.
Patients with type 2 relapses require repeated pneumocardiodilation. However, in this case, the risk of complications after the procedure increases due to the development of cicatricial changes in the lower esophageal sphincter in a number of patients. In addition, the pressure in the cardia during relapses almost never reaches such a high level as was noted before the initial treatment. It is this circumstance that determines the tactical features of the correction of relapses of the second type: lower pressure in the dilator balloon during the first procedure (on average 140 mm Hg) and a smaller increase in pressure during subsequent dilations (on average 40 mm Hg) . The final pressure in the cylinder should not exceed 300 mmHg. Art.
For recurrent dysphagia of the third type, treatment with pneumocardiodilation is less effective. Therapy has not yet been sufficiently developed. You can use antidopaminergic drugs (metoclopramide, Raglan, Cerucal), which tonic the smooth muscles of the thoracic esophagus.
The duration of remission of achalasia cardia increases as a result of patients regularly taking medications such as minor tranquilizers, antipsychotics, myotropic antispasmodics, and anticholinergics. However, these drugs do not actively influence the tone of the lower esophageal sphincter and thoracic esophagus in achalasia cardia, since their effect is to one degree or another mediated by the autonomic nervous system. α-adrenolytics and fh-stimulants are not widely used.
Currently, the most popular drugs are from the group of nitrates and calcium antagonists. The beneficial effect of nitroglycerin on dysphagia caused by achalasia of the cardia has been known for a long time: nitroglycerin and amyl nitrite significantly reduce pressure in the cardia, but its function is not normalized. The creation of long-acting nitrates has opened up new prospects for the conservative correction of achalasia. Isosorbide dinitrate (nitrosorbide) at a dose of 5 mg significantly reduces pressure in the lower esophageal sphincter in such patients with a maximum decrease in the 10th minute. Unfortunately, the clinical value of nitrates is significantly reduced due to their side effects (dizziness, headache, tachycardia).
It is also known that fluctuations in the concentration of this ion in the blood plasma cause changes in esophageal motility. Acute hypercalcemia increases thoracic peristalsis and tones the lower esophageal sphincter. However, with achalasia cardia, no electrolyte shifts were observed.
Intravenous administration of verapamil to patients with cardial achalasia leads to a significant decrease in pressure in the cardia by an average of 31.4%, especially at the 12th minute. Nifedipine is a more active drug. When taken orally 10-20 mg (1 - 2 tablets) the degree of reduction in cardiac pressure is 35-50% with a maximum at the 60th minute. The effect of the drug depends on its dose. There was also a decrease in dysphagia and cramping pain behind the sternum when swallowing. Hemodynamic side effects are minor.
The effect of nifedipine on motility of the entire esophagus has been less studied. Scintigraphy demonstrates acceleration of food passage through the esophagus, but normalization of peristalsis does not occur. From this point of view, this drug is inferior to nitrosorbide.
In our opinion, the clinical effect of any drug, in particular Corinfar (nifedipine), for achalasia cardia depends on at least three parameters: the tone of the lower esophageal sphincter, the amplitude of contractions in the thoracic esophagus and the number of extra-swallowing contractions. The passage of food through the esophagus is carried out due to peristalsis of the thoracic part of the organ and synchronous opening of the cardia. If the reduction of the tone of the latter in this case is a positive factor, then the inhibition of contractility of the thoracic esophagus is negative. Therefore, against the background of the use of Corinfar, in some cases one can expect an increase in dysphagia, caused precisely by drug-induced atony of the thoracic esophagus. In this regard, we studied the effect of 20 mg of sublingually administered Corinfar on expiratory pressure in the cardia, the number of extraswallowing contractions in the lower third of the esophagus, reflecting its excitability, as well as on the amplitude of contractions in this area. Corinfar significantly reduces pressure in the lower esophageal sphincter and the number of extra-swallowing contractions in its lower third. The amplitude of contractions in the distal part of the esophagus does not change. It should be noted, however, that such effects of the drug are very selective and do not occur in every patient. Therefore, in order to avoid unreasonable prescription of the drug, a manometric study or at least a clinical assessment should be carried out every time.
Indications for the use of Corinfar for achalasia cardia:
- relapses of dysphagia after preliminary treatment with pneumo-cardiodilation (a means for secondary prevention);
- combination of this disease with coronary heart disease and hypertension;
- correction of esophageal dyskinesia in achalasia. It is advisable to take the drug sublingually until it is completely dissolved 60 minutes before meals.
The second most important measure aimed at reducing the number of relapses of achalasia and prolonging the period of remission is medical examination. All patients are subject to dispensary registration. In most cases, it should be carried out 2 times a year: examination by a therapist, chest X-ray, esophagomanometry, as well as other diagnostic procedures necessary at the moment.
Taking into account the peculiarities of the neuropsychic status of patients with achalasia cardia, care should be taken to organize a therapeutic and protective regime. It is necessary to recommend them a clear daily routine, an optimal combination of work and rest, daily walks in the fresh air and the use of Sundays exclusively for relaxation. Morning exercises are very useful in this regard, but without exercises with the torso tilted forward or in a lying position and without tension in the abdominal muscles, since regurgitation of stagnant contents of the esophagus and gastroesophageal reflux are possible. Gymnastics should be completed with water procedures. To prevent nocturnal regurgitation, patients with achalasia cardia are recommended to sleep with the head of the bed elevated and not to go to bed immediately after eating.
The employment of these patients also has some peculiarities. They are not recommended to work associated with frequent neuropsychic overload, on night shifts, on a rotating schedule, long business trips, as well as all types of work accompanied by bending the body or lifting significant weights.
It is advisable to pay attention to patients’ adherence to a strict diet with four or five meals a day, and more often if necessary. Frequent and small meals help reduce dysphagia and regurgitation, normalize the function of the stomach and intestines. It is necessary to eat food as slowly as possible, chewing it thoroughly. Food should not be too cold or hot: the muscles of the esophagus react to the low temperature of the contents of the esophagus with an additional spasm, while hot food can intensify the inflammatory process in the wall of the esophagus. Removal of stagnant contents is facilitated by drinking a glass of warm water after meals, which to a certain extent is a prevention of stagnant esophagitis.
The diet should be mechanically and chemically gentle. The consumption of hot seasonings, sauces, spicy foods, salty and heavily fried, as well as smoked foods is prohibited. It is advisable to limit the consumption of canned food, especially fish and vegetables, as they contain large amounts of thermally processed vegetable oil or tomato sauce.
There are also a number of foods that increase dysphagia in patients with achalasia cardia - apples, persimmons, peaches, kefir, soft bread, meat, boiled potatoes, which should not be consumed.
It is necessary, however, to note that in some cases the diet of patients with achalasia cardia is determined by their individual characteristics and habits. For example, tasty and favorite foods cause less dysphagia than those recommended by a doctor, but perceived with indifference or even disgust. In this regard, sometimes you can deviate from a strict diet and recommend foods that evoke positive emotions.
For the period of stay of patients with achalasia cardia in the hospital, a diet 1 or 5a according to Pevzner or the esophageal table type is recommended.
- Surgery
Indications for surgical treatment are the combination of achalasia with a hiatal hernia or esophageal diverticulum complicated by diverticulitis, the inability to exclude cancer of the cardiac part of the stomach, the failure of instrumental dilatation of the esophagus, as well as fresh ruptures that occurred during this manipulation. Severe diseases of internal organs with decompensation of vital functions are contraindications to surgical treatment.
The most common operation currently used for achalasia cardia is extramucosal esophagocardiomyotomy using the Heller technique. The surgical approach used is left-sided thoracotomy in the seventh-eighth intercostal space or upper median laparotomy. The first approach is preferable, as it provides a wider view of the surgical area. After opening the mediastinal pleura and mobilizing the distal esophagus from the surrounding tissues, its muscular layer is dissected longitudinally to the mucosa. The length of the incision should be at least 8-10 cm, and in the distal direction it must be extended to the muscular layer of the cardiac part of the stomach.
Mortality with this type of operation averages 1.5-3%. In 65-85% of patients it is possible to achieve excellent and good results. The disadvantage of Geller's operation is the development of reflux esophagitis in a significant part of the operated patients due to a decrease in intraluminal pressure in the area of the lower esophageal sphincter. In addition, some patients experience the development of esophageal diverticula in the area of the dissected muscles. With incomplete intersection of the muscle bundles, the frequency of relapses of achalasia cardia is very high.
To prevent the above undesirable consequences of this type of intervention, a number of surgical techniques have been proposed: closing the defect in the muscular lining of the esophagus with a strand of the greater omentum on a pedicel, a flap cut from the diaphragm, suturing the dissected muscular lining in the transverse direction, suturing a flap from the esophagus to the defect in the muscular lining of the esophagus anterior wall of the proximal stomach. It should be noted that their effectiveness in preventing the development of gastroesophageal reflux after esophagocardio-myotomy was not high enough.
A very effective method of surgical treatment of achalasia cardia is a combination of Heller's operation with Nissen fundoplication. This allows not only to eliminate achalasia, but also to reliably prevent reflux esophagitis and the formation of esophageal diverticulum. When achalasia cardia is combined with duodenal ulcer, selective proximal vagotomy is performed along with this surgical intervention. However, during this operation, a number of patients experience the development of dysphagia, which may be associated with “hyperfunction” of the fundoplication valve. In these situations, cardiodilation is indicated.
Particularly great difficulties are encountered when achalasia cardia is combined with severe peptic erosive-ulcerative reflux esophagitis and severe atony of the esophagus. In these cases, economical proximal resection of the stomach and abdominal part of the esophagus is indicated, followed by intussusception (if possible, areflux) esophagogastroanastomosis in combination with pyloroplasty. Other types of surgical interventions in such a situation are usually ineffective. It should be borne in mind that proximal gastrectomy is accompanied by a fairly high postoperative mortality due to failure of the sutures of the esophagogastric anastomosis. In the presence of a pronounced inflammatory process in the wall of the esophagus, the frequency of this complication can reach 15-25%. In this regard, the use of this type of operation should be limited to strict indications.
Esophagofundostomy, which was used for a long time for advanced forms of achalasia cardia using the Heyrovsky method, is now almost completely abandoned due to the high incidence of severe reflux esophagitis.
More favorable consequences of surgical treatment are observed in patients with type I esophageal achalasia. It should be emphasized that there is a close relationship between the effectiveness of a particular type of intervention and the degree of morphological and functional disorders of the esophagus present at the time of surgery. The best long-term results are observed in patients in the absence of pronounced irreversible changes in the motor function of the esophagus. In this regard, it is advisable to resort to surgical treatment at earlier stages of the disease, if one or two courses of drug treatment in combination with pneumocardiodilation are unsuccessful. Indications for surgical treatment for type II achalasia cardia should be expanded.
How does Helicobacter pylori survive in the acidic environment of the stomach?
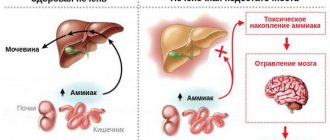
Helicobacter pylori, as a result of its vital activity, forms a cloud of alkaline environment around itself, which allows the microorganism to safely survive in the aggressive environment of the gastrointestinal tract.
In the vast majority of cases, carriage of Helicobacter pylori infection is not accompanied by any symptoms. At the same time, Helicobacter pylori infection can cause a number of problems, including extremely serious ones:
- Gastritis.
- Duodenitis.
- Stomach ulcer.
- Duodenal ulcer.
- Iron deficiency.
- Stomach cancer.
It is currently unknown why Helicobacter does not cause any problems in some people, while in others it causes serious illness.
How to determine gastric cardia insufficiency?
Nausea is a symptom of cardia insufficiency.
This pathology has quite specific clinical manifestations. The main symptoms suggesting the development of gastric cardia insufficiency are belching and heartburn.
The degree of discomfort will depend on the degree of the disease. The first degree is characterized by belching of air, the second degree is manifested by more frequent belching and protrusion of the gastric mucosa into the esophagus.
In the third degree, symptoms characteristic of esophagitis appear - heartburn, nausea, pain when swallowing, and an unpleasant taste in the mouth. What symptoms should cause concern in the patient and may indicate cardiac insufficiency? These symptoms include:
- belching air with a sour smell;
- feeling of fullness in the stomach;
- constant heartburn;
- nausea, vomiting;
- pain and rumbling in the abdomen;
- burning behind the sternum.
Most patients do not complain of lack of appetite, but may notice apathy, lethargy, and weakness. If there is pain in the abdominal area, which may indicate superficial gastritis or an ulcer, then these diseases should be excluded first. Cardiac failure is often manifested by increased gas formation.
It should be said that the pathological condition of the sphincter is not in all cases an independent disease. It can also be a manifestation of other diseases of the gastrointestinal tract. Patients with hiatal hernia have similar symptoms. With a hernia, some displacement of the sphincter occurs, which also contributes to its incomplete closure.
What is gastroesophageal reflux disease (GERD)?
When we eat, food goes down the esophagus into the stomach. The esophagus consists, among other things, of special layers of muscle that expand and contract, pushing food into the stomach through a series of wave-like movements: this is called peristaltic movements of the esophagus .
At the bottom of the esophagus, where it joins the stomach, there is a ring of muscle called the lower esophageal sphincter (LES). When food reaches the LES, it relaxes to allow it to enter the stomach, and when food passes into the stomach, it closes to prevent food and stomach acid from refluxing into the esophagus.
However, this ring of muscle is not always tightly closed, allowing stomach juices and acids to sometimes leak back into the esophagus. Most of these episodes go unnoticed because reflux only affects the lower part of the esophagus.
Acid reflux becomes gastroesophageal reflux disease (GERD) when it irritates, damages the esophagus, or causes other problems such as choking. The severity of reflux, which can cause damage to the esophagus, varies and depends on specific circumstances. But in general, the esophagus is most likely to be affected if:
- Acid often enters the esophagus.
- Gastric juice has a very low pH (that is, very high acidity).
- The esophagus cannot quickly neutralize acid.
Treatment for GERD is aimed at eliminating one or more of these risk factors..
Causes of cardia failure
The disease factor is chronic pancreatin.
The causes of insufficiency of the gastric cardia can be different. But modern medical science still identifies several main etiological factors of this disease:
- heavy physical labor or, conversely, lack of physical activity;
- poor nutrition;
- excess body weight;
- diseases of the spine, poor posture;
- physical inactivity;
- chronic diseases of the gastrointestinal tract;
- pyloric spasm;
- hiatal hernia;
- chronic pancreatitis;
- increased pressure in the abdominal cavity.
In most cases, gastric cardia insufficiency is a consequence of poor nutrition. The risk group includes those who like to eat dry food or before going to bed, as well as people who overeat or eat food irregularly. Any diseases of the stomach (especially gastritis, ulcers, neoplasms in the stomach) also contribute to the occurrence of pathology.
Obesity or incorrect posture can provoke dystopia (violation of the physiological position) of the stomach and other abdominal organs.