Cholestasis is not an independent disease, but a rather severe clinical syndrome that occurs with certain diseases of the liver, biliary tract or gallbladder. This symptom complex is characterized by a decrease or complete cessation of the outflow of bile from the intrahepatic or extrahepatic ducts.
Cholestatic syndrome is largely a problem of gastroenterology, but a dermatologist may also suspect this pathological condition, since the first manifestations of cholestasis are severe skin itching, jaundice and specific formations on the skin, such as xanthomas and xanthelasmas.
The occurrence of this syndrome is possible at any age, but men over 40 who lead an unhealthy lifestyle are at risk. In children, cholestasis is quite rare. The main cause of cholestatic syndrome in childhood is congenital malformations of the biliary system.
A separate form in medicine is cholestasis of pregnancy. It is extremely rare and tends to completely restore the functioning of the biliary system after childbirth.
Causes of cholestasis
There are many pathological factors that contribute to the development of cholestatic syndrome. The main causes of this pathology include :
- liver diseases (viral hepatitis B and C, cirrhosis);
- side effects of certain medications;
- alcohol abuse;
- liver damage from toxic substances (for example, poisoning with heavy metals, poisons);
- liver ischemia;
- chronic cardiovascular failure;
- endocrine pathology;
- autoimmune liver damage;
- poor nutrition, abuse of fatty and fried foods;
- congenital malformations of the biliary system (for example, bile duct atresia);
- cholelithiasis;
- diseases of the extrahepatic bile ducts;
- oncological diseases (for example, cancer of the tail of the pancreas);
- sepsis.
Types of cholestasis
In medical practice, the following types of cholestasis are distinguished::
- extrahepatic - a violation of the outflow of bile is associated with mechanical factors (for example, blockage of the bile duct with a stone or narrowing of the lumen due to stenosis);
- intrahepatic - is one of the syndromes in chronic liver diseases, such as hepatitis, cirrhosis.
According to the nature of the pathological process, it can be:
- spicy;
- chronic.
Symptoms of cholestasis
The following symptoms are characteristic of cholestatic syndrome:
- Severe skin itching, which intensifies at night, and during the day its intensity decreases slightly. It occurs due to retention in the body of bile salts and other substances that are excreted in bile. For quite a long time, itching may be the only symptom.
- Scratch marks on the skin.
- Skin hyperpigmentation.
- Xanthelasmas are small formations, which, as a rule, are located on the eyelids in the form of small yellowish plaques. They are slightly raised above the skin and can be located in small groups.
- Xanthomas are formations similar to xanthelasmas, but they are localized on the back and elbows. Xanthomas and xanthelasmas occur as a result of a long-term constant increase in cholesterol.
- Signs of obstructive jaundice. Due to an excess of direct bilirubin in the blood, the color of the skin becomes dark yellow, the urine acquires a specific dark color (it is described as “beer-colored urine”), and the feces become discolored.
- Dyspeptic manifestations: bloating, pain in the epigastric region and in the right hypochondrium, nausea, vomiting, loss of appetite.
With cholestasis, the intake of fat-soluble vitamins into the body is disrupted and a pathological condition such as hypovitaminosis of vitamins A, E, D, K occurs. In this case, the following symptoms may appear :
- With vitamin A deficiency: dry skin and mucous membranes, impaired twilight vision.
- With vitamin E deficiency: severe muscle weakness and decreased skin sensitivity.
- Vitamin D deficiency: frequent colds, brittle bones, muscle weakness.
- Vitamin K deficiency: increased bleeding.
The described symptoms are characteristic not only of cholestasis, but can also occur with other diseases. If you identify at least one of the listed signs, you must consult a doctor, since “self-diagnosis” in most cases is erroneous.
Causes of cholestasis during pregnancy
This form of cholestasis is known as recurrent jaundice of pregnancy. During pregnancy, liver function is impaired, which leads to the development of intrahepatic cholestasis. Symptoms of intrahepatic cholestasis in pregnancy are generalized itching and jaundice. Sometimes dark colored urine is observed. The very first symptom is intense itching of the skin with cholestasis, which occurs in the second or third trimester. The condition completely resolves after delivery, but the tendency to recur remains when taking oral contraceptives, as well as during subsequent pregnancies.
Indicators of a biochemical blood test for cholestasis in pregnancy: the bilirubin level usually does not reach 100 µmol/l (6 mg%), amounting to 34-86 µmol/l (2.5 mg%). The activity of alkaline phosphatase increases significantly, while other biochemical indicators of liver function are close to normal. Clinical, biochemical and morphological changes usually return to normal within 7-14 days after birth.
The cause of cholestasis during pregnancy is the increased sensitivity of the liver to hormonal changes. The disease is benign and does not require treatment. Cholestasis in pregnancy is associated with an increased risk of stillbirth, so the fetus should be closely monitored once diagnosed.
Diagnosis of cholestasis
After a detailed history collection and a thorough examination, the doctor may suspect this pathological syndrome. But in order to identify the cause of its occurrence and determine the severity of the disease, a specialist may prescribe additional laboratory and instrumental diagnostic tests :
- general clinical blood and urine tests;
- coprogram;
- blood chemistry;
- determination of markers of autoimmune liver damage;
- liver biopsy;
- Ultrasound of the abdominal organs;
- endoscopic retrograde cholangiopancreatography;
- percutaneous transhepatic cholangiography;
- CT (computed tomography);
- magnetic resonance cholangiography.
Cholestasis: pathophysiological mechanisms of development, diagnosis and treatment
The article presents the classification, etiology and mechanisms of development of cholestasis.
An algorithm for the differential diagnosis of cholestatic diseases is considered, which consists of a rational sequence of actions by the doctor depending on the results of laboratory and instrumental methods of examining patients with cholestasis.
A tactic for managing patients with cholestasis based on specific and nonspecific treatment methods has been proposed.
Rice. 1. Classification of cholestasis depending on the causes of development
Rice. 2. Scheme of morphological changes in patients with cholestasis (Adapted from [5].)
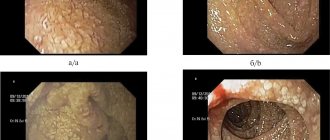
Rice. 3. Hepatocellular, canalicular and ductular cholestasis
Rice. 4. Algorithm for differential diagnosis of cholestatic diseases
Rice. 5. Treatment of cholestatic syndromes
Rice. 6. Effect of ursodeoxycholic acid on cholangiocytes (Adapted from [10].)
Cholestasis is insufficiency of bile secretion due to disruption of its production by liver cells (hepatocytes) or cessation of bile flow through the bile ducts up to the duodenal papilla. With cholestasis, a decrease in the canalicular flow of bile, hepatic excretion of water and/or organic anions (bilirubin, bile acids), accumulation of bile in hepatocytes and biliary tract, retention of bile components in the blood (bile acids, lipids, bilirubin) are observed. Long-term cholestasis (for several months/years) leads to the development of biliary cirrhosis [1, 2, 3, 4]. According to the anatomical division, cholestasis is classified as intrahepatic (intrahepatic) and extrahepatic (extrahepatic).
Intrahepatic cholestasis syndrome is caused by disruption of the vital functions of bile formation and excretion under the influence of drugs, infectious agents, as well as due to autoimmune, metabolic or genetic factors. Causes of extrahepatic cholestasis include common bile duct stones, cancer of the pancreas and papilla of Vater, cholangiocarcinoma, benign bile duct strictures, and bile duct infections. Benign bile duct strictures and cholangiocarcinoma may cause bile duct obstruction in primary sclerosing cholangitis (PSC).
Diagnosis of extrahepatic cholestasis, usually caused by obstruction of the extrahepatic bile ducts as a result of developmental abnormalities, prolonged spasm or the presence of stones, does not cause significant difficulties, while identifying intrahepatic cholestasis requires a complex of studies. The causes of the development of cholestasis syndrome can be conditionally divided into 2 groups: impaired formation of bile and/or impaired flow (excretion) of bile (Fig. 1).
In patients with cholestasis in the advanced phase, a number of histological changes occur: dilation of bile capillaries; disappearance of microvilli on the canalicular membrane; formation of bile blood clots in bile capillaries; damage to cell membranes, leading to increased permeability; violation of the integrity of tight junctions and paracellular regurgitation of bile into the blood; bilirubinostasis, formation of hepatic rosettes; proliferation of ductules in the portal tracts; periductal edema and sclerosis; periportal and mesenchymal inflammation; biliary infarctions; development of microabscesses; apoptosis; formation of xanthoma cells (Fig. 2).
Etiology and mechanisms of development of cholestasis
The etiology and mechanisms of development of cholestasis are multifactorial. Extrahepatic cholestasis develops with mechanical obstruction of the main extrahepatic or main intrahepatic ducts. The most common cause of extrahepatic cholestasis is common bile duct stones. Intrahepatic cholestasis is characterized by a decrease in bile flow and its entry into the duodenum in the absence of mechanical damage and obstruction of the extrahepatic biliary tract.
Intrahepatic cholestasis may be associated with a violation of the mechanisms of formation and transport of bile at the level of hepatocytes as a result of hepatocellular pathology, result from damage to the intrahepatic ducts, or a combination of both. Accordingly, intralobular cholestasis is distinguished, caused by damage to hepatocytes (hepatocellular) and tubules (canalicular), as well as extralobular (ductular), associated with damage to the intrahepatic bile interlobular ducts (Fig. 3) [6, 7, 8].
Hepatocellular and canalicular cholestasis can be caused by viral, alcoholic, drug, toxic liver damage, congestive heart failure, metabolic disorders (benign recurrent intrahepatic cholestasis, cholestasis of pregnancy, cystic fibrosis, alpha-1-antitrypsin deficiency). In the pathogenesis of intralobular cholestasis, dysfunction of the basolateral and canalicular membranes plays an important role.
This phenomenon may be based on disorders of hepatobiliary transport, such as mutations in transporter protein genes and acquired dysfunctions of transport systems, causing disruption of canalicular or cholangiocellular secretion. Hepatocellular accumulation of toxic cholephilic compounds causes multiple disturbances in the expression of hepatocellular transporters. In addition, the deficiency of specific bile components caused by dysfunction of transport proteins reveals the toxic potential of other bile components.
Ductular cholestasis occurs in primary biliary cirrhosis (PBC), PSC and secondary sclerosing cholangitis (SSC), biliary atresia, Caroli disease and other diseases. In most of these diseases, there is a disruption of biochemical processes in the hepatocyte, such as transmethylation and transsulfurization (resulfidation). As a result of inhibition of transmethylation reactions in hepatocellular membranes, the content of phospholipids decreases, the activity of Na+-, K+-ATPase and other transport proteins decreases, which impairs the fluidity of the membranes, as well as the uptake and excretion of bile components.
Disruption of transsulfuration reactions reduces cellular reserves of thiols and sulfates (glutathione, taurine, etc.), which are the main detoxifying substances in relation to endogenous and exogenous xenobiotics, including bile acids, and also have a pronounced antioxidant effect. Their deficiency ultimately causes cytolysis of hepatocytes during cholestasis of any origin. Ductular cholestasis develops as a result of damage to the epithelium of the bile ducts and disruption of their patency, in some cases with impaired metabolism of bile acids, as well as changes in their composition.
Algorithm for differential diagnosis of cholestatic liver diseases
It is not always possible to distinguish between types of cholestasis based on clinical symptoms and biochemical parameters. It is extremely important to distinguish between extra- and intrahepatic cholestasis using a diagnostic algorithm. Figure 4 shows an algorithm for the differential diagnosis of cholestatic diseases by identifying the presence of markers of autoimmune liver diseases: antimitochondrial antibodies (AMA), antinuclear antibodies (ANA) and antibodies to smooth muscle cells (ASMA). A positive AMA result is considered to be a titer greater than 1:80 in women over 40 years of age with PBC confirmed by liver biopsy. If the AMA result is negative, the presence of a positive response to ANA is clarified by performing endoscopic retrograde cholangiopancreatography (ERCP); in the presence of clinical manifestations, magnetic resonance cholangiopancreatography (MRCP) and computed tomography (CT) are performed. MRCP is a modern non-invasive alternative to ERCP.
Sometimes a combination of them is possible to clarify the diagnosis. CT cholangiography is also a non-invasive technology; it makes it possible to visualize the biliary tree in 36% of patients for whom other instrumental studies cannot be performed. CT cholangiography with intravenous contrast has a high risk of adverse reactions, including anaphylaxis and sudden death, which limits the use of this technique. If there is pathology identified by PSC cholangiography and the possibility of HIV cholangiopathy, it is necessary to monitor laboratory and clinical tests over time. If ERCP is normal, a liver biopsy is performed. The presence of minor changes in the biliary tract requires differential diagnosis between AMA-negative patients with an unchanged cholangiogram and AMA-negative patients with PBC or autoimmune cholangitis, manifested by the presence of a diagnostic titer of ANA and/or ASMA. The prospects for a liver biopsy depend on the lesions of the small bile ducts in: PSC; idiopathic ductopenia; granulomatous cholangitis; Hodgkin's lymphoma [9]. The absence of changes in the small biliary ducts requires differential diagnosis of diseases such as:
- drug cholestasis;
- recurrent hepatic cholestasis;
- viral hepatitis;
- autoimmune hepatitis;
- systemic diseases.
Treatment of patients with cholestasis
Treatment of patients with cholestasis can be divided into specific episodic and nonspecific symptomatic (Fig. 5). The drug of choice for nonspecific treatment of patients with cholestasis in many cases is ursodeoxycholic acid (UDCA) [9, 10, 11]. UDCA (Ursosan) is a hydrophilic bile acid, which is likely to be highly effective, since it reduces the sensitivity of hepatocyte membranes to the toxic effects of endogenous hydrophilic bile acids. It also reduces the reabsorption of bile acids in the distal ileum and regulates tubular transport, which explains the decrease in blood bilirubin levels under its influence (Fig. 6). UDCA was studied in the early 1980s, and to date there have been at least 16 controlled randomized clinical trials on its effectiveness in liver disease. For cholestatic liver diseases of various origins, the average daily dose of UDCA was 12–15 mg/kg body weight. Depending on the severity of the disease, the daily dose was increased to 20–30 mg/kg body weight in 2–3 doses. Therapy lasted from 6 months to several years [10].
Mechanisms of action of the drug Ursosan
1.
Anti-apoptotic. Ursosan, through activation of epidermal growth factor receptors, causes reactions in hepatocytes aimed at cell survival, thus causing an anti-apoptotic effect. The drug inhibits the release of cytochrome C from mitochondria and the launch of the caspase cascade.
2.
Antifibrotic (prevents the development of liver fibrosis):
- reduces the release of cytochrome C, alkaline phosphatase and lactate dehydrogenase;
- suppresses the activity of stellate cells and perisinusoidal collagen formation.
3.
Anticholestatic (eliminates all types of intrahepatic cholestasis):
- reduces the concentration of bile acids toxic to the liver cell by activating Ca-dependent alpha protein kinase and stimulating exocytosis in hepatocytes;
- induces choleresis, rich in bicarbonates, which leads to an increase in the passage of bile and the excretion of toxic bile acids through the intestines.
4.
Hypocholesterolemic (reduces cholesterol in the blood):
- reduces the absorption of cholesterol in the intestine;
- reduces cholesterol synthesis in the liver;
- reduces the excretion of cholesterol into bile.
5.
Immunomodulatory (reduces autoimmune reactions against liver and bile duct cells and suppresses autoimmune inflammation):
- reduces the expression of histocompatibility antigens: HLA-1 on hepatocytes and HLA-2 on cholangiocytes;
- reduces the formation of cytotoxic T-lymphocytes sensitized to liver tissue, reduces the “attack” of immunocompetent Ig (primarily IgM) liver cells;
- reduces the production of pro-inflammatory cytokines (interleukins IL-1, IL-2, IL-6, TNF-alpha, interferon-gamma).
6.
Litholytic (dissolves cholesterol stones in the gall bladder, prevents the formation of new stones):
- reduces the lithogenicity of bile;
- stimulates the release of cholesterol from stones into bile.
7.
Choleretic (increases bile secretion):
- stimulates exocytosis in hepatocytes;
- induces bicarbonate choleresis, enhances the excretion of hydrophobic fatty acids into the intestine.
8.
Cytoprotective (protects the cells of the bile ducts and epithelial cells of the mucous membrane of the stomach and intestines from aggressive factors):
- is integrated into the cell membranes of cholangiocytes and epithelial cells, stabilizing their structure;
- forms mixed micelles with toxic bile acids (chenodeoxycholic, lithocholic, deoxycholic) and prevents their damaging effect on cells.
Thus, the pathophysiological mechanisms of the development of cholestasis are multifactorial and interrelated; the diagnosis of cholestatic liver diseases can be carried out according to the proposed algorithm, which is based on the principle of step-by-step exclusion of the most likely causes of cholestatic diseases. The success of treatment of patients with cholestasis depends on a timely diagnosis and the use of first-choice drugs that eliminate or weaken the pathogenetic mechanisms of cholestasis development. The most studied and often used for the treatment of patients with cholestasis are ursodeoxycholic acid preparations, which include Ursosan.
Treatment methods for cholestasis
Independent attempts to treat this pathology can cause even more harm and worsen the patient’s general condition. Only a doctor, after determining the cause of cholestatic syndrome, can prescribe adequate treatment. The following methods can be used :
- Diet therapy. If you have cholestasis, you need to limit neutral fats in your diet. Instead, vegetable fats are included in the diet, since their absorption occurs without the use of bile acids.
- Drug treatment. Hepatoprotectors, cytostatics, vitamin preparations, antioxidants, choleretic agents, etc. may be prescribed.
- Surgery. Prescribed when it is impossible to eliminate cholestasis with medication. The following surgical interventions can be used: anastomosis, external drainage of the bile ducts, cholecystectomy.
During the rehabilitation period, physiotherapeutic procedures, physical therapy and massage have a positive effect.
Signs of liver cholestasis in a child
Cholestasis and jaundice in newborns usually occur in the first two weeks of a baby's life. Cholestasis is diagnosed by an increase in total and direct bilirubin. Diagnosis of chronic cholestasis includes determination of albumin, liver enzymes, fractionated bilirubin in blood serum, PT/APTT. Diagnostic evaluation for neonatal cholestasis is then necessary.
Signs of liver cholestasis in a child are icteric infants, hepatomegaly (enlarged liver), dark urine and acholic (discolored) stool. In neonatal cholestasis, primary insufficiency of bilirubin excretion leads to a decrease in the content of bile acids and their salts in the gastrointestinal tract, as a result of which the absorption of fats and fat-soluble vitamins (A, D, E, K) is impaired. This leads to vitamin deficiency and growth impairment.
Specific treatment depends on the cause of the pathology. Babies with suspected biliary atresia require diagnostic surgery with intraoperative cholangiography. If biliary atresia is confirmed, portoenterostomy is performed (Kasai procedure) - this is the absolute method of choice for surgical treatment of biliary atresia. It is advisable to perform the operation in the first two months of life, since in the future the short-term prognosis worsens significantly. Even with adequate therapy, many children develop cirrhosis and require liver transplantation.
In the absence of indications for specific therapy, therapeutic nutrition with supplements of vitamins A, D, E, K is recommended. When artificial feeding, mixtures rich in MCTs (medium chain triglycerides), which are better absorbed in case of bile acid deficiency, are recommended. Read more about the diet for hepatic cholestasis on our website Dobrobut.com.
The prognosis of neonatal cholestasis ranges from a benign course to a progressive disease leading to cirrhosis. Biliary atresia, if not treated promptly, leads to liver failure and death before the age of one year.
Consequences of cholestasis
Cholestasis is a rather dangerous syndrome that must be identified and eliminated in time. If you follow all the doctor’s recommendations, it is possible to achieve stable remission, and even complete recovery. If this syndrome is ignored, the following adverse consequences may occur :
- indigestion;
- liver failure:
- development of liver fibrosis;
- hepatic encephalopathy;
- cirrhosis;
- bleeding;
- osteoporosis;
- osteomalacia.