Often, mothers at pediatrician appointments hear the question - how do we poop? A person who is far from being a toddler will raise his shoulders in bewilderment. Well, who cares how the child solves his toilet problems. But experienced mothers know that the color, consistency, nature of feces and, in general, the process of defecation are an important criterion for assessing the overall health and development of the baby.
And if feces of a suspicious color, smell or consistency are found in a diaper or potty, then the right mother will draw certain conclusions and visit the pediatrician with the toddler.
Normal color of stool at different ages in children
Normal baby's stool in the first days of life is blackish-green in color.
Normal adult feces are brown or yellow-brown in color. But digestion in children differs significantly from the functioning of the gastrointestinal tract of adults.
In the first days of life, infants have black or black-green stool. This is meconium coming out. After 3–4 days, the color of the baby’s feces changes.
If the baby is breastfed, then his stool will be yellow in color and have a soft, even liquid consistency. If the child receives an adapted formula, then the parents will find pale yellow excrement in the diaper.
Currently, infant formulas are additionally fortified with iron to prevent anemia, so the stool takes on a greenish tint. The normal number of bowel movements in a child under one year of age is from 1 to 3 bowel movements per day.
After 6 months, the baby begins to receive additional nutrition and his feces begin to approach the usual brown color.
Immediately after birth
When the baby is in the mother's tummy, he receives all the necessary substances and microelements through the umbilical cord. The baby's digestive system is not working, but his stomach is not empty. The baby sucks his fingers, opens his mouth and thus swallows a small amount of amniotic fluid. When the baby is born, this substance will be in his intestines and will gradually be released as the baby is applied to the breast and his digestive system begins its work.
So, the baby’s first stool is meconium: dark feces with the consistency of plasticine. This is how the baby recovers for the first day or two. Sometimes this gives him unpleasant sensations: the baby worries, cries, strains before he manages to relieve himself. However, this is not always the case - many children recover easily, only by slightly pushing.
If everything is fine with the baby, he was put to the breast on time and fed on demand, then his stool gradually changes. On the third to fifth day, the baby has the so-called “transitional stool”, partly consisting of meconium, which is still in the gastrointestinal tract, partly from digested colostrum and milk. As a rule, first streaks appear in the meconium mass, then the stool gradually turns yellow. By the end of the first week, the baby's stool usually takes on the characteristics of a normal baby: yellow, rather liquid.
When should you worry? If the baby does not lose weight in the first two days, you should consult a doctor. There are children with individual characteristics who will continue to do this less often than most children. However, the cause of stool retention must be determined by a doctor. If the baby has some kind of problem with intestinal patency, help will be needed immediately, but you should not diagnose your baby without a doctor.
When should you not worry?
If a mother eats spinach, the baby's stool color may change.
Yellow liquid stool may be normal in toddlers in their first year of life. When not to sound the alarm:
- the episode of loose stool is isolated;
- the baby is active, walks and is interested in toys;
- there are no signs of fever or intestinal colic;
- the tummy is not bloated or seething;
- feces are not foul-smelling or foamy.
In this case, parents should calm down and enjoy life with their little one. Yellow feces can be caused by excess juices in the diet and the period of dentition. At this time, teeth are being cut, and this puts a strain on the digestive system as well.
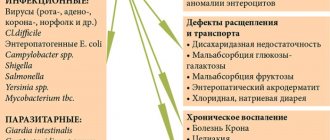
Types of diarrhea
Foamy diarrhea in an infant, which has a strong odor and is accompanied by an increase in temperature, as well as symptoms of intoxication, indicates the presence of an intestinal infection. Classification of acute intestinal infections by type of diarrhea:
- Invasive type. Acute intestinal infections of bacterial etiology. They are caused by Salmonella, Shigella, some types of Escherichia, Yersinia and other pathogens. Pathogens can invade the epithelium of the gastrointestinal tract and cause foamy stool. Watery diarrhea with yellow-green mucus mixed with blood in a child often indicates salmonellosis. Green stool and small amounts (“rectal spitting”) indicate the occurrence of shigellosis.
- Secretory type. Such diarrhea in an infant can be of bacterial etiology (Vibrio cholerae, enterotoxigenic Escherichia, Klebsiella, Campylobacter, etc.) or viral (rotaviruses, coronaviruses). These pathogens multiply only on the surface of the intestinal epithelium. This type of diarrhea causes very loose stool in a newborn, looking like “water.” Yellow diarrhea in infants and older is a clear sign of rotavirus infection.
- Mixed type. Caused by a mixed infection, clinical signs include symptoms of both invasive and secretory types.
To isolate the suspected pathogen, feces, vomit, and gastric lavage are used, where it is identified using bacteriological examination.
Its main disadvantage is the long time it takes (5-7 days); sometimes diarrhea in a newborn can be cured even before results are obtained. Serological tests are also used to detect the titer of antibodies to a specific pathogen. Treatment of acute intestinal infections is prescribed by a doctor, since loose stools in an infant can quickly lead to dehydration with serious consequences. Rehydration and detoxification therapy are prescribed, and antibacterial drugs are prescribed for bacterial infections.
Baby of the first year of life. Yellow feces as a sign of pathology
The color of a child's stool depends on complementary foods.
If a baby begins to have diarrhea of any color, this causes concern and even panic among parents.
At this age, the yellow tint of stool and its liquid consistency is not considered a pathology.
If the baby is breastfed, then the mother should first review her diet and eliminate medications, if any. A banal overload of food can also cause a negative reaction in a baby.
A similar disorder can occur if the baby sucks only part of the mother's milk. This happens when a woman, having listened to the advice of her grandmothers, expresses foremilk before feeding.
Previously, there was a myth that this milk burns out and therefore it should be expressed and only then given to the baby. In this case, the baby receives only fatty hind milk, but does not receive fore milk - less fatty, but rich in proteins. The result is yellow diarrhea.
The unexpected color of stool causes dysbiosis - a violation of the ratio of beneficial and opportunistic bacteria. In addition, this pathology may exhibit the following symptoms:
- regurgitation of milk;
- belching;
- pain and rumbling in the stomach;
- increased gas formation;
- the baby is worried, crying, pulling his legs towards his tummy;
- development slows down, the baby does not gain weight.
If dysbiosis is suspected, it is recommended to take a stool test and, based on its results, the doctor will prescribe antibacterial therapy to suppress pathogens and drugs to normalize the microflora. An infant is not immune from intestinal infections, especially when the active period of crawling and exploring the world begins. The alarm should be sounded in the following cases:
Stool color as a symptom
If the color of stool cannot be explained by a monotonous diet or use of medications, then it can be considered as a diagnostic criterion:
- Green diarrhea occurs if there is an infection of viral or bacterial origin in the digestive tract. Staphylococcal bacteria are found in stool, which gives it a greenish tint. In addition to diarrhea, the child is worried about abdominal pain, nausea, vomiting, weakness, and increased body temperature;
- The black color of stool is due to the presence of oxidized hemoglobin, which can enter the stool from stomach or duodenal ulcers. If Helicobacter multiplies in the stomach, the diet is not followed, the diet contains a lot of spicy, heavy or fatty foods, or there is a chronic gastrointestinal disease, then a peptic ulcer can develop in a 5-year-old child. This disease requires urgent treatment;
- if biliary excretion is impaired, the stool becomes grayish-white in color (acholic stool) as a result of the absence of decomposed bilirubin in it. White stool and dark urine indicate liver dysfunction;
- Yellow stool occurs if the contents of the intestine do not have time to mix with bile, since intestinal motility is increased and the passage of feces is accelerated. Infections, medications, toxic substances, and stressful conditions can lead to increased physical activity.
Based on only one symptom, it is impossible to determine the cause of the pathology; it is necessary to consider the clinic as a whole.
Intestinal infection
If, in addition to yellow diarrhea, the child experiences fever, vomiting, nausea, and weakness, then there is a high probability of developing an infection in the digestive tract. Intestinal infections most often develop in young children due to lack of hygiene skills. In children under three years of age, the disease is more severe and can cause dysbiosis, enzyme deficiency, and a decreased immune response.
Intestinal infection is caused by gram-negative enterobacteria (Shegella, Salmonella, Eschirichia, Yersinia, Campylobacter), opportunistic bacteria (Staphylococcus, Proteus, Clostridia, Klebsiella), viral agents (rotaviruses, adenoviruses, enteroviruses), protozoa (Giardia, amoeba, coccidia), mushrooms.
The frequency of bowel movements during illness can vary from 4 to 20 times a day, as the body tries to eliminate pathogenic microorganisms
With dysentery and salmonellosis, the stool is profuse, containing mucus and blood. With escherichiosis in children, watery diarrhea occurs (defecation is yellow water mixed with mucus), and blood may be present in the stool. Rotavirus infection causes watery, foamy stools up to 15 times a day.
The causative agent of the disease can only be identified through laboratory testing. Etiotropic therapy is carried out with antibiotics, intestinal antiseptics, and enterosorbents. It may be necessary to take specific bacteriophages, immunoglobulins or lactoglobulins, so treating an intestinal infection on your own is not recommended.
Poisoning
The occurrence of vomiting, nausea and diarrhea may indicate poisoning with low-quality products or toxic substances (plant or chemical origin). In this case, abdominal pain is most often cramping in nature and intensifies during bowel movements. The stool is watery with mucus and streaks of blood, its frequency can reach 10 times a day.
In severe cases, body temperature rises, intoxication syndrome increases, and dehydration begins. In a newborn, diarrhea most often occurs due to the consumption of poor-quality food. If the poisoning is severe, the stool becomes foamy (white foam).
For children under one year of age, diarrhea is a serious symptom because it can quickly lead to dehydration, which can be fatal, so seek medical attention as soon as possible. It is possible to identify the causative agent of foodborne toxic infection using bacteriological culture of feces, vomit, and gastric lavage.
Enzyme deficiency
If there is no enzyme that breaks down the substance, or if it cannot be activated in the small intestine, they speak of enzyme deficiency. In children, the disease is most often congenital. Undigested fats enter the lumen of the large intestine, stimulate cell secretion, which is why diarrhea occurs. The stool has a fetid odor, its surface is oily, shiny, the color can range from dull yellow to gray, and undigested food is noticeable in the stool. Children eat poorly and do not gain weight.
If it is impossible to break down milk sugar, infants and young children experience regurgitation, colic, flatulence, diarrhea or constipation, and disturbances in the functioning of the central nervous system.
The main symptom of lactase deficiency is fermentative diarrhea, which is manifested by frequent, loose, foamy stools with a sour odor. A child can defecate 10–12 times a day. When dairy products are excluded from the diet, the baby’s condition improves and he begins to gain weight. Lactase is synthesized in smaller quantities with age, so the disease can develop even by 4 years, despite the fact that milk was well absorbed in infancy or early age.
At 9–18 months, a genetically determined disease, celiac disease, may appear. In pathology, there is no enzyme that breaks down gluten, which is found in bread, pasta, oatmeal, barley flour, semolina, sausages, chocolate, cocoa powder and other products. The child has frequent, loose, foamy stools with a high fat content and undigested food debris. Defecation occurs 5 times a day or more. Treatment is based on adherence to a gluten-free diet.
Yellow diarrhea in older children
In the first months, infants have loose stools - this is the norm!
Unpleasant symptoms in children over one year old and adolescents can be caused by a number of reasons:
- Poor quality and stale food, consumption of prohibited foods.
- This is a kind of food intoxication. In mild cases, it causes only disruption of bowel movements; in severe cases, it causes serious food poisoning with pain, diarrhea, and in severe cases, disruption of the functioning of other organs.
- Infectious diseases of the gastrointestinal tract.
- Violation of the production of necessary digestive enzymes.
- Enzymepathies can be acquired or hereditary; intolerance to certain foods and drinks is a separate category.
- The specific symptomatology of this disease in children is a reaction to certain foods. Often in childhood, doctors are faced with hereditary enzymopathies - galactosemia, phenylketonuria, celiac disease. In addition to yellow diarrhea, the child will have other signs corresponding to a particular pathology.
- Chronic inflammatory processes in the gastrointestinal tract - gastritis, colitis, enterocolitis. Diarrhea is one of the symptoms of the pathology. Additional signs will help make a correct diagnosis - pain in the epigastric region in different locations, the nature of the pain, intestinal bloating, the appearance of stool and the frequency of bowel movements.
- Stressful situations, nervous tension.
- Imbalance of beneficial and opportunistic intestinal microflora.
- Acute leukemia is a malignant blood disease. With this pathology, bleeding occurs from various parts of the gastrointestinal tract, ulcerative-necrotic processes in the intestines.
If yellow diarrhea appears, you should carefully monitor the child's condition. If, in addition to defecation disorders, additional symptoms appear, you should definitely contact a medical facility.
Thematic video material will tell you what diarrhea in a child means:
https://www.youtube.com/watch?v=97NpP6QW-w4
Eliminating diarrhea in a child
If a child has loose stools once, then there is no need to start drug therapy. It is necessary to remember what foods were in the baby’s diet over the last 24 hours and, if the symptom repeats, analyze whether there is a pattern. Thus, it will be possible to identify foods to which the child has an individual intolerance, and in order to reduce the load on the digestive system, they simply need to be excluded from the diet.
If pathological inclusions are visible in the stool, such as fat, food particles, a large amount of mucus, or blood, then you need to take blood and stool tests, and undergo an ultrasound examination of the abdominal organs. Only after an examination will it be possible to make a diagnosis and prescribe adequate therapy that eliminates not the symptom, but the cause of the disease.
If diarrhea is frequent and profuse (regardless of the color of the stool), then you should seek medical help. To prevent the development of dehydration, children under one year of age are recommended to be hospitalized for infusion therapy.
Infants with diarrhea quickly develop life-threatening dehydration
Diet therapy
If yellowish diarrhea occurs, regardless of the cause of the symptom, a therapeutic diet No. 4 is prescribed, which helps reduce the load on the digestive tract and reduces the severity of putrefaction and fermentation processes in the intestines. It is recommended to feed the child in reduced portions, but more often, so that food is absorbed in the intestines and does not pass through in transit.
Any foods that stimulate the secretion of gastric juice and intestinal motility should be removed from the menu. Cold drinks and dishes have a laxative effect, so they should not be given during diarrhea. To reduce the severity of the fermentation and putrefactive process, you need to remove legumes, cabbage, fatty meat, milk, fresh vegetables and fruits from the diet.
When yellow diarrhea appears, a child's menu may include mucous soups, cereals, dietary meat and fish, crackers, fermented milk products, jelly, and jelly. All dishes must be steamed or boiled. Diet is an important component of therapy, so compliance with it is mandatory for several more days after the yellow diarrhea disappears.
A gluten-free or dairy-free diet in the presence of enzyme deficiency should be followed at all times.
Yellow diarrhea after antibiotics
Antibiotic drugs destroy pathogenic microflora in the intestines. But at the same time, beneficial symbionts that ensure the normal function of the gastrointestinal tract also suffer. Although gentle forms of antibiotics are currently being produced, some of which do not upset the balance of flora in the gastrointestinal tract and can be used for a long time.
In children, the balance between beneficial and pathogenic microorganisms is easier to disturb than in adults. And no one has canceled the side effects of medications. If diarrhea begins after taking antibiotics, you should monitor the child’s condition and consult a pediatrician.