Helicobacter pylori is a certain type of bacteria that is harmful to the human body. These pathogenic microorganisms live in the stomach and duodenum. As a result of their vital activity, the functioning of these organs is disrupted, since the toxins produced by Helicobacter destroy their mucous membrane.
In some cases, the human immune system is able to cope with bacteria, but if this does not happen, then the walls of the organs are damaged, which is why various intestinal diseases develop: gastritis, cancer, ulcers and others. How to determine the presence of Helicobacter in the body, and what is the norm?
Indications for use
Experts recommend taking this type of analysis at least once a year. This preventive measure will help prevent the development of many diseases associated with the digestive tract. It is imperative to consult a doctor and donate blood for Helicobacter pylori if the following symptoms occur:
- the appearance of pain and discomfort in the stomach during or after a meal. This sign often indicates a lack of digestive enzymes, stagnation of food;
- pain that appears if a person has not eaten for a long time. When eating food, such pain gradually disappears;
- damage to the esophagus is indicated by the feeling that during swallowing the patient clearly feels the movement of food, painful swallowing often occurs;
- Repeated heartburn is another reason to go to the clinic. The reflux of gastric juice negatively affects the health of the esophagus, causes severe discomfort, and often indicates damage to the gastrointestinal tract by the Helicobacter bacterium;
- heaviness in the stomach after eating even a small amount of food. A person has the feeling that food is standing in one place and is not digested;
- frequent nausea, which is not provoked by poisoning, pregnancy and other factors that usually cause it;
- the appearance of mucus or blood streaks in the stool;
- periodic pain in the ventricle, during which the patient cannot eat or drink. The condition is often accompanied by vomiting.
Even minor pain and discomfort in the stomach and intestines should not be ignored, as they often indicate the initial stage of the development of the disease.
In newborn children, one should take into account such signs as severe flatulence, frequent regurgitation, unreasonable crying in which the child draws in his legs, stool disorder - diarrhea or, conversely, constipation.
Who should have their blood tested for Helicobacter?
The introduction of Helicobacter into the stomach wall may be accompanied by atypical, but noteworthy, symptoms:
- pain - the intensity ranges from mild to strong, occurs during or after eating, “hungry” pain is possible, often a person describes his sensations when a bolus of food passes through the esophagus;
- heartburn - associated with the reflux of gastric juice into the lower parts of the esophagus, frequent repetitions are caused by increased acidity and damage to regulatory processes;
- a feeling of heaviness in the epigastric area - manifests itself after even a light meal;
- nausea - without signs of pregnancy toxicosis or any pathology;
- sometimes vomiting and acute pain in the stomach, similar to food poisoning;
- the presence of mucus and blood in the stool;
- constant belching;
- bloating (flatulence);
- violation of bowel movements (constipation or tendency to diarrhea);
- unknown weight loss.
Moderate pain due to stressful situations is a sign of Helicobacter infection
If the listed symptoms are constantly associated with risk factors such as:
- constant discomfort or overeating, drinking alcohol, hunger;
- hereditary disadvantage in the family.
A person should undergo a full examination to exclude:
- peptic ulcer;
- cancer of the stomach or esophagus;
- esophagitis (inflammation of the esophagus);
- identifying differences with dyspepsia of other etiologies;
- gastritis and duodenitis;
- infection of close relatives with Helicobacter;
- relationship to the risk group.
Repeated blood tests are recommended to assess the patient’s condition during treatment.
Features of the bacterium and its danger
Before we figure out what the analysis is, let’s find out what the characteristics of the bacterium are and what its danger to health is. Helicobacter pylori is one of the pathogenic microorganisms that can interfere with the production of gastric juice in humans. It moves quite quickly thanks to its flagella. In addition, the ammonia produced by the bacterium has a detrimental effect on stomach acid.
Helicobacter pylori is very dangerous for the body, causing gastritis, ulcers and other stomach diseases
Penetrating into the mucous membrane of the digestive organs, the uninvited guest provokes the appearance of ulcers and foci of inflammation. The bacteria multiplies quickly, poisoning the body more and more every day. It is transmitted through close household contact, sharing utensils and other hygiene items. Therefore, if this microorganism is detected in one of the household members, other family members are recommended to donate blood for Helicobacter pylori.
Important! The bacterium is resistant to gastric juice, but under the influence of antibacterial drugs it dies quite quickly.
Features of infection in children
Morbidity statistics show that 35% of preschool children and 75% of schoolchildren are infected with helicobacteriosis in Russia. Small children get the infection from mothers licking nipples, spoons when feeding, from saliva during kissing, and sharing utensils.
Detection of antibodies in the blood allows a timely course of therapy to cure the child. But at the same time, you should look for bacteria carriers among adult family members. Since it has been established that 3 years after the course of treatment, 35% of children experience re-infection. After a period of 7 years, the number of infected reaches 90%.
The most common clinical picture of the lesion develops in a child:
- from nausea;
- refusal to eat;
- dyspepsia (excessive regurgitation, bloating);
- unclear pain.
Preparation
An analysis for Helicobacter pylori involves the detection of specific antibodies in the blood serum, which are produced by the immune system when the pathogenic organism enters a person. These antibodies can be detected in the laboratory using simple chemical reactions. When detecting uninvited guests, the doctor must take into account that a sufficient amount of time must pass for the development of immune agents. That is, the formation of antibodies requires at least 7–10 days. It is this interval that is necessary for the appearance of an immune response to the pathogen.
The most accurate data can be obtained with the help of special preparation for analysis. It includes the following activities:
- a few days before the study, it is important to give up alcoholic beverages;
- 24 hours before blood sampling, you should avoid heavy physical activity and intense sports;
- Before the procedure you should not eat food, you are only allowed to drink water:
- collection of biological material is carried out in the morning;
- The study is carried out before the person starts taking any medications. If the patient is already undergoing therapy with certain medications, this must be reported when donating blood.
Accurate results can be obtained with proper preparation.
If the preparation rules are violated, a false positive response is possible. An incorrect result also often occurs in cases where the patient has undergone treatment, but antibodies are still present in the blood.
Important! A false negative analysis is observed if too little time has passed after the body has been damaged and the immune system has not had time to develop antibodies.
What's next?
An accurate diagnosis is the key to success. But the question arises: what to do next? The treatment regimen is prescribed by the European Helicobacter pylori Study Group in the so-called Maastricht Consensus. Since 1997, four such consensuses have been published. The fifth one took place in November 2016. Each subsequent “Maastricht” supplements the previous ones based on clinical studies obtained from European countries. Russia also supplies its analytics to the experts of the committee of this European group.
Treatment of Helicobacter in any case is antibacterial.
There are first-line and second-line therapies. In addition, there is triple therapy, which is prescribed if there is no mucosal defect, and quadruple therapy - if there is a mucosal defect (erosion or ulcer). Then the doctor prescribes bismuth preparations; they have a local wound-healing effect.
It may happen that first-line treatment is ineffective. Typically, if the doctor's recommendations are followed correctly, the effectiveness of first-line therapy is 70-98%. However, there are individual resistance, contraindications or side effects. For example, there is a fairly high resistance to clarithromycin in the first line; there are special regimens for such patients. The drug may also be poorly tolerated, resulting in diarrhea, vomiting, and a metallic taste in the mouth. In this case, clarithromycin can be replaced with levofloxacin or nifuratel. If the first two lines of treatment
turn out to be ineffective, then a culture is taken to test the sensitivity of the bacteria to antibiotics, and therapy is selected in accordance with the culture results. In this case, they say that we are dealing with a refractory form of Helicobacter pylori.
ELISA analysis
An enzyme-linked immunosorbent assay (ELISA) is necessary to determine whether a person has antibodies to the bacterium Helicobacter pylori. That is, not the pathogen itself, but the immune cells that the body begins to synthesize when an infectious agent enters. These antibodies are produced by plasma cells formed from B lymphocytes. During laboratory testing, they can be detected on the surface of B lymphocytes and in blood serum.
Another name for protective cells is immunoglobulins. There are five types of such cells in humans and mammals. They are designed to combat various viruses and bacteria. When it comes to Helicobacter, it is customary to talk about such types of protective cells as LgG, LgM, LgA. It is these three species that take an active part in the fight against the bacterium.
References
- Ivashkin, V.T., Maev, I.V., Abdulganieva, D.I. etc. Practical recommendations of the Scientific Community for Promoting the Clinical Study of the Human Microbiome (NSOM) and the Russian Gastroenterological Association (RGA) on the use of probiotics for the treatment and prevention of gastroenterological diseases in adults. Russian Journal of Gastroenterology, Hepatology, Coloproctology, 2022. - T. 30.
- Guevara, B., Cogdill, A. Helicobacter pylori: A Review of Current Diagnostic and Management Strategies. Dig Dis Sci., 2022. - Vol. 65(7). – P. 1917-1931.
- Choi, I., Kim, C., Lee, J. Family History of Gastric Cancer and Helicobacter pylori Treatment. N Eng l J Med., 2022. - Vol. 382(5). — P. 427-436.
- Nagy, P., Johansson, S., Molloy-Bland, M. Systematic review of time trends in the prevalence of Helicobacter pylori infection in China and the USA. GutPathog., 2016. - Vol. 8.
- Alem, M., Alem, N., Cohen, H. et al. Diagnostic value of detection of IgM antibodies to Helicobacter pylori. ExpMolPathol., 2002. - Vol. 72(1). — P. 77-83.
What does the detection of immunoglobulins indicate?
When donating blood for infection, doctors do not attach any special importance to the norms. Here, most likely, we are talking about the presence or absence of antibodies. The results table is used in some clinics, but not everywhere. The detection of immunoglobulins in biological material indicates infection with Helicobacter pylori and that pathogenic microorganisms are already actively multiplying. If antibodies are not detected, it is customary to talk about the absence of bacteria.
Blood testing is carried out in a laboratory using special equipment
Values of detected immunoglobulins:
- LgA – signals the early course of the disease. That is, the presence of this protein indicates that the bacteria entered the body recently and has just begun to multiply. Sometimes this type of antibody is detected in diseases accompanied by inflammation of the gastric mucosa;
- LgM - these proteins are recorded in the blood quite rarely. This is explained by the fact that at an early stage, few patients consult a doctor. More often, people get tested when severe pain in the stomach and other dyspeptic disorders appear;
- LgG - confirm the fact of infection with a bacterium. Most often, these proteins are detected 7–20 days after pathogenic microorganisms enter the digestive system. In addition, LgG immunoglobulins remain in the body throughout the disease and for some time after its cure.
It is worth noting that, even knowing the basic values of immunoglobulins, an ordinary person will not be able to independently establish a diagnosis. This should be done by an experienced specialist. Only a doctor can determine the degree of development of the disease and select the appropriate treatment.
Decoding the analysis results
Despite the fact that the decoding of the indicators should be entrusted to the doctor who referred for the examination, all patients want to find out their results on their own.
How much is the norm for Helicobacter pylori? The norm of bacteria content when testing venous blood: 0-0.9 units/ml .
Interpretation of other meanings:
- 0.9-1.1 units/ml – the likelihood of Helicobacter pylori infection is doubtful;
- More than 1.1 units/ml – bacteria are definitely present in the body. High risk of developing stomach ulcers and stomach cancer.
The norm for the urease test is the absence of crimson color in the color of the material. The norm for bacterioscopic examination is the absence of pathogens.
Interpretation of results
Decoding the ELISA analysis allows you to clarify some data about the pathology and select treatment methods. The interpretation should be carried out exclusively by a specialist who, when reviewing the results obtained, can accurately determine the characteristics of all immunoglobulins found in the blood.
Positive analysis
If immunoglobulin LgA is detected in the patient’s biological material, then the test is positive and Helicobacter pylori is present in the body. At an early stage of the disease, LgM proteins are also detected. They can be detected no earlier than 1–2 weeks after infection.
When considering the analysis, the doctor must take into account two options. In the first case, we are talking about the fact that the bacterium remains in the body for some time after treatment. If there is a suspicion of stomach cancer or other pathologies, additional diagnostic methods are prescribed, such as ultrasound and others.
Positive results indicate the presence of pathogenic bodies in the human body
If a person goes to the hospital for the first time and these immunoglobulins are found in his biological material, it is customary to talk about the presence of Helicobacter pylori or severe inflammation of the stomach.
Negative result
A negative test is observed in those patients who have undergone successful treatment with antibacterial drugs or the bacterium is not detected in their body. That is, the norm for Helicobacter pylori in the blood is when antibodies to this bacterium are not detected. Sometimes a negative response is observed in people whose infection occurred only recently. In this case, the LgM protein may also be detected, but the LgA immunoglobulin is still absent.
Important! The presence of LgM and LgG in 99% of cases indicates infection with Helicobacter pylori and active reproduction of the bacterium.
Types of analyzes and diagnostics
There are several methods for studying the state of the body. Each of them has its own characteristics.
ELISA for bacteria
An enzyme immunoassay is prescribed to assess the level of concentration of antibodies to Helicobacter pylori in the patient's blood. If there are antibodies to the bacteria in the blood, it means that the immune system developed them at least 1-2 weeks ago. If the body's reaction has not yet been formed, a false negative result is possible.
Reasons for false positive results:
- error by the laboratory technician conducting the study;
- not enough time has passed after eradication, since antibodies are in the blood some time after complete cure.
A positive ELISA result indicates the need for a full examination, studying the results of an extended blood test, which provides more information about the condition of the body.
Immunoglobulins in the blood LgG, LgM, LgA
In the human body, when infections or pathogenic microorganisms penetrate it, immunoglobulins are produced - blood cell proteins that resist foreign viruses. When infected with Heliobacteriosis, the human body produces immunoglobulins LgG, LgM, LgA, which actively resist Helicobacter pylori. If they are detected in a person’s blood, it should be concluded that he is sick with heliobacteriosis.
The peculiarity of immunoglobulins is that in pursuit of pathogenic cells they overtake them anywhere in the human body. These proteins are produced after colonization by bacteria in the gastrointestinal tract.
Analysis transcript:
- A reduced or negative level of LgG immunoglobulin indicates one of the following options: the bacterium is absent in the body and the likelihood of developing a peptic ulcer is low, or only 3-4 weeks have passed since infection. If you have pain in the gastrointestinal tract, you need to repeat the examination in a week.
- An elevated or positive level of immunoglobulin LgG indicates one of two options: the bacterium is present in the body, increasing the risk of developing cancer and stomach ulcers, or the person has recently been cured of heliobacteriosis.
- A reduced level of immunoglobulin LgM, usually detected immediately after infection, or its absence, clearly indicates the absence of bacteria, since this protein is detected in the early period after infection.
- An increase in LgM levels indicates that the gastrointestinal tract is at an early stage of infection, and it is almost undamaged by the infection.
PCR analysis
The results of a polymerase chain reaction study can detect Helicobacter pylori DNA samples in the blood, which puts the PCR test in first place among all diagnostic methods. A positive test result proves the presence of bacteria in the body, a negative test shows its absence. The only thing that is not available when performing a PCR blood test is determining the time of introduction of the bacteria into the body.
If antibacterial therapy or antiseptic treatment was carried out before taking blood for analysis, the results of the study will not be objective. It is better to entrust the interpretation of blood tests to a specialist, although serious laboratories include a table of the norm and deviations from it in the results.
Cytological examination
In this test, swabs are taken from the antrum of the stomach during endoscopy. The area where the smear is taken is the area of edema and hyperemia, but not erosion or ulceration. After taking fingerprints, the laboratory technician dries and stains the smears.
When examined under a microscope, Helicobacter pylori can be found in the form of a spiral or in the form of the wings of a flying seagull.
Cytology reference values:
- (+) — low level of contamination (up to 20 microbial bodies);
- (++) – average level (up to 40 microbial bodies);
- (+++) – high level (over 40 microbial bodies at 360x magnification).
Additionally, in the presence of inflammation, a cellular infiltrate is detected: (eosinophilia, neutrophilia, lymphocytes, plasma cells). Additionally, dysplasia, proliferation, metaplasia, and malignant neoplasms can be detected.
Urease test
The study is performed after taking a biopsy of the mucous membrane during endoscopy. It is placed in a carrier gel containing urea, a pH indicator, and a bacteriostatic agent. Conclusions are made based on the change in color of the biopsy material ranging from yellow to crimson.
Reference values:
- A crimson color appeared in the first hour – severe infection (+++);
- In the first 2 hours – moderate level of infection (++);
- By the end of the day – an insignificant level of infection (+);
- At a later date – the norm or a negative result.
With a low level of infection, a false negative result may be recorded. To increase reliability, it is combined with a histological method.
13C urease test, breath
This testing involves taking background breath samples on an empty stomach. After a light breakfast in the form of juice or milk, the subject drinks an aqueous solution of 13C-labeled urea, the so-called test solution. Then, 4 final samples are taken every 15 minutes.
Analysis of the test based on the presence of a stabilized isotope using a mass spectrometer:
- Mild infection - less than 3.5%;
- Average degree – 3.5-6.4%;
- Severe degree – 6.5-9.4%;
- Very severe degree - over 9.5%.
The norm for Helicobacter pylori in the urease test is 1%.
Hemotest
The analysis is based on determining the titer of antibodies - class G immunoglobulins. Normally, when Helicobacter enters the body, they bind microorganisms, stopping their pathogenic effect. The study is carried out by enzyme immunoassay after taking blood from a vein into a sterile tube. Before the study, you should not eat for 8 hours, drink coffee or alcohol, or smoke. To study the dynamics, the analysis is carried out throughout the entire treatment period.
Table for deciphering the ELISA analysis in IFE units of measurement
For more accurate interpretation of data in medical practice, a special table is used.
| Immunoglobulin type | IFE is higher than normal | Norm | IFE below normal |
| LgG | the person has undergone treatment, but antibodies are still detected, inflammation of the gastric mucosa is suspected of cancer, infection has occurred. | 30 | the infection occurred less than two weeks ago, Helicobacter is not present in the body. |
| LgA | infection has occurred, but the disease is latent and the disease has become chronic. | 30 | initial stage of infection, recovery or period of treatment with antibacterial drugs, absence of Helicobacter pylori (only with negative LgG immunoglobulins). |
| LgM | early course of the disease. | are discovered | infection occurred no more than 10 days ago, active antibiotic therapy, complete recovery or absence of pathogenic microorganisms. |
If antibodies are not detected, but the patient has symptoms characteristic of the disease, after some time he is prescribed a repeat test.
How is enzyme immunoassay performed?
Helicobacter ELISA consists of detecting a certain concentration of antibodies in the blood serum. The indicator is estimated by their dilution or titer. The presence of a positive reaction indicates that a reaction is occurring in the body with a foreign antigen in the form of Helicobacter. The severity and magnitude of the indicator determine the strength of the immune response.
Positive aspects of the method:
- the possibility of conducting research at the laboratory level in the clinic;
- detection of bacteria in the early stages of infection;
- no need for fibrogastroscopy to confirm the etiology of the disease.
Flaws:
- there remains the possibility of a false negative result in infected patients if the immunity is not strong enough;
- a false-positive effect can be obtained in patients who have already been treated, but retain antibodies to Helicobacter pylori;
- the bacterium itself cannot be isolated;
- low antibody titers are detected during treatment with cytostatics;
- the results of a blood test for antibodies to Helicobacter pylori are difficult to evaluate if the patient is treated with antibiotics, even for reasons that are not related to gastric pathology.
This means that the ELISA method is not perfect enough and does not answer many questions during diagnosis and treatment and requires additional examination.
Advantages and disadvantages of the method
Like other diagnostic techniques, ELISA analysis has its pros and cons.
Advantages:
- high efficiency (about 95%);
- the ability to detect antibodies to the pathogen in the early stages of disease development;
- assessment of the dynamics of pathology and the effectiveness of drug therapy;
- safety and possibility of multiple use;
- availability.
Enzyme immunoassay has its advantages and disadvantages
Despite the large number of advantages, there are also disadvantages. Among them are:
- inability to detect infection from the first days of infection;
- the analysis shows the presence of antibodies, but not the bacterium itself;
- when Helicobacter pylori enters the body for the first time, the response is false negative;
- a false positive result occurs after the disease has been cured for some time.
An important aspect in conducting ELISA is the level of qualifications of laboratory staff and the equipment used. It is believed that the most accurate results can be obtained in private clinics, which have modern and expensive microscopes and other research equipment in their arsenal. Such an analysis will cost more than in a public hospital, but its results will be more accurate.
A comprehensive test designed to detect H. pylori in patients with suspected gastritis, gastric or duodenal ulcers, including basic serological tests and the RT-PCR method.
Synonyms Russian
Comprehensive diagnosis of helicobacteriosis.
English synonyms
H. pylori diagnostic panel, H. pylori Abs, IgA, IgG, H. pylori, PCR.
What biomaterial can be used for research?
Venous blood, feces.
How to properly prepare for research?
- The study is recommended to be carried out before starting antibiotics and other antibacterial chemotherapy drugs.
- Avoid taking laxatives, administering rectal suppositories, oils, limit (in consultation with your doctor) taking medications that affect intestinal motility (belladonna, pilocarpine, etc.) and drugs that affect the color of stool (iron, bismuth, barium sulfate), within 72 hours before stool collection.
- Do not smoke for 30 minutes before the test.
General information about the study
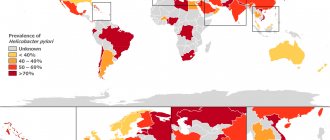
H. pylori is a gram-negative, facultative anaerobic microorganism that can infect the gastric and duodenal mucosa. In most cases, infection with H. pylori (helicobacteriosis, or helicobacteriosis) is permanent, chronic. Helicobacteriosis is very common: the bacterium H. pylori can be detected in 50% of people around the world. At the same time, H. pylori-associated diseases (gastritis, gastric or duodenal ulcers, gastric adenocarcinoma, MALT lymphoma) occur in only 15-20% of infected patients. A feature of these diseases is their favorable prognosis, subject to early diagnosis and complete eradication of H. pylori. Laboratory research methods play a leading role in the diagnosis of helicobacteriosis.
There are several methods for detecting H. pylori. Direct methods allow direct identification of the microorganism itself. Most direct methods require a sample of mucosal tissue (biopsy) and/or stomach and duodenal contents (aspirate), which are usually obtained during an endoscopic examination. Thus, direct research methods are usually invasive. In contrast, indirect methods do not detect the microorganism itself, but indirect signs of infection, for example, specific antibodies in the blood serum (serological tests) or the content of a labeled carbon atom in the exhaled air (breath urease test). Since indirect tests do not require endoscopic examination, they are called non-invasive. Both direct and indirect tests for H. pylori have their advantages and disadvantages. To accurately diagnose helicobacteriosis, several tests are required. In this regard, a comprehensive analysis that includes all the necessary tests for H. pylori is especially convenient for the doctor and the patient.
One of the most sensitive methods for detecting H. pylori is real-time polymerase chain reaction (RT-PCR). RT-PCR is a molecular diagnostic method that allows one to detect fragments of genetic material (DNA) of an infectious agent in biological material (for example, in a tissue sample). Since the analysis is based on the detection of genetic material, RT-PCR allows one to detect the presence of any forms of H. pylori (not only active spiral forms, but also inactive cocci, non-cultivable ones), as a result of which the study is characterized by very high sensitivity, exceeding the sensitivity of the bacteriological culture method. Theoretically, the presence of 1 DNA molecule is sufficient to carry out RT-PCR. In practice, the concentration of the pathogen in the sample should be about 10-100 CFU/ml. This high sensitivity of the test means that a negative test result allows H. pylori to be excluded as the cause of the disease. This is of fundamental importance in the differential diagnosis of NSAID-associated, stress and ischemic gastritis and ulcers.
It should be noted that despite the very high sensitivity of the test (85-98%), false negative results are still possible. For example, a false negative result can be obtained if the bacterial load is very low (for example, while taking certain antibiotics). Diagnostic errors can be avoided by combining this direct test with serological tests.
H. pylori infection is accompanied by a significant increase in IgG and IgA class immunoglobulins in the blood serum. These immunoglobulins (antibodies) are detected in the blood using indirect tests. IgG is found in 95-100% of cases of helicobacteriosis, and IgA in 68-80%. The study allows you to determine the antibody titer, that is, it is quantitative. Typically, high antibody titers are more characteristic of an active, ongoing infection. It should be noted, however, that there is no clear correlation between the antibody titer and the severity of the infection.
Serological tests, like the RT-PCR method, have some limitations. Thus, the result of the analysis depends on the characteristics of the patient’s immune response. The immune response of patients taking cytostatic drugs and the elderly is characterized by a reduced production of specific antibodies (any, including to H. pylori). For this reason, in order to avoid diagnostic errors, it is advisable to supplement serological tests with direct tests. This feature was taken into account when compiling a comprehensive analysis for H. pylori.
Thus, a comprehensive analysis for H. pylori is a combination of necessary and sufficient tests to identify this microorganism. The comprehensive analysis is not intended to monitor treatment. The result of both RT-PCR and the study of IgG and IgA immunoglobulins will remain positive even in the case of complete eradication of H. pylori. The false positive result of RT-PCR in this case is due to the ability of this method to detect the DNA of any, even destroyed microorganisms, while the false positive result of serological tests is due to the peculiarities of the dynamics of the immune response.
What is the research used for?
- To detect H. pylori in patients with suspected gastritis, gastric or duodenal ulcers.
When is the study scheduled?
- When examining a patient with signs of dyspepsia: discomfort or pain in the epigastric region, nausea, vomiting, loss of appetite.
What do the results mean?
Reference values
For each indicator included in the complex:
- [07-027] Helicobacter pylori, IgA (quantitative)
- [07-028] Helicobacter pylori, IgG (quantitative)
- [09-053] Helicobacter pylori, DNA [real-time PCR]
| Positive result | Negative result | |
| Helicobacter pylori, DNA [real-time PCR] (gastric aspirate, biopsy) |
|
|
| Helicobacter pylori, IgA (quantitative) | ||
| Helicobacter pylori, IgG (quantitative) |
What can influence the result?
- Treatment with tetracycline (doxycycline), penicillin (ampicillin, amoxicillin), macrolides (azithromycin, erythromycin) and metronidazole may lead to a false negative result;
- The immune response of older people, as well as patients receiving immunosuppressive therapy, is characterized by reduced production of specific antibodies, including to H. pylori, which leads to a greater number of false negative test reactions in this group of patients.
What can affect the result
Certain circumstances may affect the accuracy of the analysis. For example, in older patients, the body's immune response is slower, so it takes longer to produce antibodies. The same applies to people with very weakened immune systems, especially children who are often ill, as well as patients with various systemic pathologies.
Another group of patients who often experience a false-negative response are patients undergoing therapy with immunosuppressants. All these features must be taken into account by the doctor when interpreting the results and making a diagnosis.
A little about the features of Helicobacter
The literal Latin-Greek name Helicobacter pylori (“spiral pyloric”) is associated with the characteristic shape of the bacterium and its maximum residence in the zone of transition from the stomach to the duodenum (pylorus).
With the help of flagella, mobility and the ability to move in the gel-like mucus environment on the inner surface of the stomach are ensured. This is the only microorganism that can live in an acidic environment.
From its discovery in 1875 to the awarding of the Nobel Prize in 2005, 130 years passed. Many scientists have invested their knowledge and experience in studying the unusual infection. She did not grow on nutrient media. In order to confirm his research, Barry Marshall, a professor of the Department of Clinical Microbiology from Western University of Australia, conducted an experiment on himself: he drank the contents of a cup containing bacteria. Then, 10 days later, endoscopy showed a connection between the emerging signs of stomach inflammation and the presence of Helicobacter.
Marshall and his colleague Warren did not stop there. They were able to prove the cure of gastritis with a course of Metronidazole and a bismuth preparation, and showed the role of antibiotics in the treatment of gastritis, gastric and duodenal ulcers.
Helicobacter has many aggressive properties caused by its internal composition
Modern research has clarified the conditions for the existence of the microorganism. Helicobacter pylori uses the energy of hydrogen molecules released by intestinal bacteria. Synthesizes enzymes:
- oxidase;
- urease;
- catalase.
In hazardous conditions, it forms a film that protects against the body’s immune reactions. Over time, it changes its shape to spherical (coccal) and in this state is also contagious.
The important point is that it is in the stomach of a person without signs of disease. But if the protective forces fall, it behaves very aggressively, causing inflammation to ulcers and cancerous degeneration. That is why timely detection of traces of Helicobacter pylori in a blood test is so important for human health.
How to donate blood
To donate blood, a person must receive a referral from the attending physician and appear at the clinic at the appointed time. Biological material is collected in the morning on an empty stomach. Blood is taken from a vein on an outpatient basis. Immediately after this, the patient can go home.
Blood for Helicobacter is donated from a vein
Preparation for testing and duration of the study
Your doctor will tell you in detail how to take the test. Preparation includes:
- exclusion from the diet the day before blood donation of fatty foods;
- a categorical ban on alcohol;
- medication should be stopped 2 weeks in advance;
- minimizing physical activity;
- On the morning of the test, you are not allowed to have breakfast, you can only drink water (at least eight hours must have passed since your last meal).
Plasma is obtained from venous blood taken by sedimentation of red blood cells and other elements. Using a micropipette, it is introduced into the wells of a special plate with an antigen standard applied to them. Between substances, in the presence of antibodies in the serum, a reaction occurs and complex compounds are formed, which are visualized by adding a coloring compound.
The amount of antibodies is judged by the degree of coloring
For a more accurate assessment of the result, photometry is carried out using a spectrophotometer. It compares the material under study with control samples. Mathematical processing allows you to obtain quantitative indicators. The laboratory test for immunoglobulin G takes 24 hours to prepare, and the patient will receive the result the next day. A week is needed to study other globulins.
Other research methods
In addition to enzyme immunoassay, other diagnostic methods are often used in medical practice. The most popular and informative are:
- breath test for Helicobacter pylori - prescribed for the primary diagnosis of a bacterial infection or to assess the effectiveness of antibacterial therapy. The test is carried out in an outpatient clinic using a special plastic tube into which the patient must breathe for several minutes. In this case, the concentration of the isotope in the air should not exceed one percent. If these indicators are higher, it is generally accepted that infection has occurred;
- PCR or polymerase chain reaction is a widely used diagnostic method for identifying Helicobacter pylori. For the study, a person's blood, feces or saliva is taken. Determination of the presence of bacteria is carried out using a polymer chain reaction. Diagnostic accuracy is about 95%;
- histology or biopsy – used when a patient is suspected of having stomach cancer. Tissue analysis is carried out in a laboratory setting. Within normal limits, antibodies to Helicobacter and malignant processes are absent. If the result is positive, appropriate therapy is selected.
Analysis of the patient's blood and other biological materials is not the only research method. To obtain a more accurate clinical picture, doctors often prescribe gastroscopy, esophagogastroduodenoscopy (EGDS), fluoroscopy of the stomach, ultrasound examination, assessment of gastric juice in the laboratory and other methods. All this helps to establish an accurate diagnosis and choose the right treatment tactics.
Determination of Helicobacter pylori antigen in feces
The study is performed using the polymerase chain reaction (PCR) method. Its accuracy is 95%; determining the presence of bacteria in this way is recommended in children, elderly and seriously ill patients.
In order for the result of the analysis to be objective, you need to prepare for the study:
- Do not take antibiotics for 4 weeks before the test;
- 3 days before the test, do not eat foods that stain feces: red grape wine, beets, grapes, black currants;
- Before the study, 2-3 days before the study, exclude foods with coarse fiber from the menu: bran, radishes, cabbage, carrots, beets;
- Do not use medications that increase gastrointestinal motility.
For research, it is enough to fill a standard container for collecting samples one third full. You should not take feces from the toilet bowl, as it may contain traces of detergent. It is advisable to store the container with biomaterial for no longer than 10-12 hours at a temperature of +2 to -8°C.
The analysis result can be obtained the next day. Since stool analysis is a qualitative study, its result is formulated as “positive” or “negative”.