Megacolon is a chronic dilatation and enlargement of the colon or any part of it. The disease is characterized by the presence of constipation from the first months or years of life. In adults, the acquired form of megacolon is caused by a mechanical obstruction (scar narrowing or tumor).
The clinical picture of megacolon includes persistent constipation, flatulence, abdominal enlargement, fecal intoxication, and attacks of transient intestinal obstruction. The disease is diagnosed using X-ray methods (radiography, irrigoscopy), endoscopic studies (sigmoidoscopy, colonoscopy, biopsy), and manometry. Surgical treatment consists of resection of an enlarged portion of the colon.
The Proctology Department of the Yusupov Hospital offers a full range of diagnostic and therapeutic services for the treatment of various diseases of the rectum, including megacolon. The Yusupov Hospital uses innovative methods for diagnosing and treating diseases of the abdominal cavity and gastrointestinal tract that meet all the requirements of today and the principles of evidence-based medicine. Qualified medical and administrative staff work with patients at the Yusupov Hospital, providing emergency care, care in a clinic and hospital setting, as well as 24-hour support during treatment.
Megacolon in adults: causes of development
Thickening of the colon is associated with hypoganglionosis (underdevelopment) or complete aganglionosis (absence) of ganglion cells of the intermuscular submucosal Meissner and Auerbach plexuses.
And the hypoganglionic zones have a local location in some part of the large intestine and completely affect the entire intestine, spreading to the ileum. Based on all this, anatomically, rectosigmoid, subtotal, segmental, total and rectal forms of megacolon are distinguished. In 90% of patients, areas of aganglionosis are located in the rectosigmoid region.
A segment of the colon deprived of intramural nerve plexuses does not peristalt, but spasms due to the predominance of the influence of sympathetic innervation. Prolonged stagnation of feces in the intestines leads to intoxication of the body, as well as ulcers of the intestinal mucosa.
Tumor in the intestine: signs and early diagnosis of neoplasms
An intestinal tumor is a pathological formation formed as a result of the proliferation of cells in which the processes of reproduction and/or growth rates have significantly changed (benign neoplasms) or the maturation processes have been disrupted (intestinal cancer).
Benign intestinal tumors are neoplasms that develop in different layers of the wall of the small or large intestine and are characterized by slow growth and a relatively favorable prognosis.
A separate type of intestinal neoplasms are heterotopias from other organs (proliferation of cells from other organs) - endometriosis and carcinoid (a hormonally active tumor in structure resembling cancer, but characterized by slow growth and a benign course).
Malignant tumors of the intestine include intestinal cancer. A malignant tumor arises as a result of the rapid division of immature cells or as a result of malignancy of benign tumors.
Signs of an intestinal tumor
The first signs of an intestinal tumor in a person depend on:
- on its location (small or large intestine);
- histological structure and type of growth;
- development period (latent, prodromal and severe symptoms);
- patient's gender;
- the age of the patient and the presence of concomitant pathology;
- forms and stages of the disease.
In the latent or latent period, both with benign neoplasms and the development of malignant intestinal tumors, there are no symptoms of the disease, and the pathological process can be determined during instrumental examinations of the patient (contrast radiography, FGDS) or accidentally during planned or emergency surgical interventions.
The first signs of a tumor in the intestine appear in the prodromal period in the form of nonspecific symptoms:
- persistent dyspepsia (belching, heartburn, bitterness in the mouth, heaviness in the stomach, nausea, and less often vomiting);
- bloating, difficulty passing gas, intestinal colic;
- periodic aching or cramping pain in the abdomen, turning into a constant pain syndrome;
- prolonged diarrhea or constipation, their alternation;
- loss of appetite, weight loss (with malignant neoplasms, there is an aversion to meat or other products);
- pale skin, fatigue, weakness, anemia, difficult to treat with iron-containing drugs (especially in benign vascular tumors - cavernous or capillary hemangiomas, as well as intestinal cancer);
- darkening of stool, which is associated with latent (hidden bleeding);
- prolonged low-grade fever (body temperature does not fall below 37 C);
- mucus, streaks of blood in the stool.
During the period of severe symptoms, there are clear signs of the presence of a neoplasm in the intestinal cavity or germination into neighboring organs:
- progressive deterioration of health and increase in all nonspecific symptoms;
- significant reduction in body weight;
- persistent pain in the area where the tumor is located;
- palpable tumor in the abdomen;
- signs of intestinal obstruction (prolonged retention of stool, gases, increased peristalsis);
- mucus, blood in the stool, sometimes the presence of pus;
- intestinal bleeding;
- pain when urinating, urinary retention (when a tumor grows into the prostate gland and bladder in men);
- the release of gases and feces from the vagina when an intestinal tumor grows into the uterus and vagina and the formation of retrovaginal fistulas are symptoms of an intestinal tumor in women.
Early detection of intestinal tumors
Timely diagnosis of an intestinal tumor and removal of a benign tumor significantly increases the patient’s chances of a complete recovery.
Today, there are various methods for diagnosing the presence of a neoplasm in the intestine:
- “routine” (simple) methods: collection of complaints and medical history, palpation, digital examination of the rectum, radiography using contrast agents (irrigoscopy), FGDS, colonoscopy, transrectal ultrasound;
- new universal methods: determination of tumor markers in blood serum, CT and MRI, positron emission tomography.
Therefore, it is important to know what symptoms exist for an intestinal tumor, and if they appear, contact a medical facility as soon as possible to exclude or confirm the diagnosis.
To diagnose intestinal tumors, specialists at our clinic use Expera endoscopic equipment, which allows for examination with high quality and image resolution. Also, this new generation device has the ability to perform narrow-spectrum gastro- and colonoscopy in NBI mode.
This method allows you to:
- identify a tumor at the earliest stages of its development immediately after the first symptoms appear;
- carry out a simultaneous biopsy to determine the cellular composition of the tumor or with minimal likelihood of suspicion of malignant growth;
- stopping intestinal bleeding;
- removal of a foreign body from the intestine.
Today, endoscopic examination with intravenous sedation (introducing the patient into short-term sleep) is justified, which contributes to the early diagnosis of intestinal tumors and elimination of symptoms (the prognosis of the disease improves).
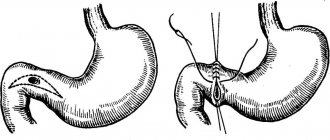
Megacolon in adults: types
Megacolon can be congenital or acquired. Congenital megacolon (Hirschsprung's disease) is characterized by aganglionosis - the absence of nerve plexuses inside the walls of the rectosigmoid colon. The deinnervated section of the intestine is narrowed, lacks peristalsis and is an organic obstacle to the passage of feces.
Congenital megacolon occurs due to:
- anomalies in the development of Favalli-Hirschsprung disease (development of the intramural system of the colon);
- fistulous forms of atresia, stenosis of the rectum and anus (anorectal defects).
The formation of acquired megacolon may be associated with secondary changes in the colon as a result of:
- scars in the colon after injury and inflammation (adhesions, strictures);
- blockage by a tumor;
- endocrine disorders (gigantism, hypothyroidism);
- damage to the central nervous system;
- occurrence of atonic constipation (intestinal atony);
- medicinal action.
Idiopathic megacolon, which is characterized by the absence of any changes in the ganglia of the intermuscular plexuses:
- inert rectum (megarectum);
- megadolichosigma, megadolichocolon;
- dolichomegasigma, dolichomegacolon.
Megacolon in adults: symptoms
The severity of the course and clinical features of the disease are directly related to the extent of the affected area and the compensatory capabilities of the body. In adults with megacolon, flatulence develops, abdominal circumference increases, and chronic fecal intoxication increases. Vomiting with bile occurs periodically. Bowel movement occurs only after performing a cleansing or siphon enema. Feces are characterized by a putrid odor, mucus, blood, and particles of undigested food. Patients with megacolon experience exhaustion, retarded physical development, and anemia.
Progressive chronic constipation and intestinal bloating with megacolon lead to thinning and sagging of the abdominal wall, the formation of the so-called “frog belly”. Through the anterior abdominal wall, peristalsis can be observed in the distended intestinal loops. Expansion and swelling of the colon with megacolon is accompanied by a high position of the dome of the diaphragm, a decrease in the respiratory excursion of the lungs, displacement of the mediastinal organs, and a change in the size and shape of the chest (barrel chest). Against this background, cyanosis, shortness of breath, and tachycardia develop, changes are recorded on the electrocardiogram, and conditions are created for recurrent pneumonia and bronchitis.
Frequent complications of megacolon are dysbiosis and the development of acute intestinal obstruction. With dysbacteriosis, secondary inflammation develops in the intestines, ulceration of the mucous membrane occurs, which is manifested by “paradoxical” diarrhea. The development of the intestines is accompanied by uncontrollable vomiting and abdominal pain. In severe cases - perforation of the colon and fecal peritonitis. When intestinal volvulus or nodulation occurs, strangulation intestinal obstruction may occur. Depending on the severity of megacolon symptoms, there are three main stages:
- megacolon compensation;
- subcompensation of megacolon;
- megacolon decompensation.
Diverticular disease of the intestine (diverticulosis) - symptoms and treatment
A diverticulum is a hernia-like protrusion that can form in the wall of any hollow digestive organ, from the esophagus to the small and large intestines [1]. In this article we will talk about colon diverticula, as they often lead patients to a surgeon and coloproctologist.
Colon diverticula can be either single or multiple.
A condition in which there are many non-inflamed diverticula in the colon is called diverticulosis [9][19]. Typically, patients with this disorder are not bothered by anything. They learn about their disease only after a colonoscopy performed for another disease [1][9]. Sometimes diverticulosis is accompanied by pain and bloating, changes in bowel movements and other symptoms.
When diverticula begin to become inflamed, we are talking about diverticular disease of the intestine . It develops in 20% of people with diverticulosis. 75% of them develop acute diverticulitis, which is accompanied by pain in the left lower abdomen, constipation and fever, and 25% develop complications such as diverticulum perforation, abdominal abscess, peritonitis, intestinal stenosis, internal and external fistulas or bleeding from a diverticulum [8].
Previously, the main cause of colon diverticula was considered to be a deficiency of plant fiber, because a regular lack of vegetables and fruits in the diet leads to the development of constipation and increases pressure in the intestinal lumen [1][7][9][10]. But thanks to research, it has become known that the real causes of the formation of diverticula are disorders in the genes that encode the development of neuromuscular and connective tissue. These genetic changes disrupt the structure and contractile activity of the intestinal wall. In fact, “weak” spots are formed in which diverticula appear [1][2][12]. And fiber deficiency is one of the main risk factors for the development of diverticulosis.
Other risk factors include smoking and alcohol abuse. By avoiding these factors and consuming at least 25-30 g of vegetables and fruits per day, we reduce the risk of developing diverticular disease [3].
Diverticulosis can be diagnosed at any age:
- the proportion of patients under 40 years of age is 5%;
- 40-50 years - 5-10%;
- 50-60 years old - 14%;
- 60-80 years old - 30%;
- over 80 years old - 60-65% [1][2][7][9][19].
Statistics show that diverticula are more often found in older people. But this does not mean that the disease appears with age. It’s just that older people are more likely to undergo emergency operations for peritonitis, and are prescribed an abdominal ultrasound or colonoscopy, for example, if constipation develops. It is possible that these same people could have developed diverticula in their youth.
Megacolon in adults: diagnosis
When diagnosing megacolon, specialists at the Yusupov Hospital take into account data from clinical symptoms, objective examination, results of X-ray and endoscopic diagnostics, laboratory tests (stool for dysbacteriosis, coprograms, histology).
During an examination by a proctologist, an enlarged, asymmetrical abdomen is revealed. On palpation, intestinal loops filled with feces have a doughy consistency, and in the case of fecal stones, a dense consistency. With megacolon, a symptom of “clay” is noted - pressing with fingers on the anterior abdominal wall leaves marks of indentation on it.
Plain radiography of the abdominal cavity with megacolon reveals swollen and dilated intestinal loops of the colon, a high-lying dome of the diaphragm. X-ray contrast irrigoscopy allows you to determine the aganglionic zone - the area of narrowing of the colon with expansion of its overlying sections, the smoothness of their contours, the absence of folding and haustra. In this case, expansion of the rectum (megarectum), sigmoid (megasigma) or the entire colon (megacolon) may predominate. Using sigmoidoscopy and colonoscopy, the large intestine is examined and a transanal endoscopic biopsy is performed. The absence of nerve cells of the Auerbach plexus in the biopsy specimen of the muscular lining of the rectum confirms the diagnosis.
Differential diagnosis for megacolon is carried out with:
- colon tumors;
- chronic colitis;
- irritable bowel syndrome;
- diverticular disease;
- habitual constipation caused by anal fissures.