Gastroenteritis or rotavirus infection (popularly known as stomach and intestinal flu). The causative agents of this disease are various kinds of viruses, but most often it causes intestinal flu - the Rotavirus virus, as well as pathogens such as astroviruses, noroviruses, caliciviruses, adenoviruses. Most often, children and elderly people are exposed to this disease, and the disease is more severe.
The symptoms of Gastroenteritis are well expressed, but in an adult with a strong immune system, this infection can occur latently and not show any symptoms, but a healthy appearance does not indicate that the person is not contagious. The acute period of the disease lasts a week, after 5-7 days the person recovers completely, but still remains dangerous to others.
Symptoms
The disease is transmitted mainly through the fecal-oral (food) route and is highly contagious. Sources include patients still shedding viruses in their feces and asymptomatic infections. Stomach flu is caused by rotaviruses, noroviruses, sapoviruses and adenoviruses.
The main symptoms of stomach flu are diarrhea and/or vomiting. Diarrhea in adults is the passage of at least one (in some definitions more than three) liquid or semi-liquid stools per day. In newborns, infants, and toddlers, diarrhea is considered to be an increase in the number of bowel movements and a fluid or semi-liquid consistency compared to what is considered an illness.
Diarrhea and/or vomiting with intestinal flu may be associated with the following phenomena:
- cramping pain in the abdomen;
- nausea;
- lack of appetite;
- heat;
- Bad mood;
- restless behavior in a child.
How does stomach flu spread?
Symptoms and consequences of intestinal infections
Viruses that cause intestinal or stomach flu are transmitted through the air, are highly contagious and widespread, especially during the cold season. If there is a sick person in the team (even at the initial stage), most likely, several more people will “catch” the virus in the next 1-2 days. The disease can become epidemic.
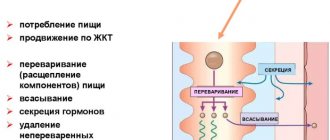
When the pathogen enters the body, intoxication and damage to the gastrointestinal tract occurs, such as acute gastroenteritis. As a result, dysbiosis develops and the process of water absorption is disrupted, which leads to dehydration. Together with water, a person also loses vital minerals - sodium, potassium, chlorine, magnesium. And without these substances, metabolism is impossible, blood clotting function is impaired, and it is difficult to maintain normal blood sugar levels.
Intestinal flu in children
Stomach flu in children can be a serious problem. In such patients, severe dehydration is more common, which requires intravenous drip administration in a hospital setting. Children in the first three years of life are at greatest risk of developing severe diarrhea.
A baby can become infected through contact with a sick child or adult who transmits viruses on hands or objects contaminated with the virus. The likelihood of infection is much higher in nurseries, kindergartens and wards of children's hospitals.
How can you become infected with this disease?
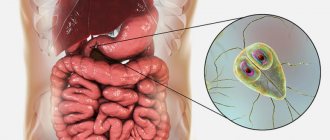
Rotavirus infection is transmitted through food.
Rotavirus infection enters the human body through the gastrointestinal mucosa, and within 16 hours to 5 days the virus begins to develop.
How quickly the disease will develop and how severely it will depend on the concentration of the pathogen and how strong the patient’s immune system is.
The virus is transmitted through food, unwashed vegetables, fruits, and low-quality dairy products. LCD flu can be given another name - “disease of dirty hands.” Infection is possible through tap water (not boiled); even with simple bathing, this infection can enter the body.
Another way through which the infection enters the body is through airborne droplets. When someone with the virus speaks loudly, sneezes without covering their mouth, or coughs, the virus spreads through the air, infecting other people. It is also possible to become infected through household contact, especially in places where there are a large number of people, for example: office premises, kindergartens, schools, shops, etc.
The causative agent of gastrointestinal flu is very resistant to various conditions and influences. It can withstand low temperatures up to freezing, and high temperatures and can also withstand heating up to 60 degrees.
The virus can only be killed with a concentrated disinfectant containing chlorine.
Treatment
methods for intestinal flu in adults and children are the same. They rely on fluid replacement and proper nutrition to prevent dehydration, electrolyte disturbances, and malnutrition. Pharmacotherapy is also used for intestinal flu.
Bowel treatment can be done at home in the absence of symptoms requiring hospitalization. These include a fever greater than 38.5°C, blood in the stool, vomiting that prevents oral fluid intake, and symptoms of severe dehydration. In children, this is loss of consciousness, weakness, sunken and dry eyes, crying without tears, dry mouth and tongue, weight loss.
How to hydrate your body
To irrigate the body during intestinal flu, special medications are recommended that can be purchased at a pharmacy without a prescription. Based on them, a liquid of optimal composition is prepared. If there is no access to a pharmaceutical drug, the patient can be given other lightly salted liquids, such as water, liquid tea, carrots or soup.
You need to drink a lot of liquid. Contrary to popular belief, Coca-Cola is not recommended for stomach flu because sugary carbonated drinks can make diarrhea worse. For the same reason, you should not drink fruit juice. It is worth knowing that cool liquids taken in small sips are better tolerated by patients.
How to prepare rehydration liquid
If it is impossible to use a pharmaceutical drug, you can prepare the irrigation fluid yourself. You will need the following ingredients:
- teaspoon of table salt;
- a teaspoon of baking soda;
- 0.5 cups of orange juice or 2 bananas;
- 4 teaspoons sugar.
All ingredients must be mixed and filled with boiled water to 750 ml.
What can you eat?
It is now believed that people without significant symptoms of dehydration can be fed as before the disease. This applies to both adults and children. The rule also applies to children who are breastfed or formula-fed. The latter need to be fed more often (every 3 hours). During intestinal flu, you should not starve patients or take long breaks from eating!
Diet
Both children and adults during stomach flu should avoid foods with a lot of sugar, fatty foods and foods cooked with fat. You can eat the traditionally recommended carrots, rice porridge or applesauce. However, they do not affect the duration of the disease, although they slightly improve stool consistency.
Drugs
Considering that the most important thing is to replenish fluids and continue nutrition, a child with intestinal flu can be given a probiotic with a proven effect or smecta. There is no justification for using activated carbon or tannins.
Medicines containing loperamide can only be taken by adults!
Laboratory diagnosis of intestinal infections
The most susceptible to intestinal infections are young children under 5 years of age, people with weakened immune systems and/or those suffering from diseases of the gastrointestinal tract.
Therefore, when the first symptoms and discomfort appear, you should not hesitate; it is better to immediately consult a doctor, get tested and begin restorative treatment. To diagnose acute intestinal infections, CITILAB can perform a number of necessary studies using the PCR method. They reliably allow us to identify the genetic material of the pathogen:
- 97-84-104 — Acute viral intestinal infections (enterovirus, rotavirus, norovirus, astrovirus).
- 97-84-102 - Rotavirus types A, C.
- 97-84-103 — Enterovirus.
- 97-84-105 - Norovirus types 1 and 2.
What to do when the first flu symptoms appear?
As soon as you feel flu-like symptoms, you need to take immediate action. Be sure to visit a doctor or call a doctor at home. This is necessary to accurately diagnose the disease and prescribe effective drugs to treat influenza. The doctor will order tests to determine the type of virus.
Patients often ask whether the flu is dangerous for doctors. At the height of the epidemic, they examine and visit dozens of patients with flu-like symptoms, giving the impression that medical workers are invulnerable. In fact, doctors also get sick, and during periods of outbreaks they are also susceptible to viral infections.
When the doctor announces the diagnosis and prescribes medications, you need to start taking it. Until this moment, you can use folk remedies, first of all, drinking plenty of fluids. It helps reduce intoxication and avoid dehydration. The best choice of drinks is herbal teas, fruit drinks, compotes, fruit infusions, kefir and low-fat milk. Coffee is not recommended: it provokes a rapid heartbeat and can have a bad effect on your already depressed state of health. The drink should be warm: hot liquid is contraindicated for the mucous membranes; the slightest damage to them opens the way for bacterial infection.
Ventilate the room more often, this will help reduce the concentration of pathogenic viruses.
At the same time, maintain a comfortable temperature in the room, avoid cold or stuffiness and heat.
People often ask if they can take a shower. The water procedure has a beneficial effect on the body: water removes perspiration, viruses and toxins from the skin. However, poor health can become an obstacle to this: focus on your health status. During this time, you need to avoid physical activity, even if you exercise regularly.
Review your diet: give up heavy fatty foods, smoked foods, and spicy foods. They overload the gastrointestinal tract, which is best avoided in the current state. The other extreme is refusing food due to lack of appetite; this should not be allowed. For flu symptoms, the optimal diet is low-fat warm broths, porridge, cottage cheese.
Remember to maintain bed rest. This is not a whim of doctors, but an objective necessity: if you endure the disease “on your feet,” the risk of complications increases, even very dangerous ones - diseases of the respiratory tract, cardiovascular and nervous systems.
Routes of transmission
In the transmission of infection, the main role is played by airborne droplets: when coughing or sneezing, small drops of saliva or sputum enter the air and spread over a distance of up to 1.5 meters. In the room, the droplets break up into smaller fragments and remain suspended. And the virus itself remains viable for up to several hours. Infection occurs by inhaling this aerosol.
The second most important is the contact route of spread: a sick person, sneezing, covers his face with his hand and then spreads the virus by touching objects in the environment. Therefore, using a handkerchief and washing your hands; actually reduce the risk of spreading infection.
The average incubation period is up to 2 days.
Prevention of respiratory diseases
A sick patient should reduce social contacts, especially with the elderly, pregnant women and people with chronic diseases. To reduce the risk of infection, you must follow a few simple rules:
- washing hands thoroughly with soap
- limiting contacts during epidemics: it is worth limiting close contact with a person who has catarrhal manifestations of ARVI (coughing, sneezing, runny nose)
- irrigating the nose with saline solutions after visiting public places (in the autumn-winter period, when the heating is on, dry air in the room negatively affects the nasal mucosa and it becomes more vulnerable to the penetration of various pathogens, and the use of saline solutions moisturizes the nasal mucosa)
- regular ventilation and wet cleaning of premises
- general strengthening methods, which include hardening, the use of vitamins and dietary supplements, the elimination of bad habits, and a healthy balanced diet help strengthen the immune system
Vaccination remains the most effective way to prevent influenza . The influenza vaccine protects the vaccinated person, even if the circulating viruses are not exactly the same as the vaccine viruses. Vaccination allows you to avoid a severe course of the disease and reduce the likelihood of complications and death. It is especially important to get vaccinated against influenza for people with chronic illnesses and people living with those at high risk11.
Complications of influenza
With prolonged progression of the disease, as well as with non-compliance with the doctor’s instructions - for example, if bed rest is violated during the acute period of the disease, with premature interruption of antiviral treatment, the development of serious, life-threatening complications from various organs and systems is possible.
Flu can lead to:
- otitis media,
- sinusitis,
- pharyngitis,
- laryngitis,
- tracheitis,
- neuralgia,
- sore throat,
- bronchitis,
- pneumonia,
- pulmonary edema,
- meningitis,
- respiratory failure
- a number of other dangerous diseases of the cardiovascular, excretory and respiratory systems.
After suffering from pneumonia, residual effects in the form of bronchiectasis and pneumosclerosis often persist.
Pregnant women infected with influenza virus or ARVI are also at high risk of complications and mortality. Mortality rates among pregnant women with severe influenza infection vary in different countries and in Russia are 0.3%. Most deaths occur in pregnant women in the third trimester. Healthy expectant mothers in the third trimester have a risk of severe respiratory infection comparable to that of nonpregnant patients with chronic comorbidities.[ii]
How does flu infection occur?
The source of an infectious disease can be a sick person with clinically obvious and atypical (implicit) manifestations of the disease. The greatest infectiousness is observed during the first 3 days from the onset of clinical manifestations. Isolation of the pathogen lasts approximately 5-7 days in an uncomplicated form (faster formation of immunity and elimination of the virus) and up to three weeks in a severe and complicated form (slow formation of immunity, including due to a possible initial weakening of protective mechanisms - concomitant diseases, age ).
The transmission mechanism is airborne droplets (aerosol route), contact route is possible (when using shared utensils, kissing, contaminated hands). Autumn-winter seasonality with an epidemic component is quite typical, repeating at approximately the same interval. Sporadic incidence of ARVI is observed at any time of the year.
Recent studies have shown that influenza viruses live on human hands for 5 minutes. If during this time a person touches some things, the viruses transfer to them and live there much longer. They last for 24 to 48 hours on metal and plastic, and ten days on glass. According to statistics, one flu patient on average infects five people.
Which doctor should I see if I have a cold?
An initial consultation with a therapist is required. It may be necessary to examine other specialists, for example, an infectious disease specialist, an ENT specialist, an ophthalmologist. If this data is not enough, then laboratory tests can be performed.
Methods for clinical and laboratory diagnosis of respiratory infections include the following9:
- PCR diagnostics based on detection of RNA or DNA viruses
- immunofluorescence and enzyme immunoassay
- serological methods
- test for rapid diagnosis of influenza
- rapid diagnosis of beta-hemolytic streptococci
- microbiological cultures to determine the sensitivity of microflora to antimicrobial drugs.
The basic principle of diagnosing ARVI and influenza is to compare the general clinical picture of the disease (a set of complaints, symptoms) with the results of laboratory tests. The specialist should also take into account the epidemiological situation in the region, information about circulating strains of viruses, the emergence of new pathogens and mutations of viruses.
How often do we get ARVI?
Acute respiratory viral infections (ARVI) are the most common form of acute diseases. Approximately 80-90% of residents of the Russian Federation fall ill with ARVI every year. And during epidemics, almost every person gets sick once or more1. And all over the world, according to the World Health Organization (WHO), every adult on average gets sick 2 to 4 times a year2.
This is due to the high contagiousness of viruses and their wide variety. Moreover, different viruses can change due to mutations and become more infectious.