Metronidazole (MT) is a widely used antimicrobial and antiparasitic drug [3–6]. Moreover, in clinical practice, the scope of its application is often associated not only with the effect on microorganisms, but also with its electron-acceptor property [7]. Its last property is most widely used in oncology to increase the effectiveness of radiotherapy for malignant tumors. Thus, to increase the effectiveness of radiation therapy for rectal tumors, 5-fluorouracil (5-FU) and MT are administered to patients during irradiation [8]. In addition, cancer patients after surgical treatment and against the background of adjuvant chemotherapy are prescribed MT to prevent local infectious complications [9]. At the same time, there is information in the literature about the effect of MT on the toxicity of cytostatics. In particular, MTX has been shown to increase the toxicity of methotrexate and 5-FU when administered together to tumor-inoculated mice [10]. Clinical studies found that the administration of the alkylating agent bisulfan against the background of MT led to a significant increase in liver enzymes compared to the control group that received the cytostatic alone [11]. It has also been shown that MT is able to influence the pharmacokinetics of the immunosuppressant tacrolimus, significantly increasing its biological activity and, at the same time, toxicity. Thus, in order to avoid drug overdose during the use of MTX, the course dose of the immunosuppressant tacrolimus had to be reduced by 4 times [12]. Although the very fact of increased toxicity of drugs when used together with MTX and the need to use MTX in cancer patients is beyond doubt. One of the promising directions to reduce the effect of MT on the toxic properties of cytostatics may be the development of optimal regimens for administering these drugs relative to each other [13].
The purpose of this work was to study the influence of different time intervals between the administration of MT and 5-FU on their biological effects. The choice of drugs is determined by the breadth of their use in oncological practice for various forms of cancer.
Material and methods
Animals
. Mice of the CBA/Lac male and C57Bl/6 female line weighing 18–20 g at the age of 1.5 months were obtained from the Stolbovaya nursery in the Moscow region. MT and 5-FU are official drugs. The doses used were the maximum tolerated or were close to those, which was due to the need to register the effect of increasing the toxicity of the combined use of drugs. MT was used once at a dose of 1 g per 1 kg of animal body weight (maximum tolerated dose 1.4 g/kg). The antitumor efficacy of the combined action of the drugs was studied in the following regimens: 5-FU was administered at a dose of 100 mg/kg subcutaneously, and MT was administered at a dose of 1 g/kg intraperitoneally 20 minutes, 1 hour, 4 hours, 12 hours before the administration of 5-FU. There were 10 animals in each group. When assessing the toxicity of the studied combination, MT was administered intraperitoneally at a dose of 1 g/kg 20 minutes, 1 and 4 hours before subcutaneous administration of 5-FU. Treatment began 7 days after tumor cell transplantation. Each group contained 10 CBA/Lac mice. The death of animals was recorded within 30 days after administration of the drugs, assessing the reliability of differences in their life expectancy in the groups that received one antimetabolite and an antimetabolite with a modifier. There were 10 animals in each group. In control groups, mice were administered 5-FU or M.T. alone. The “pure” control group received isotonic sodium chloride solution.
Transplantable tumors
.
Melanoma B16 and mucinous ovarian cancer CaO-1 were obtained from the bank of tumor strains of the Russian Cancer Research Center named after. N.N. Blokhin" of the Russian Ministry of Health. Transplanted CaO-1 ovarian carcinoma has been described as highly sensitive to the action of 5-FU [1, 2]. Melanoma B16 is resistant to 5-FU. The experiments used the 3rd passage of the tumor in vivo
.
A suspension of tumor tissue was performed at 105 cells in 0.1 ml of nutrient medium 199. B16 melanoma cells were transplanted into C57Bl/6 mice, CaO-1 ovarian carcinoma cells were transplanted into CBA/Lac mice. The antitumor effect was assessed by tumor volume and tumor growth inhibition (TGR). The volume of the tumor over time (in mm3) was determined by the formula V=a
2
b
, where
a
is the smallest linear size of the tumor in millimeters;
a, b
—the largest linear size of the tumor in millimeters.
Tumor growth inhibition was calculated using the formula: TPO = V
avg.
experience – V
average control /
V
average control. The toxic effect of drugs and their combinations was assessed by the number of leukocytes in the peripheral blood of animals, changes in their body weight and the dynamics of their death.
Instructions for use METRONIDAZOLE tablets
To avoid the development of resistance of microorganisms, metronidazole should only be used to treat infections caused by metronidazole-sensitive strains (according to microbiological examination of the material or epidemiological data).
Trichomoniasis with clinical symptoms.
Metronidazole is indicated for the treatment of trichomoniasis with clinical symptoms in women and men, if the presence of trichomonas has been confirmed by appropriate laboratory tests (smear and/or culture).
Asymptomatic trichomoniasis.
Metronidazole is indicated for the treatment of women with asymptomatic trichomoniasis (endocervicitis, cervicitis or cervical erosion). Because there is evidence that the presence of trichomonas may interfere with the accurate evaluation of cytological smears, additional smears should be performed after eradication of the parasite.
Treatment of a spouse without clinical manifestations.
T. vaginalis infection is a sexually transmitted disease. Thus, asymptomatic sexual partners should be treated at the same time to prevent reinfection from the partner, even if the pathogen is not isolated. The decision about whether to treat an asymptomatic male partner in whom trichomonas is not detected, or where testing has not been performed, is an individual one. In making this decision, it should be noted that there is evidence that a woman can become infected again if her husband is not treated. In addition, because there are significant difficulties in isolating the pathogen from an asymptomatic patient, negative smear and culture results should not be relied upon. In any case, in case of re-infection, the spouses should be treated with metronidazole at the same time.
Amoebiasis.
Metronidazole is indicated for the treatment of acute intestinal amebiasis (amebic dysentery) and liver abscess caused by amoebae. When treating a liver abscess caused by amoebas with metronidazole, the need for aspiration or drainage of pus cannot be excluded.
Anaerobic bacterial infections.
Metronidazole is indicated for the treatment of severe infections caused by susceptible anaerobic bacteria. Necessary surgical procedures must be performed in combination with metronidazole therapy. In case of mixed aerobic and anaerobic infection, appropriate antimicrobial agents should be used in addition to metronidazole. When treating severe anaerobic infections, metronidazole is usually given first. Intra-abdominal infections, including peritonitis, intra-abdominal abscess and liver abscess, are caused by Bacteroides, including the B. fragilis group (B. fragilis, B. distasonis, B. ovatus, B. thetaiotaomicron, B. vulgatus), Clostridium, Eubacterium, Peptococcus niger and Peptostreptococcus .
Infections of the skin and skin structures,
caused by Bacteroides (including the B. fragilis group), Clostridium, Peptococcus niger, Peptostreptococcus and Fusobacterium.
Gynecological infections,
including endometritis, endomyometritis, tubo-ovarian abscess and infections after gynecological surgery caused by Bacteroides (including B. fragilis group), Clostridium, Peptococcus niger and Peptostreptococcus.
Bacterial septicemia,
caused by Bacteroides (including the B. fragilis group) and Clostridium.
Bone and joint infections
caused by Bacteroides species (including the B. fragilis group) as adjunctive therapy.
CNS infections
including meningitis and brain abscess caused by Bacteroides (including B. fragilis group).
Lower respiratory tract infections,
including pneumonia, empyema and lung abscess caused by Bacteroides (including B. fragilis group).
Endocarditis,
caused by Bacteroides (including the B. fragilis group).
Research results
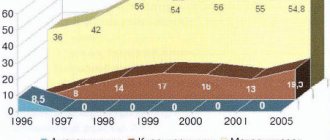
In Fig. Figure 1 shows the growth dynamics of the CaO-1 ovarian carcinoma tumor in the control and against the background of exposure to 5-FU and M.T. Introduction by M.T. intraperitoneally at a dose of 1 g/kg on the 7th day after tumor transplantation did not have a significant effect on the dynamics of its growth. Subcutaneous administration of 5-FU at a dose of 100 mg/kg on the 7th day after tumor transplantation caused a delay in tumor release by more than 2 weeks. Subcutaneous administration of 5-FU 1 hour after intraperitoneal injection of MT enhanced the effect of the cytostatic agent, increasing the time of tumor emergence from 14 days when exposed to 5-FU alone to 17 days. A similar effect was observed when exposed to MT 20 min before injection of the cytostatic. However, with this scheme of administration of 5-FU and MT, the death of up to 40% of animals was observed. The death of animals suggests increased toxicity of this combination of drugs. Administration of the cytostatic after 4 and 12 hours did not affect the effect of the cytostatic.
Rice. 1. Influence of M.T. on the antitumor effect of 5-FU using the example of the growth dynamics of CaO-1 carcinoma. The x-axis shows days after tumor transplantation; the ordinate is the tumor volume in mm3.
In Fig. Figure 2 shows the dynamics of the growth of CaO-1 ovarian carcinoma in the control and against the background of drug exposure with an increase in the interval between the administration of the antimetabolite and MT to 12 hours. As can be seen from the above figure, in the control group there is rapid growth of the primary node. Introduction by M.T. intraperitoneally at a dose of 1 g/kg on the 7th day after tumor transplantation does not have any significant effect on tumor growth. Subcutaneous administration of 5-FU at a dose of 100 mg/kg on the 7th day after tumor grafting caused a shorter delay in tumor exit. Co-administration of MT and 12 hours later 5-FU did not increase the antitumor effect of the antimetabolite. However, increasing the administration interval to 12 hours led to the death of no more than 10% of the animals in this experimental group. The absence of animal death indicates a decrease in the toxicity of the drug combination with this administration regimen compared to the previous one.
Rice. 2. Influence of M.T. on the antitumor effect of 5-FU using the example of the growth dynamics of CaO-1 carcinoma at an interval of drug administration of 12 hours. The x-axis shows days after tumor transplantation; the ordinate is the tumor volume in mm3.
In Fig. Figure 3 shows the growth dynamics of B16 melanoma in the control group and against the background of drug exposure. Introduction by M.T. at a dose of 1 g/kg body weight of animals on the 7th day after tumor inoculation did not have a significant effect on tumor growth. 5-FU at a dose of 100 mg/kg on the 7th day after tumor transplantation did not inhibit tumor growth. Subcutaneous administration of 5-FU 20 minutes after MT also did not lead to the appearance of an antitumor effect of the antimetabolite. These data indicate that MT does not have a modifying effect on melanoma cells, which would overcome the initial tumor resistance to this antitumor drug.
Rice. 3. Influence of M.T. on the antitumor effect of 5-FU using the example of the growth dynamics of B16 melanoma. The x-axis shows days after tumor transplantation; the ordinate is the tumor volume in mm3.
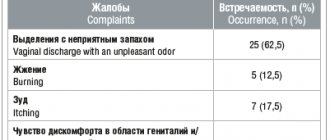
In a special series of experiments, the effect of MT on the toxicity of 5-FU was assessed. In table Figure 1 presents the results of experiments to study the effect of the interval between the administration of 5-FU and MT on the death of animals. As follows from the data in table. 1,5-FU did not cause death in mice at a dose of 200 mg/kg. However, the introduction of the MT modifier 20 minutes before the injection of the antitumor drug led to the death of 70% of the animals, which indicates an increase in the toxicity of the chemotherapy drug under the influence of MT. 5-FU at a dose of 300 mg/kg led to lethal effects in 70% of individuals, and its application 20 minutes after administration of MT (1 g/kg) caused 100% death. At the same time, there is a significant decrease in the average life expectancy of dead animals from 14 to 9.9 days. Increasing the interval between the introduction of the modifier and 5-FU to 1 hour reduced the death of animals in this group by up to 90%. The decrease in toxicity of the drug combination can be explained by the rapid metabolism of MT in the mouse body. It is obvious that during this period the concentration of MT in the blood decreases and its effect on the toxicity of 5-FU decreases.
Table 1. The influence of various modes of administration of the MT modifier on the toxicity of 5-FU Table 1. The influence of various modes of administration of the MT modifier on the toxicity of 5-FU
This assumption is confirmed by data indicating that a further increase in the interval between drug administration to 4 hours leads to an even greater reduction in the toxicity of the combined action of MT and 5-FU. The modifier itself in mono mode did not cause the death of animals.
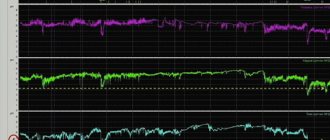
In table Figure 2 presents the results of experiments studying the effect of an antitumor drug and MT, as well as their combination on the number of leukocytes in the peripheral blood of mice. In the control group of animals, the number of leukocytes in the peripheral blood was stable throughout the entire observation period with average values from 9.6 to 11.2∙103 cells/μl. The introduction of the MT modifier at a dose of 1 g/kg caused a decrease in the number of leukocytes in the peripheral blood to 7.6∙103 cells/μl on the 4th day after the administration of MT. In the following days, there was a restoration of the number of cells in the peripheral blood almost to the initial levels. In the group of animals that received 5-FU at a dose of 100 mg/kg, there was also a decrease in the number of leukocytes in the peripheral blood to 7.0∙103 cells/μl on the 4th day after administration of the antitumor drug. In the following days, there was also a restoration of the number of cells in the peripheral blood almost to the initial levels. In the group of animals that were administered the modifier 2 hours before the injection of the antitumor drug, there was also a decrease in the number of leukocytes in the peripheral blood to 6.1∙103 cells/μl on the 4th day after the administration of the antitumor drug. In the following days, a restoration of the number of cells in the peripheral blood was observed. However, there was no restoration to the original number of cells in the peripheral blood of mice during the studied period of time. The latter circumstance can be explained by the increased toxicity of this combination of drugs compared to their separate use. Increasing the interval between the administration of the modifier and the antitumor drug to 4 hours led to the fact that the dynamics of changes in the number of leukocytes in the peripheral blood was similar to that in the group of mice that received 5-FU alone.
Table 2. Effect of 5-FU and its combination with MT on the average number of leukocytes in the peripheral blood of mice (∙103 cells/μl) Note. Here and in the table. 3:* — p<0.05 significant differences between experimental groups and control (M±m).
As follows from table. 3, in the control group of animals, the average body weight was stable throughout the entire observation period. The introduction of the MT modifier at a dose of 1 g/kg causes a decrease in weight by approximately 5% (from 21.5 to 20.5 g). In the group of animals that received 5-FU at a dose of 100 mg/kg, there was also a decrease in animal body weight by approximately 5%. In the group of animals that received the modifier 2 hours before the administration of the antitumor drug, there was a significant decrease in the body weight of the animals, reaching 16.1 g by the 7th day (25% decrease), which indicates an increase in the general toxic effect of the drug combination compared to their separate use. When the interval between the administration of the modifier and the antitumor drug is increased to 4 hours, the loss of animal body weight does not differ from this indicator in groups of animals with separate use of these drugs.
Table 3. Effect of 5-FU and its combination with MT on the average body weight of mice, g
Discussion
This study provides data on the effect of MT on the specific activity of the antitumor drug 5-FU. The therapeutic effect of the drug and its combination with MT was assessed by its effect on the dynamics of tumor growth in mice - B16 melanoma and CaO-1 ovarian carcinoma.
5-FU inhibited the growth of CaO-1 ovarian carcinoma. Influence of M.T. The antitumor efficacy of 5-FU depended on the interval between the administration of MT and the cytostatic agent. An increase in the antitumor effect of 5-FU was observed when the modifier was administered 20 minutes and 1 hour after the cytostatic agent. MT and the synergistic effect of the combination decreased with increasing interval between administrations of these drugs.
The lack of enhancement of the antitumor effect of the combination in mice engrafted with B16 melanoma resistant to 5-FU indicates that MT is not a modifier of B16 melanoma resistance to 5-FU. The above suggests that MT has an effect on 5-FU metabolism. This position is confirmed by a series of experiments devoted to the study of the toxicity of the combination depending on the dose of 5-FU and the time interval between administrations of MT and cytostatic. According to the data obtained, the time interval of 5-FU should be at least 4 hours. With a shorter interval (in particular, after 2 hours), the toxicity of the cytostatic increases 1.5-2 times, which leads to an increase in the death of animals.
Metronidazole
Gastrointestinal disorders: epigastric pain. nausea, vomiting. diarrhea, glossitis, stomatitis, “metallic” taste in the mouth, decreased appetite, anorexia, dry oral mucosa. constipation, pancreatitis (reversible cases), discoloration of the tongue, coated tongue" (due to the proliferation of fungal microflora).
Immune system disorders: angioedema, anaphylactic shock.
Nervous system disorders: peripheral sensory neuropathy, headache, convulsions, dizziness, the development of encephalopathy and subacute cerebellar syndrome (impaired coordination and synergism of movements, ataxia, dysarthria, gait disturbances, nystagmus, tremor) has been reported, which are reversible after discontinuation of metronidazole , aseptic meningitis.
Mental disorders: psychotic disorders, including confusion, hallucinations; depression, insomnia, irritability, increased excitability.
Visual disturbances: transient visual disturbances such as diplopia, myopia, blurred contours of objects, decreased visual acuity, impaired color perception: neuropathy/optic neuritis.
Blood and lymphatic system disorders: agranulocytosis, leukopenia, neutropenia, thrombocytopenia.
Disorders of the liver and biliary tract: increased activity of liver enzymes (aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase), development of cholestatic or mixed hepatitis and hepatocellular liver damage, sometimes accompanied by jaundice; In patients treated with metronidazole in combination with other antibacterial agents, cases of liver failure requiring liver transplantation were observed.
Skin and subcutaneous tissue disorders: rash, itching, skin flushing, urticaria, pustular skin rash, Stevens-Johnson syndrome. toxic epidermal necrolysis.
Disorders of the kidneys and urinary tract: staining of urine in a brownish-reddish color, caused by the presence of a water-soluble metabolite of metronidazole in the urine, dysuria, polyuria. cystitis, urinary incontinence, candidiasis.
General disorders and disorders at the injection site: fever, nasal congestion, arthralgia, weakness.
Laboratory and instrumental data: flattening of the T wave on the electrocardiogram.