A hiatal hernia (HH) is a disease characterized by pathological movement of internal organs into the chest, which should normally be located under the diaphragm. We are talking about the abdominal esophagus, stomach or intestines (rarely).
The disease is more common in older people. It is noteworthy that hiatal hernia often occurs without any clinical manifestations and sometimes goes unnoticed. Clinical manifestations of hiatal hernia are often similar to other diseases. Thus, the patient is often treated for gastritis or stomach ulcers, forgetting to exclude a hernia. At the CELT clinic, gastroenterologists perform all the necessary examinations to establish an accurate diagnosis and adequate treatment.
At CELT you can get advice from a gastroenterologist.
- Initial consultation – 4,200
- Repeated consultation – 3,000
Make an appointment
Causes of the disease
A hernia can be diagnosed at birth and be congenital. The pathology develops as a result of underdevelopment (shortening) of the esophagus and requires timely surgical correction. Congenital hiatal hernia is a rare pathology.
An acquired hernia develops due to a weakening of the ligamentous apparatus, as a result of which the esophageal opening of the diaphragm expands. This occurs for various reasons:
- In persons with connective tissue weakness, suffering from related diseases (for example, varicose veins and others).
- As a result of increased intra-abdominal pressure, which is facilitated by pregnancy, a high degree of obesity, ascites, trauma, heavy lifting, persistent cough in chronic pathology of the bronchopulmonary system, etc.
- Increased motility of the gastrointestinal tract.
- Shortening of the esophagus due to its deformation resulting from burns or various inflammatory diseases.
- Asthenia of the patient against the background of sudden weight loss.
Classification
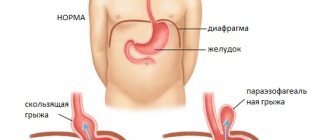
Various anatomical features of the hiatal hernia make it possible to distinguish the following types of acquired disease:
- Sliding (axial or axial).
- Paraesophageal (permanent).
- Mixed (combines the two above mechanisms).
Axial hernia is the most typical hernia. A characteristic feature of this variety is the possibility of spontaneous return of internal organs back into the abdominal cavity when changing body position. The lower segment of the esophagus and the cardiac part of the stomach are localized above the diaphragm during overeating and during the adoption of a horizontal body position.
But not every hernia can be repaired on its own. The paraesophageal hiatal hernia often becomes strangulated, which is fraught with serious consequences for the body. It is distinguished from an axial hernia by the anatomically correct location of the lower esophagus and the upper part of the stomach under the diaphragm. The stomach gradually moves into the chest, first its fundic section, then the antrum. In rare cases, the entire organ appears above the diaphragm, but the gastroesophageal junction continues to maintain its location in the abdominal cavity.
If the hernial sac is formed, among other things, by the gastroesophageal junction, we are talking about a mixed hernial hernia.
Separately, congenital hiatal hernia is distinguished, in which the intrathoracic location of the stomach is noted due to a shortened esophagus.
Based on the radiological signs and size of the hernial protrusion, there are 3 degrees of hernial hernia:
- The first is that the abdominal esophagus penetrates the chest, and the stomach is tightly adjacent to the diaphragm.
- The second is that the stomach is on a par with the diaphragm.
- Third, the contents of the hernial sac include both the lower segment of the esophagus and part of the stomach. Sometimes there are intestinal loops above the diaphragm.
Hiatal hernia
A hiatal hernia (HH) is a displacement of the abdominal part of the esophagus and stomach into the chest cavity through the esophageal opening of the diaphragm.
The main complication of hiatal hernia is gastroesophageal reflux disease (GERD). This is a condition in which acidic stomach contents enter the esophagus.
Complications of GERD:
- Erosion and ulcer of the esophagus.
- Esophageal stricture.
- Baret's esophagus (precancerous condition).
- Infringement of the abdominal organs (with paraesophageal hernias).
The distribution of GERD throughout the world ranges from 8-27.8% per 100 thousand population. In Russia it is 23.7% per 100 thousand population.
Types of hiatal hernia.
A) Sliding - part of the esophagus and stomach in a vertical position returns to the abdominal cavity. B) Fixed - part of the esophagus and stomach remain in the chest cavity (fixed with adhesions).
A) Cardiac - only the cardiac part of the stomach is displaced. B) Cardifundal - the cardiac part and the fundus of the stomach are displaced. C) Subtotal - 2/3 of the stomach is located above the diaphragm. D) Total - the entire stomach is located above the diaphragm. D) Paraesophageal - the cardiac part of the stomach remains in the abdominal cavity, and the abdominal organs (stomach, colon, greater omentum) are displaced above the diaphragm.
Risk factors.
- Increased body weight.
- Intake of fatty foods, coffee and carbonated drinks.
- Drinking alcoholic beverages.
- Smoking.
Symptoms.
1. Esophageal symptoms.
- Heartburn.
- Belching, regurgitation (rejection of previously eaten food).
- Dysphagia.
2. Extraesophageal symptoms.
- Cough and wheezing.
- Hoarseness, sore throat.
- Otitis.
- Non-cardiac chest pain.
- Erosion of tooth enamel and other manifestations of the teeth.
- Anemia.
Diagnostics.
- X-ray examination with contrast agent (polypositional).
- EGDS (if necessary, taking a biopsy).
- Esophageal manometry (study of esophageal motility).
- Daily pH-metry.
Treatment.
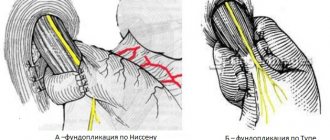
The main method of treatment is complex drug therapy. If the course of therapy is ineffective and there are complications, surgical treatment is indicated. An operation aimed at eliminating reflux is called fundoplication. Main types of fundoplication: 1. Fundoplication according to Nissen, according to A.F. Chernousov (fundoplication 360* circular). 2. Fundoplication according to Toupet (fundoplication 270* partial).
The choice of type of fundoplication is made only after a comprehensive diagnostic examination.
Employees of the department of high-tech surgery of the Moscow Scientific Research Center named after. A.S. Loginova, these operations are performed using low-traumatic approaches (laparoscopic operations, robotic operations). The postoperative period is 1-2 days. The rehabilitation period is 1-1.5 weeks.
Clinical symptoms
Half of the cases are characterized by the absence of symptoms or mild clinical manifestations. This applies to small-sized hiatal hernias. The larger the hernial protrusion, the more pronounced the symptoms are observed.
The disease is characterized by pain, but its localization may vary. In addition to the epigastric region (the “solar plexus” area), pain sensations can be concentrated behind the sternum with irradiation to the back and between the shoulder blades (simulating a heart attack) or mask the disease as pancreatitis (have a shingles nature).
What signs of pain indicate the presence of a hiatal hernia?
- The appearance of pain after eating, lifting heavy objects, with bloating and taking a horizontal position of the body, when bending the body forward.
- Improvement after vomiting, belching, drinking water or taking an upright body position.
Symptoms accompanying severe pain when a hernia is strangulated:
- nausea;
- increased respiratory rate;
- vomiting streaked with blood;
- increased heart rate;
- cyanosis of the skin and mucous membranes;
- lowering blood pressure.
Sometimes the hiatal hernia causes cardiac arrhythmias. This must be taken into account during long-term and unsuccessful treatment with a cardiologist.
Gastroesophageal reflux disease (GERD) is considered a frequent companion of hiatal hernia, which provokes the appearance of a new symptom complex resulting from digestive disorders:
- vomiting air, eaten food or bile.
- Regurgitation not preceded by nausea. The symptom occurs when the body is positioned horizontally at night, following a heavy dinner, and can lead to the development of complications in the form of diseases of the bronchopulmonary system.
Other clinical manifestations characteristic of hiatus hernia:
- Dysphagia is a specific symptom characterized by impaired movement of food through the esophagus after swallowing. This complaint is provoked by drinking hot or cold water, swallowing a poorly chewed food bolus or large amounts of liquid, as well as stress factors.
- Severe heartburn.
- Persistent hiccups.
- Burning sensation in tongue.
- Hoarse voice.
Diagnostics
Diagnosis of hiatal hernia includes the following instrumental examination methods:
- The main method for diagnosing hiatal hernia is radiography of the esophagus with contrast.
- Endoscopic examination (esophagoscopy - examination of the esophagus, fibrogastroscopy - examination of the gastric mucosa). This method reveals inflammatory phenomena (esophagitis, gastritis or ulcers) and pathological displacement of organs.
- An endoscopic biopsy is performed if a cancerous tumor is suspected.
- Esophageal manometry evaluates motility, the condition of the esophageal sphincters, and the effectiveness of treatment.
- pH testing examines the acidic environment of the digestive tract.
- Impedance measurements are used to determine the nature of the digestive tract environment (the method is based on resistance measurements).
- Gastrocardiomonitoring involves conducting electrocardiography and determining the acidity of digestive juice.
Laboratory methods include examining stool for occult blood, which reveals hidden bleeding from the gastrointestinal tract.
Timely contact with a gastroenterologist and accurate diagnosis can prevent the development of complications such as peptic ulcers, bleeding, cicatricial narrowing and perforation of the esophagus, strangulated hernia, cardiac arrhythmia and cancer.
Transmigration of the mucous membrane and hiatal hernia
A large fixed hernia is recognized relatively easily. Even before receiving the contrast mass, an accumulation of gas is detected in the posterior mediastinum, bordered by a narrow strip - a reflection of the wall of the hernial sac. A suspension of barium sulfate fills the part of the stomach that has fallen into the chest cavity, so you can immediately determine the size of the hernia. The location of the hiatus, which in such cases is a hernial orifice, is indicated by notches on the contours of the stomach. When diagnosing paraesophageal hernias, there is also no particular doubt. The esophagus is well filled with a contrasting mass, passes past the hernia and reaches the cardia, which appears at the level of the hiatus or below it. From the stomach (and not from the esophagus), the barium suspension enters the hernia. The latter is visible both in the vertical and horizontal position of the patient, and is located above the diaphragm and usually includes only part of the stomach. However, cases of simultaneous presence of omentum and individual intestinal loops in the hernia have been described. There have also been cases of strangulation of a fundic paraesophageal hernia (a hernia that includes part of the vault of the stomach is called a fundic hernia). The gas bubble in the mediastinum increases sharply, and the horizontal level of the liquid contents of the hernia stands out against its background. In addition, the collapse of the intestines and the absence of gas accumulations in the intestinal loops are striking.
Detection of small axial hernias requires certain tactics. X-ray examination should be carried out both in a vertical and (necessarily) in a horizontal position of the patient. X-ray examination is very effective when the patient is in a horizontal position on his stomach with a slight rotation. The rotation angle is chosen so as to obtain an image of the supradiaphragmatic segment of the esophagus, the diaphragm and the subdiaphragmatic segment together with the cardia. The radiologist must study the condition of the esophagus in all phases - contraction, relaxation, pneumorelief, supplementing radiography with targeted images. With the first sip of the contrast mass in an upright position, the patient may notice some expansion of the distal part of the esophagus, in particular the vestibule, or even retraction of the latter into the hiatus area. In the medial part of the gastric bladder, a shadow of swollen folds of the mucous membrane often appears; It is characteristic that this shadow changes shape and outline during peristaltic contractions. The axial hernia itself in the vertical position of the patient is visible only when it is fixed, which generally happens infrequently.
In its expanded form, all radiological semiotics are determined in the horizontal position of the patient. The first sign, which seems to signal the possibility of a hiatal hernia, is the unusually high localization of the upper esophageal sphincter, i.e., the place of transition of the tubular part of the esophagus into its ampulla. The second sign is the presence of the vestibule and cardia above the esophageal opening. The level of cardia should always be established, since it is taken into account when choosing an operative approach. The radiologist is in danger of mistaking the esophageal ampulla for a hernia. Meanwhile, their differences are obvious. The ampulla is part of the esophagus, a direct continuation of its axis, a pear-shaped extension of the supradiaphragmatic segment. It appears with a deep breath and disappears with exhalation, when the walls of the esophagus collapse. In relation to the hernia, the supradiaphragmatic segment is located eccentrically. On inspiration, an ampulla forms above the hernia. On exhalation, the hernia persists. Small peristaltic retractions may occur on the contours of the ampulla, which does not happen with a hernia. With a hernia, the subphrenic segment of the esophagus is missing. An indicative symptom of a hernia is the presence in the supradiaphragmatic formation of several tortuous folds of the gastric mucosa (and not narrower and fewer esophageal folds). The folds converging and intertwining in the hernial opening and above it, as well as the flow of barium sulfate between them and the walls of the esophagus can form a curious figure of a “corrugated collar”. The contrast mass is retained in the hernia for some period of time. With a hernia, the esophageal opening is enlarged, and the gastric bladder is reduced and deformed. It should be emphasized once again that, unlike a paraesophageal hernia, the filling of an axial hernia occurs from the esophagus.
X-ray examination plays an important role in recognizing complications of hiatal hernia and, above all, esophagitis. Esophagitis is caused by gastroesophageal reflux, which almost always accompanies a hernia. The folds of the mucous membrane in the esophagus are thickened, the outlines of its distal segments become wavy. Peptic esophagitis may be accompanied by cicatricial shortening of the esophagus, which contributes to the development of a hernia or is even one of the pathogenetic factors in its occurrence. In such cases, it is necessary to differentiate between a hernia and a congenital anomaly - a short esophagus with a thoracic location of the stomach. This anomaly is quite typical: the esophagus is straightened, ending high in the chest cavity with a short connection to the stomach. The latter has an elongated cylindrical or conical shape. However, with this anomaly there is also gastroesophageal reflux and peptic esophagitis and ulcers can develop, then the differential diagnosis of congenital and acquired hernia is difficult.
Significant difficulties may arise when diagnosing a combination of a hernia with a peptic ulcer and cardiac cancer . Due to unusual topographic-anatomical relationships, spasms, cicatricial constrictions, a very motley and bizarre x-ray picture is created. Only with the help of a series of targeted radiographs in different positions of the patient’s body is it possible to distinguish between the shadows of the esophageal and gastric folds and the accumulation of barium sulfate in ulcerations, as well as changes in the relief of the mucous membrane and the contours of the esophagus and stomach caused by the tumor.
It remains to add that after surgical removal of the hernia, the X-ray examination should be repeated. It allows you to assess the usefulness of the operation, the state of function of the esophagus and stomach, the presence and degree of gastroesophageal reflux.
How is a hernia treated at the CELT clinic?
At the initial stage, conservative methods of hernia treatment are used. The clinic of concomitant diseases of the gastrointestinal tract comes to the fore, so therapy is aimed at eliminating them. The clinic’s gastroenterologists will select an individual treatment regimen that includes a basic list of drug groups:
- antacids;
- proton pump inhibitors;
- H2-histamine receptor blockers;
- drugs that improve motor skills (prokinetics);
- B vitamins.
Indications for surgical removal of the hiatal hernia:
- Fixed large hiatal hernia.
- Long-term and ineffective conservative therapy.
- Development of complications of the disease.
- Precancerous condition of the mucous membranes (so-called dysplastic changes).
In our clinic, preference is given to low-traumatic surgical interventions - laparoscopic operations, which allow access to internal organs through small punctures in the skin measuring 0.5-1 cm. To avoid relapses, surgeons always install a mesh implant.
There are main groups of surgical interventions:
- Crurorrhaphy (suturing the hernial opening and strengthening the ligamentous apparatus).
- Gastropexy (attachment of the stomach to the abdominal wall).
- Fundoplication (surgery restores the normal relationship of the fundus of the stomach with the lower part of the esophagus).
- Partial removal of the esophagus (performed in the presence of a scar stricture).
Specialists will give all the necessary recommendations and describe in detail the principles of diet therapy and proper lifestyle. Thus, people suffering from hiatal hernia should eat no later than 3 hours before bedtime, sleep with the head elevated, normalize weight, and avoid overeating and heavy lifting. After surgery, patients must be observed by a gastroenterologist. Relapses of the disease are extremely rare.
The success of treatment for hiatal hernia depends on the level of qualifications and experience of doctors, as well as (to a large extent!) on the patient’s compliance with all the doctor’s recommendations. Rest assured that at the CELT clinic you will receive decent attention and high-quality medical services.
Hiatal hernia: what to do if you are diagnosed with this?
This disease is distinguished by the fact that it is difficult to diagnose in the early stages. What are the symptoms of the pathology? How is it treated and how can it be avoided?
We talk about hiatal hernia with Yulia Gennadievna Aichkina, a gastroenterologist at Clinic Expert Voronezh.
— Yulia Gennadievna, what is a hiatal hernia?
- This is a condition (abbreviated as hiatal hernia) caused by the displacement of abdominal organs into the mediastinum through the esophageal opening of the diaphragm. Such a hernia is one of the risk factors for the development of gastroesophageal reflux disease - this pathology is accompanied by inflammation of the mucous membrane of the esophagus.
— How common is a hiatal hernia?
— If we talk about diseases of the digestive system, it is believed that the hiatal hernia is one of the first places. Although this is a subjective assessment, since often the disease can occur without obvious symptoms. According to some data, in Russia this pathology is observed in 5-35% of residents, and in older people - up to 50%.
— What are the causes of hiatal hernia?
— Congenital hernias can appear due to uneven development of the muscles and openings of the diaphragm, incomplete descent of the stomach into the abdominal cavity, weakness of the connective tissue in the esophageal opening of the diaphragm. However, in most cases, acquired types of hiatal hernia occur. This is facilitated by the combined influence of various factors, one of the main ones being weakness of connective tissue structures and atrophy of muscle fibers.
The development of a hernia can be associated with heavy lifting, constipation, excess weight, and in women - with pregnancy. Chronic cough and frequent vomiting also contribute to the appearance of hiatal hernia. That is, we are talking about factors that increase intra-abdominal pressure.
Read materials on the topic:
Constipation in adults: looking for causes and getting rid of it. What does fat have to do with it or why do people gain weight?
— What do the symptoms of a hiatal hernia look like?
— Its small size, as a rule, rarely causes any serious problems. When a hiatal hernia occurs, a person begins to experience pain as soon as it gets larger. The patient complains of unpleasant sensations such as heartburn, belching with a sour or bitter taste, pain and difficulty swallowing food, heaviness in the stomach, pain in the chest, which can be taken as signs of angina pectoris or myocardial infarction. These symptoms intensify after eating and physical activity. A hiatal hernia also makes itself felt by pain when coughing and flatulence. The pain may ease or disappear if the person changes body position. He feels better after burping, taking a deep breath, or vomiting. But when bending forward, the pain may intensify.
Another manifestation of the disease may be dysphagia - difficulty passing food through the esophagus. This is especially noticeable when a person eats hastily, “on the go,” when the food is liquid or semi-liquid, or if you swallow too cold or too hot water.
— How is a hiatal hernia diagnosed?
— Often the disease develops asymptomatically and is detected accidentally during an X-ray examination of the esophagus or stomach, or during an endoscopic examination (esophagoscopy, gastroscopy). An ECG (to exclude cardiac pathology) is required, and less often - a CT scan of the chest and mediastinum. In the most difficult cases, diagnostic laparoscopy is performed.
Read materials on the topic:
X-ray of the stomach: an eternal classic or a step back? Where can I find the courage to make up my mind? Gastroscopy - WITHOUT fear! What does an electrocardiogram reveal?
— What is the treatment for hiatal hernia?
- If there are no manifestations of the disease, it is not required. It is important to avoid obesity, since excess weight increases intra-abdominal pressure. If symptoms of the disease occur, a therapist or gastroenterologist may prescribe conservative drug treatment aimed at preventing gastroesophageal reflux (the so-called reverse movement of stomach contents into the esophagus). In this case, agents are used that suppress the production of hydrochloric acid in the stomach, reduce the acidity of already formed gastric juice, and normalize the contractile function of the stomach.
For large hernias, ulcers in the esophagus and ineffective therapy, the patient is recommended to undergo surgery, which is performed laparoscopically. Surgical treatment consists of lowering the stomach into the abdominal cavity and restoring the hole in the diaphragm using various techniques.
— Is it possible to treat a hiatal hernia with folk remedies?
- Definitely not.
— Are there any special dietary requirements for hiatal hernia?
— Firstly, it is recommended to eat leisurely, not on the run, without overeating, because in this case a person inevitably swallows large portions of air along with food, and this increases intragastric pressure. It is better to eat your last meal in the evening no later than 3 hours before bedtime. You should limit yourself in consuming foods such as fatty meat, lard, and do not get carried away with pasta, noodles, bakery products, butter cookies and pastries. You will also have to be careful with spicy seasonings, fried foods, carbonated drinks, and alcohol.
— How to prevent the development of a hiatal hernia?
- If we cannot change heredity, then we can eliminate the situations that cause an increase in intra-abdominal pressure. To do this you should:
- normalize weight;
- be careful when lifting weights;
- eliminate constipation;
- treat diseases accompanied by chronic cough;
- quit smoking and alcohol;
- follow the rules of healthy eating.
You can make an appointment with a gastroenterologist here. ATTENTION: the service is not available in all cities
Interviewed by Igor Chichinov
The editors recommend:
What to do if you suffer from heartburn? How to and how NOT to treat gastritis How to protect the stomach from ulcers? Living in acid: what do we know about Helicobacter pylori How to avoid becoming a balloon? Getting rid of gas formation in the intestines
For reference
Aichkina Yulia Gennadevna
In 2015 she graduated from Voronezh State Medical University. N.N. Burdenko.
In 2022, she completed residency in the specialty “General Medical Practice” and primary retraining in gastroenterology.
He holds appointments as a gastroenterologist at the Expert Clinic Voronezh at the address: st. Pushkinskaya, 11.
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Appointment with a gastroenterologist (primary) | 4 200 |
| Fluoroscopy and radiography of the esophagus | 2 600 |
| Gastroscopy (videoesophagogastroduodenoscopy) | 6 000 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions