Gastroenterologist
Neronov
Vladimir Alexandrovich
24 years of experience
Gastroenterologist, Doctor of Medical Sciences
Make an appointment
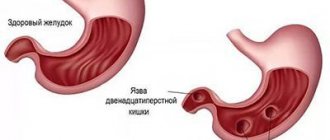
Duodenitis is an inflammatory process that develops in the mucous membrane of the duodenum. Damage to the upper parts of the organ causes symptoms that are mistakenly taken by patients for manifestations of gastric ulcer. Inflammation in the lower intestine is similar to acute pancreatitis or cholecystitis. The pathology causes attacks of nausea and vomiting, heartburn, belching, and intense stomach pain. The acute stage of the disease lasts several days. Children and adults are prescribed a gentle diet and drug treatment. Relapses provoke the transition of duodenitis to the chronic stage with the spread of the inflammatory process to the pyloric part of the stomach. If left untreated, severe complications develop: intestinal perforation, acute pancreatitis, intestinal bleeding.
General information
The disease can occur in acute or chronic form. In the first case, drug therapy eliminates the symptoms of the disease and prevents structural changes in the mucous membrane of the duodenum. The chronic type of inflammation is characterized by regular relapses and changes in the structure of the intestinal epithelium. The disease remains the most common pathology of the duodenum. Up to 95% of clinically diagnosed cases of acute duodenitis resulted in the transition of the pathology to the chronic stage. Men suffer from inflammation of the mucous membranes of the duodenum twice as often as women.
Reasons for development
Gastroenterologists consider the inflammatory process as a multifactorial phenomenon. The causes of primary duodenitis are foods that irritate the mucous membranes of the gastrointestinal tract - dishes with a lot of spices and salt, drinks with a high ethanol content, strong varieties of tea and coffee. The secondary form of pathology develops against the background of other diseases from which the patient suffers - duodenal ulcer, impaired blood supply to the intestine, infection with the bacterium Helicobacter Pylori. Inflammation of the duodenal mucosa can result from colitis, hepatitis, liver cirrhosis or pancreatitis.
Diagnosis of bulbits
The main methods used in diagnosing bulbitis are as follows:
- Gastroduodenoscopy is the most informative method that helps to determine or exclude the disease. This endoscopic procedure determines whether there are inflammatory processes on the mucous membrane, whether erosions, duodenal ulcers, or duodeno-gastric reflux have developed. The study is carried out on an empty stomach with possible preliminary sedation of the patient (under anesthesia, which allows you to forget about some discomfort associated with this procedure).
- A study of biopsy material or a urease breath test helps determine the presence of Helicobacter infection, which very often causes a recurrent inflammatory process.
- X-ray examinations (performed less frequently).
When contacting a clinic for diagnostics, you must remember that most of the proposed procedures are performed on an empty stomach. A preliminary consultation with a gastroenterologist will allow you to properly prepare for the tests, which will significantly increase their information content.
Etiology
A focus of inflammation in the duodenum is formed due to damage to epithelial cells by hyperacid juice coming from the stomach. The increased acidity of this compound irritates the intestinal mucous membranes. In the absence of pronounced symptoms, the pathology proceeds unnoticed by the patient and quickly progresses to the chronic stage. Degenerative processes develop in the intestinal wall (leading to the formation of foci of atrophic duodenitis).
Pathology of the secondary type occurs due to functional digestive disorders provoked by the primary disease. Chronic damage to the liver, gallbladder and pancreas leads to changes in the enzyme balance. As a result of these changes, the protective properties of the epithelium of the duodenum are weakened - a focus of inflammation is formed.
Symptoms of the disease
The clinical picture of duodenitis directly depends on the form of the pathological process. Duodenitis, which often occurs in combination with a gastric ulcer, is accompanied by intense pain in the epigastric (epigastric) region, worsening on an empty stomach or at night. If the disease occurs in combination with enteritis, then intestinal symptoms predominate in the clinic.
The process of absorption of beneficial components from food is disrupted, and digestive disorders appear, including diarrhea. If the passage of the food bolus in the lumen of the organ slows down or completely stops, then the following symptoms of gastric duodenitis :
- severe pain syndrome, with the pain being paroxysmal;
- pain in the epigastric region;
- feeling of abdominal distension, bloating;
- nausea and attacks of vomiting, while the vomit contains bile impurities;
- belching with a bitter taste.
If the duodenum is affected locally, then the symptoms of biliary dyskinesia predominate. The pain can spread to the left or right hypochondrium, and also have a girdling character. External signs include yellowing of the skin and eye sclera, itchy skin, light-colored stool and darkening of urine.
Symptoms
Symptoms of duodenitis depend on the clinical form of the disease found in the patient. An ulcer-like type of inflammation provokes the development of acute pain in the epigastrium - the area located above the navel. After eating, the condition of the child or adult improves. The gastro-like form of the pathology leads to heartburn and belching. Pain in the epigastric region appears 20 minutes after consuming hot foods or drinks. Associated symptoms include attacks of nausea and vomiting. Patients often note a decrease in appetite and excessive accumulation of gases in the intestines. The pancreatic-like type of disease is characterized by acute pain in the right or left hypochondrium. Over time, dyspeptic disorder develops. The mixed form of the pathology has a variety of symptoms, which depend on the frequency of the patient’s meals and the presence of chronic diseases of the gastrointestinal tract.
Inflammation of the duodenum: symptoms and treatment
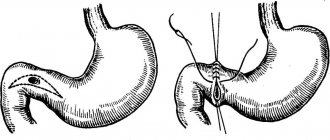
Duodenitis is an inflammation of the mucous membrane of the duodenum and its gradual structural restructuring. With the development of a single lesion of the duodenal bulb, bulbitis develops; if pathological changes occur in the area of the papilla of Vater (large duodenal papilla), the disease is called sphincteritis or odditis. Duodenitis can be an independent pathology, but more often it is combined with other pathological processes in the gastrointestinal tract. Often inflammation spreads not only to the intestines, but also to the stomach, resulting in gastroduodenitis.
The reasons for the development of this pathology are often hidden in a person’s lifestyle. Rough food, irregular nutrition, smoking, drinking alcohol, frequent psycho-emotional stress and nervous tension - all this leads to the launch of processes, as a result of which inflammation develops. Duodenitis also develops and progresses against the background of gastric ulcer, duodenal diverticulosis, diseases of the liver and biliary tract, and pancreatitis.
Pathological factors include: an increase in the content of pepsin and hydrochloric acid in gastric juice, an insufficient amount of secretin (the process of neutralization of hydrochloric acid worsens), an increase in the delay in the evacuation of duodenal contents.
There are acute, chronic and phlegmonous duodenitis.
The clinical picture of acute inflammation of the duodenum is characterized by: epigastric pain, a feeling of fullness, nausea, vomiting, and drooling. There may be a decrease in appetite and an increase in body temperature. Even more rare, but possible clinical manifestations: arterial hypotension, headache. Often the patient feels general weakness.
A diagnosis is made based on the clinic and diagnostics performed. Duodenal intubation reveals mucus and desquamated epithelium during duodenoscopy, and inflammatory changes in the mucosa during gastroscopy. Differential diagnosis with diseases of the digestive system, in particular gastritis, is mandatory.
For inflammation of the duodenum, treatment is conservative. Depending on the severity of the condition and the severity of symptoms, therapy is carried out on an outpatient or inpatient basis. For increasing pain, antispasmodics and analgesics are used. Anti-inflammatory, reparative and enveloping drugs are prescribed. Diet therapy is required.
Chronic duodenitis is quite diverse in its clinical manifestations. To facilitate the diagnostic task, several forms are distinguished:
- Ulcer-like. This form is characterized by pain reminiscent of a peptic ulcer, but of less intensity and not associated with seasonality.
- The gastritis-like form is distinguished by the clinical appearance of dyspeptic disorders. Vomiting, diarrhea, and bloating are frequent accompaniments of this form.
- Pancreatitis- or cholecystitis-like forms are characterized by nagging pain in the right hypochondrium, girdle pain. Manifestations intensify after eating fatty foods.
- The neurovegetative form is more common in young women and is accompanied by a general somatic clinical picture. Increased fatigue, irritability, general weakness, headaches often lead the patient to neurologists and psychotherapists, and the inflammatory process of the digestive tract is overlooked.
- The mixed form is characterized by a combination of various clinical manifestations of all of the above forms.
- The asymptomatic form does not manifest itself in any way, except for increasing general weakness. More common in older people.
As a result, chronic duodenitis can become erosive, which often leads to the development of hidden gastrointestinal bleeding and anemia. In this case, general weakness, dizziness, melena, and decreased blood pressure appear, sometimes to the point of collapse.
The diagnosis of chronic inflammation of the duodenum and accompanying symptoms determine treatment. Diet therapy is mandatory. Salted, fried, smoked, fatty foods are excluded - everything that can have an irritating and carcinogenic effect on the gastrointestinal mucosa. In drug therapy, antacids are more often used to protect against the secretory activity of the stomach and reparants. All other therapy is carried out taking into account the form of chronic duodenitis. Phlegmonous duodenitis is a form that requires mandatory hospitalization in a gastroenterological hospital. Primary phlegmonous duodenitis develops when bacterial flora penetrates through the mucous membrane into the deep layers and extensive ulcerative defects. Secondary phlegmonous duodenitis occurs when bacterial flora is introduced hematogenously from other foci (abscesses of various locations, boils, gangrene).
The clinical picture is quite bright, characterized by a hectic temperature reaction and chills. Often there is excruciating pain in the upper abdomen, often on the right. Against the background of general intoxication, general weakness, headache, and a feeling of aching throughout the body develop. A clinical picture of an “acute” abdomen appears: a board-shaped abdomen, a dry brush-like tongue, a positive Shchetkin-Blumberg sign. A frequent complication of phlegmonous duodenitis is peritonitis, diaphragmatic abscess, mediastinitis, purulent pleurisy, sepsis. To prevent the development of complications, the patient needs urgent surgical treatment, which is the main thing for this form.
The diagnosis of inflammation of the duodenum (duodenitis) is made based on clinical manifestations, history and diagnosis. One of the main research methods is gastroscopy with biopsy.
Gastroscopy refers to endoscopic research methods. Thanks to this procedure, it is possible to visualize the mucous membrane of the digestive tract and detect defects. The manipulation is carried out using a gastroscope equipped with a fiber-optic system and forceps. This device is a flexible tube inserted through the mouth and esophagus into the stomach. The optical system produces a fairly bright, detailed image that is displayed on the screen. If necessary, photographs are taken and attached to the patient's medical record. Gastroscopy helps to examine all visible defects of the mucous membrane and take samples from suspicious formations for biopsy, followed by histological and cytological examination. The examination is carried out in a gastroentorological hospital by a specially trained endoscopist. The interpretation and conclusion are given by the same doctor. If a pathology is detected, the attending physician, based on the clinic and endoscopic data, makes a diagnosis and prescribes adequate drug therapy. A type of gastroscopy is FEGDS (fibroesophagogastroduodenoscopy), which allows you to visualize the mucous membrane of not only the esophagus and stomach, but also the duodenum.
Diagnostic measures
Diagnosis of duodenitis is carried out during gastroscopy - immersion of an endoscopic probe into the patient’s stomach and intestines. Additional ways to confirm the diagnosis are:
- X-ray examination of the gastrointestinal tract;
- biochemical analysis of gastric juice;
- duodenal intubation;
- general clinical and biochemical blood tests;
- coprogram.
If signs of malignant degeneration of duodenal tissue are detected, the doctor takes a biopsy - biomaterial that is subjected to histological examination in the laboratory.
Therapeutic course
Treatment of duodenitis is carried out under the supervision of a gastroenterologist. The patient is prescribed a strict diet: foods that are difficult to digest (milk, cereals) and dishes with spices are excluded from the diet. Drug therapy is based on drugs that suppress excessive secretion of hydrochloric acid in the stomach. Normalization of digestion is carried out by taking enzyme agents by a child or adult. Protecting the walls of the duodenum from irritation requires the use of gastroprotectors - drugs that coat the mucous membranes of the gastrointestinal tract.
In case of a complicated course of the disease, the gastroenterologist may insist on surgical intervention. Surgeons will eliminate intestinal obstruction and remove adhesions formed due to secondary duodenitis. In such cases, treatment requires hospitalization of the patient.
Treatment of duodenitis
First of all, it is necessary to normalize your diet. As a rule, a therapeutic diet is prescribed (table No. 1 in the acute stage and No. 5 in the chronic stage).
In acute cases of the disease, it is allowed to consume weak tea, cocoa, low-fat cottage cheese, eggs, oatmeal and semolina porridge, and pureed soups. Prohibited: mushrooms, peppers, sweets, coffee, fatty meat and fish, buns. During chronic exacerbation, vegetable soups, bread, lean meats (beef, chicken), and non-acidic fruits are allowed. The same things are prohibited as in the acute stage. During the period of remission, you can eat any food, but in moderation. Preference should be given to a healthy and proper diet and not to overeat.
Medicines are prescribed depending on the cause of the disease.
- Antibiotic therapy for Helicobacter Pylori infection
- Medicines to reduce acid production in the stomach.
- Preparations with an enveloping effect.
- Anti-inflammatory drugs.
- Pancreatic enzymes.
- Medicines aimed at restoring the mucous membrane (cytoprotectors).
- Antispasmodic drugs.
- If helminths are present, take medications to get rid of them.
- With high psycho-emotional stress, sedatives may be prescribed.
Attention! All medications are prescribed only by a doctor based on an analysis of the medical history, examination and research. Self-medication is unacceptable. Information about medications is given for informational purposes only.
Preventive measures
The basis for the prevention of gastrointestinal diseases is a balanced diet. Doctors recommend that patients stop smoking and drinking alcohol. Reducing the risk of developing inflammatory processes in the duodenum is facilitated by timely treatment of pathologies of the digestive system.
In the chronic course of the disease, a child or adult will need to regularly undergo clinical examinations and take medications that help eliminate the cause of inflammation of the intestinal epithelium. In this case, a favorable prognosis is formed - the patient’s quality of life remains at a consistently high level.