- Treatment of the stomach and 12 intestines
- Nutrition for pathology
- Preventive actions
- Advantages of online registration at the International Center for Health Protection
The intestine is an organ of the digestive system, consisting of several sections. None of them are immune from inflammatory processes. Pathology occurring in the upper segment is called inflammation of the duodenum. This is an intermediate section located between the stomach and small intestine. Due to the peculiarities of being in the human body, it is subject to a double risk of infection: ascending with the contents of the stomach and descending from the lower intestinal sections.
The disease also has another name – duodenitis. As a separate pathology, it is rare. Symptoms of inflammation of the duodenum usually occur against the background of other gastrointestinal diseases. The incidence of dysfunction has no connection with the gender or age of the patient. It occurs equally in different groups of subjects.
Symptoms of the disease
Symptoms of duodenal inflammation can vary. They are determined by the clinical form of the disease. In most cases, the following deviations are recorded:
- Pain. Unpleasant sensations and discomfort are localized in the epigastric region. It is possible that they spread to the right hypochondrium.
- Intoxication syndrome. Infectious toxicosis causes weakness, excessive fatigue, and fever.
- Disruption of the normal functioning of the stomach. In combination with gastritis, there are manifestations of heartburn, nausea, and in rare cases, vomiting.
- Digestive disorders. Recorded when the patient has colitis or enteritis. Expressed in diarrhea, bloating, constipation, constant but mild pain in the entire abdomen.
With duodenostasis - a violation of the patency of the duodenum - the clinical manifestations are pronounced:
- bloating, rumbling;
- sharp pain in the upper abdomen, forcing a person to take a special position;
- nausea and vomiting bitterness.
Local forms of inflammation of the duodenum affect the common bile duct, which makes it possible to clearly visualize the symptoms of biliary colic or biliary dyskinesia.
If the patient is diagnosed with anemia, it may indicate internal bleeding.
Causes of the disease
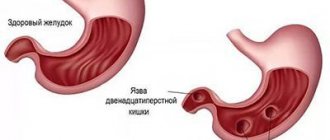
Inflammation of the duodenum is divided into primary and secondary. Primary damage to the mucous membrane of the digestive organs is associated with a violation of the level of acidity. Damage to the walls of the stomach and duodenum is the result of exposure to an aggressive gastric environment. This happens due to the fact that the patient did not eat properly for a long time: he ate a lot of salty, fatty and fried foods, and preferred to eat dry food. The natural defense of the mucous layer in such situations is weakened, which is why the body is unable to neutralize the harmful effects of hydrochloric acid.
A secondary disease occurs against the background of other malfunctions in the body:
- gastritis caused by Helicobacter pylori bacteria;
- peptic ulcer with high acidity;
- cholecystitis and pancreatitis, due to which duodenostasis gradually develops;
- liver dysfunction – hepatitis, cirrhosis;
- toxic infection, food poisoning;
- burn of the mucous membrane due to chemicals entering the digestive tract;
- foreign body in the abdominal organs.
Depression, stress, mental problems, alcohol abuse and smoking can also trigger the development of pathology. The risk group also includes those who take non-steroidal anti-inflammatory drugs and cytostatics.
Stages of duodenal cancer
In the overwhelming majority, mucous adenocarcinoma develops in the duodenal wall; anatomical features make it possible to diagnose it in the early stages.
Staging is based on the degree of involvement of the intestinal wall in the malignant process and the presence of metastases in the lymphatic collector:
- Tumor within the mucous membrane - stage 1;
- Neoplasm within the wall with metastasis to the lymph nodes near the organ - stage 2;
- Cancer of the intestinal wall grows into the abdominal cavity and involves nearby anatomical structures - stage 3;
- With any size of tumor lesion of the duodenal wall, the appearance of metastases in other organs - stage 4 is unconditionally established.
Diagnosis of pathology
If you have problems with the duodenum, you need to visit a gastroenterologist. He will palpate your abdomen. The occurrence of pain in the epigastric zone indicates duodenitis. Accurate diagnosis is possible after examination. EGD or esophagogastroduodenoscopy is considered the most informative. A gastric tube with a camera attached is inserted into the patient. The device allows you to examine the entire gastrointestinal tract and identify abnormalities, see the intestinal mucosa, detect the localization of inflamed areas and bleeding. If necessary, an endoscopist can take a piece of stomach tissue for histology.
Additional examinations include ultrasound, x-ray, test for the presence of Helicobacter pylori bacteria, blood and stool tests, and measurement of gastric acidity. A coprogram, a three-time examination of stool for occult blood, and blood biochemistry may also be needed.
Features of the structure of the organ
The anatomical structure of the stomach includes four main parts:
- cardiac section (divided into supracardial and subcardial sections) - located near the esophagus, this is where the food mass enters the stomach;
- The pyloric region, also called the pyloric region, is located at the entrance to the duodenum. From it, the food bolus enters the duodenal bulb for further processing, and then into the postbulbar section and further along the intestine;
- body (fundus) - the part between the cardiac and pyloric sections;
- the bottom is the most elevated part of the organ, located in the upper right part above the cardiac section.
The mucous membrane gets its name from the thick layer of mucus that protects the surface of the stomach from the effects of gastric juice and self-digestion.
The structure of the gastric mucosa differs depending on the section. Based on this feature, only three sections are distinguished, since the bottom and body have a similar mucosal structure.
The mucous membrane contains glands that secrete gastric juice. The enzymes in its composition break down proteins and participate in the primary breakdown of fats.
The muscular layer of the stomach walls is involved in grinding food into a liquid pulp, chyme, which enters the intestines in small portions, passing through all sections.
The human stomach takes different times to digest different foods. Most quickly, in about 20 minutes, the stomach copes with fruit juices and broths; it takes up to six hours to digest meat.
Each section of the stomach has different glands, of which there are at least 15 million. The cardiac glands are tubular in shape and very similar to the glands of the adjacent esophagus.
The largest number of glands are located in the mucous membrane of the body and fundus of the stomach. They consist of different types of cells: chief, parietal, mucous cervical and accessory, as well as endocrine.
Classification of duodenitis
Inflammation of the duodenum is divided into various types depending on the location, the causative agent of the pathology, and the nature of the course of the disease. The classification of this dysfunction looks like this:
1. For reasons and conditions of occurrence:
- acute duodenitis – characterized by a sudden onset, pronounced symptoms, and a short course; possible catarrhal, ulcerative, phlegmonous forms;
- chronic inflammation - can last for several years with mild symptoms.
2. According to the localization of inflammatory foci:
- diffuse (widespread) duodenitis - the entire duodenum is inflamed;
- local: popilit - inflammation of the major papilla, bulbitis - damage to the bulb, postbulbar duodenitis - damage to the distal part.
3. According to the degree of damage to the mucous membrane:
- superficial – the pathology is considered to be the most “peaceful”, since the inflammatory process affects only the upper layers of the mucosa;
- interstitial - the mucous membrane suffers more, this type of disorder is characterized by penetration into the deep layers;
- atrophic – in the damaged area there is thinning or absence of the mucous membrane at all;
- erosive - leads to the appearance of ulcers and erosions of the intestinal walls, can cause the development of stomach and duodenal ulcers.
Specific duodenitis is classified into a special category. They appear against the background of tuberculosis, fungal infection, immunodeficiency, Crohn's disease.
Duodenal diverticulum simulating a pancreatic cyst
Ultrasound scanner HS70
Accurate and confident diagnosis.
Multifunctional ultrasound system for conducting studies with expert diagnostic accuracy.
Introduction
A diverticulum (from Latin diverto, divertere - to fold, to direct in the other direction) is a protrusion of the wall of a hollow organ that communicates with its lumen. There are true and false diverticula, the former are rare, mostly congenital, single. Their wall has the same structure as a hollow organ (hence the name). Having a muscle layer, true diverticula are able to actively empty themselves, and their inflammation rarely occurs [2]. False diverticula are relatively common and represent a protrusion of the mucous membrane between the muscle fibers; their wall does not contain a muscle layer and they cannot actively empty themselves. This favors stagnation of contents and the development of diverticulitis.
Diverticula occur in weak areas of the wall, most often in tunnels formed by vessels that penetrate the muscle layer. Proximity to blood vessels creates a high risk of bleeding [4, 7]. That is why the clinical significance of the disease lies in the possibility of developing complications, including life-threatening ones [2].
In the diagnosis of diverticula of the digestive tract (they can occur in any hollow organ, but, as statistics show, they are more common in the colon), the leading place is occupied by the x-ray method, since endoscopic examination is noticeably inferior in accuracy. Thus, esophagogastroduodenoscopy (EGDS) detects a disease, for example in the duodenum, in only 1/3 of the patients for whom the diagnosis is established radiologically. For the stomach this figure is even lower [4].
In recent years, quite a lot of experience has been accumulated in ultrasound diagnostics of pathological conditions and diseases of the gastrointestinal tract [1, 3, 5, 6]. However, in the available literature we have not encountered a single case of successful ultrasound diagnosis of diverticula of the stomach or duodenum.
In this report we would like to share an observation that confirmed the possibility of echographic diagnosis of duodenal diverticulum.
Case description
Patient A., 66 years old, complained of short-term, periodically occurring aching pain in the epigastrium and right hypochondrium, not associated with food intake, a feeling of bitterness in the mouth, belching of air and food, heartburn, and nausea. From the anamnesis it is known that in 1982 a cholecystectomy was performed for cholelithiasis. Subsequently, I felt well, was not examined, and was not treated. The complaints described above have been bothering me for the last 4-5 weeks, and therefore I went to the doctor at the clinic at my place of residence, where an ultrasound of the abdominal organs revealed a pancreatic cyst.
Upon presentation: satisfactory condition, increased nutrition, skin and visible mucous membranes are clean, normal color. No abnormalities were detected from the cardiovascular system or lungs. Pulse 79 beats. in 1 minute, rhythmic, good filling. Blood pressure = 135/90 mm Hg. Art. The tongue is moist and covered with a gray coating. The abdomen is soft, moderately painful on palpation in the epigastrium. The liver is not enlarged and not palpable. Stool with tendency to constipation. There is no dysuria. Clinical and biochemical blood tests revealed no diagnostically significant deviations from the norm.
Ultrasound of the abdominal organs: the liver is not enlarged in size (4.3-13.3 cm), its contour is smooth, the parenchyma has moderately pronounced signs of fatty infiltration. No focal pathology was identified. The intrahepatic bile ducts and veins, portal (0.9 cm) and splenic (0.4 cm) veins are not dilated. The common bile duct is visualized in fragments, the diameter does not exceed 0.8 cm. The gallbladder is not visualized (surgically removed). The pancreas is of normal size (2.9-1.6-2.1 cm), the contour is smooth, evenly diffusely compacted. The duct of Wirsung is not dilated. The cross-sectional diameter of the digestive tract at the level of the esophageal opening of the diaphragm is 1.6 cm. There is a lot of mucus in the stomach on an empty stomach, its wall is not thickened (0.3-0.5 cm). At the level of the outer contour of the head of the pancreas, a rounded formation with smooth contours of reduced echogenicity is visualized with a delicate internal structure measuring 2.1 × 3.2 cm (Fig. 1). Polypositional examination failed to reveal the connection of this formation with the head of the gland. At the same time, locally, at the level of this formation, the thickness of the wall of the distal part of the duodenal bulb was 0.5 cm (in other parts 0.2-0.3 cm). The spleen is not enlarged, its structure is homogeneous. Free fluid in the abdominal cavity is not detected. The abdominal aorta is of normal diameter (1.8 cm). Para-aortic lymph nodes are not visualized. Conclusion: condition after cholecystectomy. Ultrasound signs of liver steatosis, hiatal hernia. Pancreatic head cyst? To exclude pathology of the stomach and duodenum, X-ray and endoscopic examinations are indicated.
Rice. 1.
Echogram of a duodenal diverticulum simulating a pancreatic cyst.
X-ray of the stomach and duodenum: the act of swallowing is not impaired. The esophagus is freely passable; there is a significant size (up to 7 cm) hiatal hernia with severe reflux esophagitis and reflux of stomach contents into the distal esophagus, increasing in size when lying on the stomach. The stomach is usually located and contains mucus and fluid on an empty stomach. The folds of the mucous membrane are thickened, convoluted, and form serration along the posterior wall and greater curvature in the cardiac region. The pylorus is freely passable; prolapse of the gastric mucosa into the duodenal bulb is noted. In the descending branch of the duodenal loop, a pedunculated diverticulum measuring 3 cm with a large amount of mucus in it is detected (Fig. 2). The duodenal bulb is irritated, the barium suspension passes through it very quickly, and a reverse reflux of the barium mass into the stomach is noted. Conclusion: sliding hernia UNDER. Reflux esophagitis. Gastritis. Duodenitis. Duodenogastric reflux. Diverticulum of the duodenal loop with signs of diverticulitis. The patient categorically refused to undergo EGD.
Rice. 2.
X-ray of a duodenal loop diverticulum.
Conclusion
The duodenum is the most common location of small intestinal diverticula, which in 98% of cases are located on the inner wall of the duodenum, where they are embedded in the pancreatic tissue, and only in 2% - on the free outer wall [4]. Most often, diverticula are localized in the area of the major duodenal papilla; people over 40 years of age prevail. In approximately 30% of patients, duodenal diverticula are combined with other diseases: peptic ulcer, gastric polyposis, cholelithiasis, pancreatitis, colon diverticulosis. If patient conservative treatment does not produce the desired results, surgery is indicated.
The case under consideration is interesting in that a large duodenal diverticulum simulated a pancreatic cyst during ultrasound examination. Cysts (pseudocysts) of the pancreas are much more common than diverticula, so it is quite natural to conclude that the patient has a cyst. However, the absence of indications in the anamnesis for acute or chronic pancreatitis, an unsuccessful attempt to trace the connection of the identified fluid formation with the head of the pancreas during polypositional examination, and local thickening of the duodenal wall allowed us to suggest a possible other pathology and prescribe further examination.
Thus, when identifying a volumetric fluid formation of the pancreas (in the projection of the gland) during echography, it is necessary to include the pathology of the stomach and duodenum in the differential diagnostic search algorithm, not forgetting about diverticula, since, as S.V. rightly notes. Herman, “The key to early diagnosis of digestive tract diverticula is a high index of suspicion of the disease” [2].
Literature
- Burkov S.G. Ultrasound diagnosis of diseases of the gastrointestinal tract // Doctor. - 1997. - N 1. - P. 16-18.
- German S.V. Diverticular disease of the colon: myths and reality // Ros. and. Gastroenterology, hepatology, coloproctology. - 2000. - N 1. - P. 66-75.
- Clinical guide to ultrasound diagnostics / Ed. V.V. Mitkova. IV volume. - M.: Vidar, 1997. - 388 p.
- Krylov A.A., Zemlyanoy A.G., Mikhailovich V.A., Ivanov A.I. Emergency gastroenterology. Guide for doctors. - St. Petersburg: "Peter", 1997. - P. 139-164.
- Berstad A., Hausken T., Gilja OH Ultrasonography of the human stomach // Scand. J. Gastroent, 1996. - Vol. 220. Suppl. pp. 75-82.
- Gimondo P., Mirk P., Romano M., Jannetti G., Gallipoli A. Ecographia e tratto gastroenterico: Stato dell`arte // Giornale Italiano Di Ecografia. 2000. - Vol. 3.- N 2. S. 121-129.
- Telford GL, Appel D. Diverticulitis // Gastrointestinal emergencies / Ed. M. B. Taylor. 1997. - P. 571-576.
Ultrasound scanner HS70
Accurate and confident diagnosis.
Multifunctional ultrasound system for conducting studies with expert diagnostic accuracy.
Treatment of the stomach and 12 intestines
For the treatment of the duodenum, drug treatment is mainly used. Diet is also of great importance. In case of acute inflammation or exacerbation of chronic pathology, symptomatic therapy is prescribed:
- antacids - medications that neutralize hydrochloric acid, thereby reducing the acidity of gastric juice;
- antispasmodics – medications that relieve spasms and pain and alleviate the patient’s condition;
- enveloping compounds - protect surface tissues and the endings of sensory nerves without interacting with proteins or cellular structures;
- antibiotics - when Helicobacter bacteria are detected, they are selected depending on what caused the deviation and at what stage it is;
- medicines to get rid of parasites - if the cause of the disease, such as helminthic infestation, has been established;
- medications that improve intestinal motility - if the patient is diagnosed with duodenostasis.
Treatment of chronic duodenum requires the following medications:
- anticholinergics, the action of which is aimed at reducing pain and discomfort;
- antacids and enterosorbents that protect the mucous membrane from the negative effects of external factors;
- anti-inflammatory, healing medications that enhance tissue regeneration, preventing the progression of the pathological process;
- dopamine blockers, which help get rid of nausea and vomiting in case of problems with motor function of the duodenum;
- sedatives that help cope with the manifestations of neurasthenia, often a concomitant disease.
Successful treatment of secondary pathology is impossible without getting rid of the main deviation. The rarest form - phlegmosis, which is an acute purulent-destructive process - is treated through surgery with further antibiotic therapy. Physiotherapeutic procedures are auxiliary, which are carried out during periods when the disease does not worsen. These measures include warming up the epigastric area, ultrasound, balneotherapy, paraffin-ozokerite applications, and magnetic therapy.
Structure of the small intestinal wall
On a section, the intestinal wall consists of 4 membranes of different histological structure (from the lumen outward):
- Mucous;
- Submucosa;
- Muscular;
- Serous.
Mucous membrane
The mucous membrane of the small intestine has circular folds protruding into the lumen of the intestinal tube, with villi and intestinal glands. The functional unit of the intestine is the villus, which is a finger-shaped outgrowth of the mucous membrane with a small area of submucosa. Their number and size are different in different segments of the intestine: in 12 PCs - up to 40 units per 1 square millimeter and up to 0.2 mm in height. And in the ileum, the number of villi decreases to 20-30 per 1 square millimeter, and the height increases to 1.5 mm.
In the mucous membrane, under a microscope, a number of cellular structures can be distinguished: border, stem, goblet, enteroendocrine cells, Paneth cells and other macrophage cellular elements. Border cells (enterocytes) have a brush border (microvilli), at the level of which parietal digestion occurs and due to the number of villi of which the surface of contact of food with the area of the inner lining of the intestine increases 20 times. Also, the presence of folds and fibers contributes to a 600-fold increase in the overall suction surface. In total, the working area of the intestine is up to 17 square meters in an adult.
At the level of the border cells, proteins, fats and carbohydrates are broken down into their simplest components. Goblet cells produce a mucous secretion to facilitate the movement of food chyme through the intestine and prevent “self-digestion.” Paneth cells secrete a protective factor - lysozyme. Macrophages are involved in protecting cells and the body from the penetration of bacteria and viruses with food into tissues.
Submucosa
The submucosal layer contains abundant nerve endings, blood vessels, lymphatic vessels, and Peyer's patches (lymph nodes).
Muscularis
The muscular plate is represented by smooth muscle circular fibers that ensure the movement of villi and motility of the intestinal tube.
Serosa
The serous membrane covers the loops of the small intestine and provides mechanical protection from damage and mobility.
Nutrition for pathology
To restore normal functioning of the body, it is important to follow the correct diet. All extraactive and irritating substances should be excluded from the diet. These are fried, spicy, salty foods, spices and alcohol. Allowed:
- soups from pureed vegetables, cereals;
- white bread crackers;
- boiled lean meats;
- buckwheat, oatmeal, semolina with milk;
- pasteurized milk and cream;
- pureed or steamed carrots, beets, potatoes, green peas.
You need to eat food in small portions 5–7 times a day. You should drink 1.5 to 2 liters of clean water. It is allowed to drink weak tea.
Functions of the small intestine
The small intestine includes several important functions in the digestive system.
- Digestive function. Ensures the breakdown and absorption of nutrients (vitamins, organic structures, water, salt, some medications) into the blood for delivery to all organs and systems of the body, the formation of final products that pass unchanged into the feces.
- Secretory function. This is the secretion of intestinal juice up to 2.5 liters per day, containing enzymes for processing proteins, fats, carbohydrates into the simplest substances - peptidase, lipase, disaccharidase, alkaline phosphatase and others.
- "Reservoir" function. It is determined by the accumulation and activation of the secretions of other glands - pancreatic juice, bile, which are released when food enters the stomach and 12 PCs and are involved in digestion.
- Endocrine function. It consists in the production by cells of the small intestine (especially in the 12 PCs) of hormones and mediators (histamine, serotonin, gastrin, motilin, cholecystokinin).
- Motor-evacuation function. Provides for contraction of the wall of the intestinal tube due to peristaltic waves, advancement and mixing of food masses (chyme), and the work of villi.
Preventive actions
The measures taken depend on the goals. If you need to prevent the development of the disease, follow the rules of personal hygiene, limit contact with bacteria carriers, eat right, and follow a daily routine.
If it is necessary to reduce the risk of exacerbations, you need to be examined by a gastroenterologist every year, do not deviate from the prescribed diet, stick to a diet, and do not self-medicate if suspicious symptoms occur.
Advantages of online registration at the International Center for Health Protection
A stomach ulcer is a chronic disease that requires the supervision of an experienced and qualified gastroenterologist. If you have been diagnosed with this or have clinical manifestations similar to this pathology, make an appointment with a doctor at the International Center for Health Protection.
We carry out accurate diagnostics, based on which we prescribe the optimal course of therapy. We have been providing medical services to Moscow residents for more than 14 years. The treatment regimen depends on the presence of complications, the severity of dysfunction, and the general condition of the patient; in each individual case it is determined individually.
You can make an appointment by phone or using the online form. We offer comfortable conditions for patients and their relatives.