The article was prepared by a specialist for informational purposes only. We urge you not to self-medicate. When the first symptoms appear, consult a doctor.
The main difference between erosive gastroduodenitis and other forms of this pathology is the presence of ulcers and erosions against the background of inflammation of the mucous membrane of the stomach and duodenum. At the same time, the normal functioning of the glands of the gastrointestinal tract is maintained.
Erosive gastroduodenitis is diagnosed mainly in young women and men. With this disease, surface defects appear on the mucous membrane. Ulcers and erosions do not penetrate the submucosal and muscular layers; they can be single or multiple. Erosive gastroduodenitis is accompanied by bleeding from mucosal defects, which over time leads to anemia.
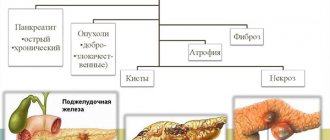
If the patient does not receive adequate treatment, the pathological process is complicated by the development of stomach and upper intestinal ulcers, cholecystitis, and pancreatitis. This form of gastroduodenitis is the most common among all pathologies of the gastroduodenal zone; the disease can be either acute or chronic. Compared to ordinary gastritis, erosive gastroduodenitis does not go into remission for a long time and is difficult to treat.
What is duodenitis? Functions of the duodenum duodenum
Duodenitis is an inflammatory disease of the duodenum. At the first consultation at Sarklinik, the doctor will tell you what duodenitis is , what are the causes, symptoms and signs of duodenitis. What is the difference between gastritis (inflammation of the stomach) and duodenitis (inflammation of the duodenum, 12 duodenum) and enteritis (inflammation of the intestines)? How to treat acute and chronic duodenitis , esophagitis, exacerbation of duodenitis, gastric reflux? Where is the duodenitis clinic located? What are the characteristics of erosive (incorrectly erosive) duodenitis, catarrhal, superficial, proximal, distal duodenitis, reflux duodenitis, giardiasis duodenitis in children? Why does reactive duodenitis occur in adolescents, atrophic, follicular, hemorrhagic, ulcerative, hypertrophic, diffuse duodenitis in adults? How to cure the diagnosis of weak, moderate, moderate, moderately severe, strong, severe duodenitis, bulbitis, cholecystitis, postbulbar duodenitis? What diet , nutrition , menu for duodenitis, gastritis? folk remedies , folk remedy treatment , herbal treatment, folk medicine, herbs, folk medicine, antibiotics, antibiotic treatment, diet 1, 2, 3, 4, 5, 6, 7, 8, 9 not help How to choose drug treatment if there is primary or secondary duodenitis, DGR? How dangerous is the disease, how to treat duodenitis? How to relieve pain due to duodenitis, why temperature, fever, hyperthermia? How is focal chronic duodenitis ? How to get rid of duodenitis , how to remove duodenitis? What does the army think about duodenitis? Where is the diagnosis of duodenitis , FGDS (fibrogastroduodenoscopy) with biopsy done? How does the duodenal bulb, gallbladder, stomach, intestines, pancreas suffer during inflammation? What can you eat for duodenitis, where to treat? Why does catarrhal gastritis, helminthic infestation, bulbitis, superficial gastritis, gastroduodenitis, esophagitis, dyskinesia, colitis, enterocolitis, gastritis, pancreatitis, cholecystitis, duodenal gastric reflux, hyperthyroidism, hypothyroidism, thyrotoxicosis, gallbladder dyskinesia occur?
Duodenitis of the duodenum - diagnosis
After collecting an anamnesis and examining the patient, the doctor will prescribe a number of additional examinations: esophagogastroduodenoscopy (EFGDS), ultrasound examination of the abdominal organs, examination of gastric juice (composition and acidity), coprogram, general blood test and biochemistry, X-ray and duodenoscopy. If oncology is suspected, a special examination will be scheduled.
After receiving the results, the specialist will tell you how to treat exacerbation of duodenitis and outline a diet that you need to follow for a month. Only after the specified period has passed and in the absence of symptoms can the diet be expanded. Nutrition for superficial duodenitis should be gentle on the gastrointestinal tract, but beneficial for the body.
Duodenum, 12 duodenum: treatment
The duodenum is an important organ of the digestive system and digestive behavior. The intestinal cavity is a reservoir into which digestive juices flow from the pancreas, liver and glands of the wall of the small intestine. Here, cavity digestion begins to take place, preparing the food bolus for the final breakdown of nutrients in the brush border of the cells of the duodenal mucosa. Between the microvilli, abundantly covered with enzymes, the bulk of the nutrients entering the human body are digested and absorbed at high speed. This digestion in the brush border is called parietal. The duodenum is richly innervated, especially in the initial section and in the area of confluence of the ducts from the gallbladder and pancreas. In the muscular lining of the intestine there are sensors for the rhythm of contractions of the entire small intestine.
The duodenum is also a hormonal organ. In the intestinal wall, under the influence of gastric contents, enterogastron is produced, which suppresses the secretion of gastric juice and relaxes the muscles of the stomach wall. Enterogastron prevents the digestive hormone gastrin from stimulating the activity of the gastric glands. Gastrin is produced by the pyloric zone of the stomach, which is close in origin and structure to the duodenum. The duodenum secretes pancreozymin, cholecystokinin, secretin and other hormones that regulate the activity of the pancreas and gallbladder, while simultaneously stopping gastric secretion. Digestive hormones from the duodenum stimulate the intestinal glands, which actively begin to secrete juice and stimulate intestinal motility. In the duodenum, hormones of general action are found that affect the body’s metabolism, endocrine, nervous, and cardiovascular systems.
Causes
Erosive gastroduodenitis can occur against the background of the aggressive influence of various negative factors - external and internal. Most often, the following exogenous factors lead to the development of this pathology:
- Helicobacter pylori infection;
- prolonged stress;
- poor nutrition;
- gastrointestinal diseases.
- eating rough or spicy foods, hot or too cold drinks;
- taking medications (non-steroidal anti-inflammatory drugs, glucocorticoids);
- alcohol abuse.
Among the endogenous causes, it is worth highlighting hereditary genetic disorders, increased production of hydrochloric acid, the presence of reflux of duodenal contents into the stomach, a decrease in the protective properties of gastric mucus, intestinal infections, and concomitant pathology of the liver and pancreas.
Acute duodenitis
Acute duodenitis usually occurs in combination with acute inflammation of the stomach and intestines as acute gastroenteritis, gastroenterocolitis. Morphologically there are:
1) catarrhal acute duodenitis;
2) erosive-ulcerative acute duodenitis;
3) phlegmonous acute duodenitis.
According to the predominant clinical manifestations, various forms of duodenitis are distinguished:
1) resembling duodenal ulcer;
2) resembling chronic gastritis;
3) resembling cholecystitis;
4) resembling acute gastritis;
5) resembling appendicitis.
Acute duodenitis occurs as a result of exposure to a number of factors on the body:
1) food toxic infections;
2) poisoning with toxic substances that have an irritating effect on the mucous membrane of the digestive tract;
3) excessive intake of very spicy food, usually in combination with large amounts of strong alcoholic drinks;
4) damage to the duodenal mucosa by foreign bodies.
EROSIVE CONDITIONS OF THE GASTRODUODENAL AREA
From a modern point of view, erosions of HDSO are considered as the morphological equivalent of homeostasis disorders. After the widespread introduction into clinical practice of fibroendoscopic examinations of the upper gastrointestinal tract, the frequency of detection of HDSO erosions has increased markedly. The article discusses issues of epidemiology, pathogenesis, clinical picture, treatment and prevention of erosions of HDSO. The paper deals with gastroduodenal mucosal erosions (GDMEs). From the current knowledge, GDMEs are considered as a morphological equivalent to hemostatic disorders. After wide introduction of fibroendoscopic studies of the upper gastrointestinal tract into clinical practice, the detection rates for GDMEs noticeably increased. The paper considers the epidemiology, pathogenesis, clinical presentation, and prevention of GDMEs.
V.B. Grinevich, Prof. Department of Therapy, Faculty of Advanced Training for Physicians,
St. Petersburg U.P. Uspensky, Ph.D. Department of Gastroenterology, Military Medical Academy, St. Petersburg
Prof. VB Grinevich, Department of therapy, Faculty for Postgraduate Training of Physicians, Saint Petersburg Yu. P. Uspensky, Candidate of Medical Science, Department of Gastroenterology, Military Medical Academy, Saint Petersburg
Erosions of the stomach and duodenum are defects of the gastroduodenal mucosa (GDM), arising at the site of foci of superficial necrosis and not reaching its muscular layer.
Erosions of the HDSO were first described by the Italian anatomist Morgagni back in 1761 in the work “On the location and causes of diseases identified by the anatomist,” based on the study of extensive sectional material. Subsequently, the study of the process of erosion of HDSO, mainly as a pre-ulcerative condition, was reflected in the works of K. Rokitansky (1842). Some attention to the problem of superficial destructive changes in the HDSO was also paid by major researchers of the domestic therapeutic school in not so distant times (Yu.M. Lazovsky, V.Kh. Vasilenko). An increase in special interest in this form of pathology of the gastroduodenal part of the gastrointestinal tract has been noted in the last 10–20 years, which is due to the widespread introduction of endoscopic research methods into medical practice. Today it has become clear that erosions of HDSO are the morphological equivalent of deep disorders of homeostasis, realized through changes in metabolism, immunoreactivity and microcirculation processes. Thus, it is more correct to speak not about local erosive defects as such, but rather about erosive conditions of the gastroduodenal region [1]. An important milestone in the study of the problem was the establishment of the fact that, along with rapidly passing acute banal erosions (BE), there are chronic complete erosions (PE) with a progressive nature of the clinical course [2]. Acute (based on the criterion of duration of existence) include flat erosions, the period of epithelization of which does not exceed 2–7 days; to chronic – existing, without undergoing reverse development, for 30 days or more [3]. Endoscopically, acute erosions are superficial flat polymorphic (point, linear, polygonal) defects of HDSO, covered with fibrin or hydrochloric acid hematin (hemorrhagic erosions), and chronic - elevated (complete) erosions - round polypoid formations, mature and immature. When analyzing the degree of maturity of PE based on endoscopy data, it is necessary to be guided primarily by an assessment of the state of the surface epithelium of polypoid formations and classify as immature those PE that have only a rim of hyperemia at the apex. If there are signs of necrosis and desquamation of the surface epithelium, PE is considered mature. In turn, endoscopically diagnosed mature PE correspond to the clinical stage of exacerbation of chronic erosive gastritis (CEG), and immature ones correspond to its remission.
Epidemiology
According to the literature, BE of HDSO are more common in men in ratios from 4: 1 to 2: 1. At the same time, in childhood, erosive changes in HDSO are more often observed in girls. There is evidence that chronic erosions of HDSO also predominate in men, but with less consistency (from 2:1 to 1.1:1). Erosive changes in the HDSO are often detected already in childhood. Subsequently, both acute and chronic erosions of HDSO are diagnosed in patients with CEG of different age categories, however, there is a very clear tendency towards an increase in the frequency of formation of PE of HDSO in older people (in 60–70% of cases, PE is detected in people over 40 years old). Evidence of the widespread prevalence of erosive changes in the HDSO is their detection in sections on average in 6% of those who died from various diseases. The frequency of detection of HDSO erosions in general somatic patients examined endoscopically varies from 2 to 20%. Among diseases combined with erosive changes in the gastrointestinal tract, peptic ulcer of the stomach and duodenum is in first place in terms of frequency of occurrence (from 1/3 to 1/2 of cases). Moreover, if BE of HDSO are combined with ulcerative disease of the stomach and duodenum in approximately equal proportions, then chronic erosions are somewhat more often associated with ulcerative disease with localization of the ulcerative defect in the duodenal bulb [4]. Among other diseases combined with erosive gastritis (EG), diseases of the liver, pancreas, heart, blood vessels and lungs should be highlighted. The frequency of development of erosive changes in HDSO in patients with chronic hepatitis and cirrhosis of the liver is very significant (from 10 to 40% of cases) [5]. At the same time, chronic erosions of HDSO are more often combined with liver cirrhosis with portal hypertension of alcoholic etiology, while acute erosions are more often combined with postnecrotic cirrhosis of viral etiology. In addition, on average, 1/4 of patients with CEG suffer from concomitant chronic pancreatitis. Quite often (up to 30% of cases) erosions of HDSO are diagnosed in patients with chronic nonspecific bronchopulmonary diseases, as well as with acute destructive processes in the lungs (abscess, gangrene). Finally, literature data indicate that erosive changes in HDS in 20–30% of cases are accompanied by cardiovascular diseases such as coronary heart disease, hypertension, systemic atherosclerosis, as well as heart defects accompanied by circulatory failure.
Etiopathogenesis
Taking into account the etiology, acute erosions are divided into primary and secondary. Primary (exogenous) include erosions induced by stressful situations, as well as exposure to the mucous membrane (MS) of external factors (ethanol, ulcerogenic medications, occupational hazards, etc.). Secondary (endogenous) are formed as a complication of various diseases (elimination uremic gastritis, gastric cancer and lymphomatosis, anemia, Crohn's disease, other immunopathological processes, etc.) [6, 7]. Histologically, such erosions, regardless of origin, represent desquamation of the superficial pit epithelium and superficial necrosis of the mucus (superficial necrotic or desquamation erosions).
According to etiology, chronic erosions
are also divided into
primary (stressogenic-adaptogenic)
, which, as a rule, arise in practically healthy young people without concomitant diseases under the influence of unfavorable socio-climatic or psychotraumatic factors and can undergo involution as their influence is eliminated. Histologically, such erosions correspond predominantly to hyperplastic PE of “young” people with foveal and simple regenerative hyperplasia as a manifestation of desynchronization of the processes of cell proliferation and differentiation (evolving erosions). Such PE in young people in 30% of cases, according to dynamic endoscopic observation, can undergo reverse development. Moreover, the duration of their existence does not exceed 2–3 months.
To secondary (somatogenic)
include chronic erosions that occur more often in middle and older age as a local equivalent of the syndrome of generalized circulatory-hypoxic disorders, altered immunoreactivity and metabolism of the body against the background of diseases of the cardiovascular system (chronic coronary heart disease, hypertension) and liver (chronic hepatitis and cirrhosis ), which are combined with PE with a frequency of up to 75% of cases. Histologically, such erosions correspond predominantly to fibrous-fibrinoid erosions (non-evolving erosions, torpid form). Such PE lasts for 6 months or more, the possibility of their spontaneous involution becomes unlikely, and the erosive process becomes truly chronic. Regarding the role of Helicobacter pylori in the pathogenesis of EH, it should be noted that this microorganism is less often detected in young people with a mild or asymptomatic clinical course of EH, while in patients with BE, OM, primarily in combination with ulcer, is determined with a fairly high frequency (from 75 to 70% of cases) [8]. However, there is no compelling reason to assume a connection between the contamination of SB with Helicobacter pylori and the nature of the clinical manifestations of EG, since most likely the dissociation in the frequency of detection of Helicobacteriosis is due to the different severity of gastric inflammatory-dystrophic and atrophic changes in the gastrointestinal tract in people of different age categories. In contrast to BE HDSO, chronic erosions already at a young age are closely associated with Helicobacter pylori, which is subsequently detected in patients with BE HDSO with great consistency, regardless of the combination of BE and PU. Apparently, Helicobacter pylori is not the main pathogenetic factor in the development of a chronic erosive process. It also seems unlikely that it will influence the clinical manifestations of the disease. At the same time, the participation of Helicobacter pylori in the formation of mechanisms of the progressive course of CEG with PE CO is very possible.
Clinical course
When studying the features of the clinical symptom complex of EG with BE and PE of HDSO, its pronounced dependence on the type of erosive changes and the age of the examined was established. Analysis of the features of clinical manifestations of EG indicates that they are primarily determined by the type of erosive lesion of the HDSO. Thus, EG with EB OM do not have a clearly defined clinical symptom complex, while the clinical manifestations of other diseases against which EB develop (ulcerative disease of the stomach or duodenum, chronic hepatitis, cirrhosis of the liver, etc.) come to the fore. It is important that in young people with predominantly unchanged OM and without connection with concomitant diseases, EB in 30–70% of cases may not have any clinical manifestations. The observed symptoms are, as a rule, scanty and nonspecific: the most common are heartburn, sour belching, and extremely rarely, low-intensity fasting and “hungry” pain in the epigastrium. EG with BE SO is characterized by the development of hemorrhagic complications [9]. On the contrary, for patients with EG with PE HDSO, the manifestations of dyspeptic and abdominal pain syndromes are very pronounced and quite specific. Belching and heartburn are persistent and are observed in 75% of patients with PE, often combined with heaviness in the right hypochondrium and flatulence, primarily in patients with concomitant chronic duodenitis and terminal esophagitis. Periodic, fasting and “hungry” pain in the epigastrium, characteristic of the vast majority of patients with PE, often radiates to the spine. Moreover, if in young patients with PE aching and dull pain predominate, then in older age groups the pain against the background of increasing severity in the epigastrium is predominantly cramping in nature with the addition of nausea, stool instability with a predominance of constipation. Thus, the clinical picture of CEG with PE HDSO reveals a certain similarity with the clinical picture of ulcerative disease with antral or duodenal localization of the ulcerative defect. A fairly frequent predominance of pronounced symptoms of underlying diseases in patients with PE was also noted. These include primarily diseases of the cardiovascular system (hypertension, coronary heart disease) and liver (chronic hepatitis and cirrhosis). With a combination of erosive and ulcerative processes within the HDSO, the features of the clinical course of ulcerative disease also depend on the type and location of accompanying erosive changes. It is especially important that superficial destructive changes in the HDSO are an important marker of the intensity of reparative processes in the edge of the ulcer. Thus, PE is reliably associated with an increase in the time of scarring of ulcerative defects by at least 7–14 days, while when an ulcer is combined with BE of HDSO, its healing time in the vast majority of cases is reduced by an average of 3–5 days [10, 11]. The development of erosive processes in the gastrointestinal tract, especially chronic erosion, is closely related pathogenetically to diseases of the cardiovascular system such as hypertension and coronary heart disease. Moreover, it has been established that PE of HDSO can serve as an early preclinical marker of these diseases, i.e., the detection of PE indicates a threat of developing cardiovascular pathology in the future. Hemorrhagic complications are relatively common (4.5% of cases) in acute erosive lesions of the mucous membrane and are practically not observed as a complication of CEG with PE of the mucous membrane. At the same time, according to literature reports, in isolated cases, with the predominant development of one of the components of the morphological substrate, they can transform into polyps of the corresponding type (hyperplastic, fibrosing, etc.). Isolated cases of malignancy of PE HDSO have also been described.
Diagnostics
Differentiation of the two types of erosions, as well as other pathological formations in the stomach and duodenum, is usually carried out by the method of fibrogastroduodenoscopy. In this case, BE of HDSO are visualized in the form of flat surface defects of the SO epithelium of various shapes. PE HDSO endoscopically look like polyp-like formations with umbilical depressions at the apexes, made with fibrin or hydrochloric acid hematin. In this case, the sizes of polypoid formations of PE range from 3 to 10 mm, their number ranges from 1 to 15, and PE are located, as a rule, in the form of chains in the antrum of the stomach. During the period of remission of CEG, there may be no umbilical depressions at the apexes of the PE, but there may be only a rim of hyperemia. Histological BE of HDSO are stereotypically characterized by necrosis and desquamation of the superficial pitted epithelium. Neutrophilic-eosinophilic or lymphocytic infiltration of the mucous membranes of the pererosive zone is characteristic. In the surrounding acute erosions of the mucous membrane, the phenomena of superficial or diffuse gastritis predominate; less often, the mucous membrane is atrophic or histologically unchanged. At the same time, the morphological signs of PE are: foveal hyperplasia of the epithelium, elongation and expansion of the gastric glands. There is evidence of the presence in the PE zone of areas of stromal fibrosis, fibrinoid necrosis of the mucus, and polymorphic cell, predominantly lymphoplasmacytic, infiltration of the mucus. In contrast to patients with EB, atrophic or atrophic-hyperplastic gastritis is characteristic of the mucous membrane of the peri-erosive zone in patients with PE, while histologically unchanged gastritis is detected extremely rarely. The opinion that PE SOs can histologically correspond to ulcerated benign gastric polyps, as well as data according to which PEs are often located at the tops of hyperplastic polyps deserve special attention. For the purpose of differential diagnosis of PE and polyps with erosions at the apex, as well as if malignancy is suspected, it is recommended to obtain research material using a “loop” rather than a pinch biopsy. X-ray diagnostics of CEG is used in patients with contraindications to fibrogastroduodenoscopy, when refusing it and the need to differentiate between erosive and infiltrative processes. Data on the effectiveness of X-ray diagnostics of erosive changes in the HDSO are contradictory. There is evidence that when using the pneumorelief technique (double contrast) in combination with dosed compression on the anterior abdominal wall, an image of HDSO erosions can be obtained in the form of small rounded elevations with a diameter of 1 - 3 mm with a tiny shadow of a contrast agent accumulation detected in the center. X-ray differentiation of PE from wide-based gastric polyps allows their characteristic arrangement in the form of chains converging towards the antrum of the stomach, in combination with superficial barium depots at the apexes.
Treatment and prevention
Patients with CHE can be treated on an outpatient basis if the patient has good social and living conditions and medications are available in the pharmacy network. The exception is patients with CEG with PE HDSO against the background of decompensated diseases of the cardiovascular system and liver, which require inpatient treatment mainly for the purpose of correcting the underlying disease. Treatment
EG with BE GDSO involves, first of all, the elimination of unfavorable factors of an exogenous and endogenous nature, i.e.
elimination of stressful influences, normalization of diet and quality of nutrition, cessation of smoking and drinking alcohol, and taking drugs with ulcerogenic properties. Drug treatment in this case has no special features: antacids (Maalox, etc.) are prescribed in dosages adequate to the acid-neutralizing activity of the drug. The use of this therapy allows in 70% of cases to achieve clinical and endoscopic remission of the disease in 5–10 days, while the period of epithelization of BE does not exceed 5–8 days. In cases of combination of CEG with gastroesophageal reflux disease, the prescription of foaming antacids (Topalkan, Gaviscon) containing alginic acid is indicated. These drugs, interacting with hydrochloric acid, form foam on the surface of the gastric contents, covering the esophagus with each episode of reflux. The persistence of clinical symptoms during treatment is associated with the slow disappearance of acute inflammatory phenomena in the perierosive mucus and is accompanied by a disruption of the motor-evacuation relationship in the gastroduodenal zone. In the latter case, the prescription of motor activity regulators (cisapride, domperidone, metoclopramide) is justified. In case of the recurrent nature of acute erosion and the threat of transformation of EG into ulcer, the use of histamine H2 receptor blockers (ranitidine, famotidine) in short courses with mandatory gradual withdrawal of the drug may be indicated. Prescription of proton pump inhibitors (omeprazole, pantoprazole, lansoprazole) to patients with HDSO erosions is indicated in complicated cases, for example, in the treatment of CEG complicated by bleeding. Course treatment with proton pump inhibitors also requires gradual withdrawal of the drug. Subsequently, the patient can be transferred to taking H2 blockers or antacids. Therapy of CEG with PE SO should be based on the fact that for the majority of patients with chronic erosions who have diseases of the cardiovascular system, liver and biliary tract, pancreas, decompensation of these diseases, which was the main reason for placing patients in a therapeutic hospital, coincides with time with the onset of exacerbation of CEG. Conversely, comprehensive adequate drug treatment, for example, of hypertension combined with PE HDS, makes it possible to achieve sustainable compensation for both diseases. This clearly demonstrates the unique properties of PE not only as a local morphological equivalent of diseases of the cardiovascular and hepatobiliary systems, but also as a concomitant clinical marker reflecting the nature of their course. One of the methods of etiopathogenetic treatment of CEG with PE SO is local immunocorrective therapy using a donor leukocyte mass injected into the area of the apex of PE, in combination with sessions of hyperbaric oxygenation. Among other methods, we should recommend the use of solcoseryl, which activates the activity of oxidative phosphorylation enzymes and improves oxygen utilization. The effectiveness of etiopathogenetic therapy for EG with PE HDSO increases with the prescription of cytoprotective drugs - film-forming drugs (sucralfate) or synthetic analogues of prostaglandins (misoprostol). Anti-Helicobacter therapy leads to a significant reduction in the incidence of exacerbations of CEG. Prevention of
EG with BE of HDSO should include optimization of diet, work and rest. It is important that ulcerogenic drugs are prescribed only as drugs of choice and in combination with antacids and cytoprotective drugs. In order to prevent relapse of the disease, it is also necessary to prescribe anti-relapse drug therapy for at least 3-4 weeks in the autumn-spring period. In this case, it is advisable to use antacids (Remagel, Topalkan, Maalox), as well as drugs with astringent and enveloping effects (Vicalin, Vikair, Rotor). Prevention of EG with PE HDSO, in addition to these general measures, should be aimed primarily at adequate treatment of such diseases of the cardiovascular system as coronary heart disease and hypertension, as well as diseases of the biliary tract and liver (chronic hepatitis, cirrhosis of the liver, dyskinesia biliary tract) and pancreas (chronic pancreatitis). Moreover, the entire complex of measures to minimize risk factors for these diseases equally contributes to preventing the development of EG with PE HDSO. During the period between relapses, drinking mineral waters of low and medium mineralization should be used. Patients should be referred for sanatorium-resort treatment no earlier than 1 month after the exacerbation of the disease has stopped. Of the physiotherapeutic factors for existing liver damage, decimeter wave therapy is indicated, and for the pancreas, treatment with sinusoidal modulated currents is indicated. Physiotherapeutic treatment for patients with EG is contraindicated in the acute phase of the disease, the presence of a concomitant single polyp of the gastric mucosa, as well as in cases of suspected neoplasm. Patients with EG with BE of HDSO with a recurrent nature of the disease (two or more relapses per year) or with a clinical course complicated by bleeding require constant medical supervision. Control endoscopic examinations should be carried out 3, 6 and 12 months after relapse of the disease. Considering the risk of oncological complications in patients with PE HDSO, there is a need for their constant dynamic monitoring. Control endoscopic examinations with targeted biopsy from the edge of the PE and histological analysis of gastrobiopsy material should be carried out at least once a year for patients under 30 years of age and at least once every 6 months for older patients.
Conclusion
The unique features of chronic erosions of GDS (existence without regression for decades, permanent fibrinoid necrosis in the morphological substrate, not recognized by phagocytes, morphological proximity to gastric polyps, and according to clinical manifestations - to ulcer) predetermine the continued interest in the study of this form of pathology of the gastroduodenal zone of the gastrointestinal tract. intestinal tract, primarily in terms of their clinical and prognostic features, determining their place in the overall structure of morbidity.
Literature:
1. Grinevich V.B., Uspensky Yu.P., Grigoriev V.P., Kalinin A.V. Erosive changes in the gastroduodenal mucosa - a pre-ulcerative condition? // Wedge. honey. – 1991. – T. 69, No. 11. – P. 57–9. 2. Grinevich V.B., Tkachenko E.I., Uspensky Yu.P. Classification of erosions of the mucous membrane of the stomach and duodenum // Klin. honey. – 1996. – T. 74, No. 1. -S. 75–6. 3. Walk L., How long can a gastric erosion persist? // Radiologe. – 1991. – Jg. 31. H.1. – S. 38–9. 4. Vasiliev Yu.V., Rishi K.M. Treatment of duodenal ulcer combined with chronic gastric erosions // Klin. honey. – 1991. – T. 69, No. 7. – P.52–3. 5. Loginov A.S., Blok Yu.E., Vasiliev Yu.V., Burdyukova O.P. Treatment of erosive and ulcerative lesions of the upper gastrointestinal tract in decompensated cirrhosis of the liver // Sov. honey. – 1989. – No. 11. – P. 82–3. 6. Ilchenko A.A. Peptic ulcer in combination with erosive gastritis // Modern problems of gastroenterology and hepatology: Scientific materials. session - Tbilisi: B. i., 1988, - pp. 250–2. 7. Bernersen B., Johnsen R., Straume B., Burhol PG. Erosive prepyloric changes in dyspeptic and non-dyspeptic in a defined population. The sorreisa gastrointestinal disorder study // Scand. J. Gastroenterol. – 1992. – Vol. 27, No. 3. – R. 233–7. 8. Preobrazhensky V.N., Klimov N.P., Katkov V.I. and others. Treatment of patients with long-term non-healing duodenal ulcers in combination with chronic gastric erosions in the presence of Helicobacter pylori // Doctor. case. – 1991. – No. 2. – P. 87–9. 9. Borgiorno A., Rini G.B., Rotollo G. et al. Follow-up duodeno erosivo emorragico. Valutazioni del rischio di UD // Minerva dietol. gastroenterol. – 1985. – Vol. 31, No. 2. – R. 131–3. 10. Grinevich V.B., Tkachenko E.I., Uspensky Yu.P. and others. Peptic ulcer of the stomach and duodenum in combination with erosions // Doctor. case. – 1991. – No. 4. – P. 40 – 3. 11. Grinevich V.B. Clinical and biological patterns of the peptic ulcer prediction system: Abstract of thesis. diss. Dr. med. Sci. – St. Petersburg. – 1994. – 42 p.
Acute duodenitis: symptoms, signs
What are the signs and symptoms of acute duodenitis ? The clinical picture of acute duodenitis is characterized by symptoms such as epigastric pain , nausea, vomiting, general weakness, pain on palpation in the epigastric region, and increased temperature. The diagnosis is confirmed by FGDS (fibrogastroduodenoscopy), which detects inflammatory changes in the duodenal mucosa. With phlegmonous duodenitis, the patient’s general condition sharply worsens, tension in the abdominal wall muscles in the epigastric region is determined, a positive Shchetkin-Blumberg sign is detected, and an increase in temperature is noted.
Acute catarrhal duodenitis and erosive-ulcerative duodenitis often end in self-healing within a few days. With repeated duodenitis, a transition to a chronic form is possible. Complications of acute duodenitis are intestinal bleeding, perforation of the intestinal wall, and the development of acute pancreatitis.
Chronic duodenitis: causes
Chronic duodenitis is a chronic inflammation of the duodenum. The occurrence of chronic duodenitis is facilitated by irregular nutrition with frequent consumption of spicy, irritating, too hot foods ( primary chronic duodenitis ). Secondary chronic duodenitis is observed in diseases such as chronic gastritis, peptic ulcer of the stomach and duodenum, chronic pancreatitis, food allergies, giardiasis, uremia. In the pathogenesis of chronic duodenitis, the direct effect of the irritating agent on the mucous membrane of the duodenum and the proteolytic effect of active gastric juice on it are important.
Treatment of erosive gastroduodenitis
Diet therapy
A necessary component of effective treatment of erosive gastroduodenitis is adherence to a proper diet. This is especially important during an exacerbation period, when a gentle diet should be prescribed. It provides for the complete exclusion of fried, fatty and spicy foods, carbonated liquids and rich broths. You should also exclude too coarse, cold or hot foods from your diet. Meals should be small and frequent, at least five times a day.
Drug therapy
Drug therapy primarily involves eradicating Helicobacter pylori infection when it is detected. For this purpose, first or second line circuits are used. The first line is three-component eradication therapy, which includes a proton pump inhibitor (omeprazole, rabeprazole, etc.), amoxicillin and clarithromycin. If it is ineffective, second-line therapy is prescribed. It involves the appointment of an antisecretory drug, tetracycline, metronidazole and bismuth preparations.
It is also necessary to use drugs to protect the mucous membrane, which include antacids and alginates. An important component of the treatment of erosive gastroduodenitis are cytoprotectors: bismuth and sucralfate. These products form a protective film over the erosions, which prevents the aggressive influence of increased acidity on them.
It is recommended to prescribe reparatives and antioxidant therapy, which improves regenerative processes in the mucous membrane. Vitamins A, E and C are used for this purpose. Antispasmodic drugs such as drotaverine and papaverine are used to reduce pain. If the cause of the development of erosive gastroduodenitis is psycho-emotional stress, patients are advised to take sedatives.
Classification of chronic duodenitis
Classification of chronic duodenitis:
1) chronic duodenitis , mainly bulbitis , of acidopeptic origin;
2) chronic duodenitis, combined with atrophic gastritis or enteritis;
3) chronic duodenitis that developed against the background of duodenostasis;
4) local duodenitis (papillitis, peripapillary diverticulitis).
According to the endoscopic picture there are:
1) superficial chronic duodenitis;
2) atrophic chronic duodenitis;
3) interstitial chronic duodenitis;
4) erosive-ulcerative chronic duodenitis.
What is catarrhal duodenitis
Taking into account the clinical picture, acute (catarrhal, phlegmonous and ulcerative) and chronic duodenitis are distinguished. The latter can be primary or secondary. Primary develops against the background of poor nutrition, smoking and alcohol abuse. The causes of the secondary are diseases of the stomach, liver and gall bladder.
Clinical classification:
- chronic acidopeptic bulbitis (develops against the background of chronic gastritis);
- chronic duodenitis with enteritis;
- duodenitis due to insufficient mobility of the duodenum;
- local duodenitis.
You can find out more about what catarrhal duodenitis is on our website Dobrobut.com. Make an appointment with a specialist around the clock.
Chronic duodenitis, symptoms of chronic duodenitis
What are the signs, manifestations, symptoms of chronic duodenitis ? The clinical picture of chronic duodenitis is characterized by such signs as constant, dull or ulcer-like pain in the epigastrium , a feeling of fullness or distension in the upper abdomen after eating, decreased appetite (poor appetite), vomiting, nausea. On palpation, pain is noted in the epigastric region.
With proper treatment, the prognosis is favorable. With the erosive-ulcerative form of duodenitis, various complications can often occur, most often intestinal bleeding.
The clinical picture of duodenitis is diverse and nonspecific. Isolated chronic duodenitis is rare. It is combined with chronic gastritis, peptic ulcer, enteritis, pancreatitis, and diseases of the biliary tract.
Main symptoms of the disease
In the acute form, the patient complains of general weakness, nausea, vomiting, severe pain in the pit of the stomach, and severe night pain.
The symptoms of chronic duodenitis are more smoothed out. Most often the patient is concerned about:
- heartburn, belching;
- decreased appetite;
- headache, irritability;
- feeling of fullness in the stomach;
- aching pain in the pit of the stomach.
Duodenitis against the background of intestinal diseases is characterized by intestinal manifestations - loose stools, flatulence, pain in the intestines. If the pathology has developed as a result of duodenostasis, the patient will complain of severe pain in the right hypochondrium, rumbling in the abdomen and bitterness in the mouth.
Diagnosis of chronic duodenitis, differential diagnosis
Diagnosis of chronic duodenitis is carried out using diagnostic methods such as fibrogastroduodenoscopy with biopsy, duodenoscopy, pH-metry, floor-by-floor manometry, impedance measurement. In parallel with the diagnosis of duodenitis, other digestive organs are examined.
Often duodenitis simulates duodenal ulcer. People of all age groups suffer from duodenitis. More often, inflammation of the duodenum occurs in young women, in whom duodenitis can be severe, accompanied by various disturbances in the activity of the central nervous system and endocrine glands. Duodenitis often occurs in childhood, which is facilitated by the inherited weakness of the hormonal apparatus of the duodenum, the variability of its shape, mobility and location in relation to the axis of the body.
The duodenum does not have a mesentery. In the case where the embryonic mesentery is preserved, the intestine is abnormally mobile and forms additional loops. Part of the liquid food mass flowing through the duodenum gets stuck in the additional elbow, creating favorable conditions for the proliferation of microorganisms in the intestinal cavity. When exposed to alcoholic drinks or irritating foods, an inflammatory process occurs. An obstacle to the passage of food through the duodenum also appears when it is located in the opposite direction relative to the axis of the body.
What contributes to the development of duodenitis?
What diseases contribute to duodenitis? Giardiasis , ascariasis, chronic infection in the oral cavity, pharynx, genitals, gall bladder, and renal failure contribute to the development of duodenitis.
The inflammatory process can be sluggish, manifested by disturbances in appetite and general well-being, and mild dyspeptic symptoms. Patients experience lethargy and mental instability. Children grow up thin and develop poorly.
When infected with Giardia, the clinical picture of duodenitis can develop rapidly. Suddenly, usually after an error in diet, an attack of severe abdominal pain occurs, causing patients to squirm. The pain is not relieved by antispasmodics. The patient's face becomes hyperemic and becomes covered with drops of sweat.
Dowdenitis complications
What are the complications of duodenitis ? A severe complication of long-term duodenitis is duodenal hormonal insufficiency. Inflammation, destroying the duodenal mucosa, causes death and inhibition of cells that secrete hormones. The appearance of symptoms of duodenal insufficiency is facilitated by congenital weakness of the endocrine apparatus of the duodenum, hypoxia, and concomitant chronic infectious diseases. Insufficiency of the hormonal function of the duodenum causes indigestion, carbohydrate metabolism, significant emaciation or weight gain. Severe neuropsychic and cardiovascular disorders occur.
In young women, duodenal hormonal insufficiency begins to manifest itself in the premenstrual period. Headaches, nausea, vomiting, irritability appear, and performance decreases. Attacks of severe weakness can last from one to four weeks. Weakness is accompanied by palpitations, heart pain, nausea, vomiting, often in the morning on an empty stomach. Patients lose their ability to work, interest in life and family. In a number of patients, attacks of weakness with trembling, pain in the heart, and frequent urination occur immediately after eating or several hours later, less often at night.
Duodenal hormonal insufficiency in acute and chronic duodenitis, duodenostasis is manifested by diencephalic, dumping, Meniere-like, hypoglycemic syndromes, attacks of severe weakness, dizziness, headaches, tachycardia, weight loss, muscle atrophy, depression. There is a dysfunction of other endocrine organs, especially the insular apparatus.
Treatment of duodenitis in Saratov, treatment of chronic duodenitis
Complex differentiated treatment of duodenitis in Saratov, treatment of chronic duodenitis in Saratov, treatment of patients with chronic duodenitis and gastroduodenitis with the widespread use of new reflexology techniques allows you to achieve satisfactory results even with a pronounced clinical picture of the disease! Sarklinik knows how to treat duodenitis, how to cure duodenitis, how to get rid of duodenitis.
Sign up for a consultation. There are contraindications. Specialist consultation is required.
Photo: Wacpan | Dreamstime.com\Dreamstock.ru. The people depicted in the photo are models, do not suffer from the diseases described and/or all similarities are excluded.
Related posts:
Spasm of the esophagus: treatment, causes, how to relieve, treat cardiospasm of the esophagus, esophagospasm
Duodenitis: treatment, symptoms, chronic, erosive, superficial, cactar, how to treat
Belching, treatment, frequent rotten belching of air, eggs, food
Stomach ulcer, duodenal ulcer, peptic ulcer: treatment in Saratov
Hepatomegaly, steatosis, fibrosis, alcoholic hepatitis, liver cirrhosis, alcohol damage