When testing for dysbacteriosis in a child’s body, a tendency is immediately revealed that confirms the immaturity of the organs of the digestive system. At the same time, this type of analysis confirms the existing imbalance in the intestinal microflora. Most often, with dysbacteriosis in infants or newborns, there is a risk of having any diseases, as a result of which a malfunction occurred in the body. In most cases, dysbiosis does not have pronounced symptoms and is usually similar to any other disease of the digestive tract. In this regard, it becomes quite difficult to determine and identify dysbiosis in the child’s body. Therefore, submitting stool for analysis is one of the reliable and accurate laboratory methods that can confirm this diagnosis. What will be the interpretation of the test for dysbacteriosis in children?
Intestinal microflora
Intestinal microflora is the internal microbiological environment inhabited by microscopic organisms. A stable qualitative and quantitative composition of bacteria ensures the healthy condition and functionality of the intestinal sections of the digestive system (large and small intestine).
Microflora takes part in metabolic processes, regulation of cellular immunity, absorption of nutrients, synthesis of amino acids and B vitamins. When the balance of the microenvironment is disturbed, intestinal disorders, pathologies of a bacterial nature, and chronic diseases of the gastrointestinal tract develop.
Representatives of the intestinal microenvironment are:
- Normal beneficial anaerobes (microorganisms living without oxygen), making up more than 90% of the total number of bacteria. The intestinal group includes lacto-, bifido-, enterobacteria, enerococci and Escherichia coli.
- Opportunistic gram-positive and gram-negative facultative (non-strict) anaerobes, the number of which is strictly limited (with active reproduction they provoke bacteriological disorders). This category includes streptococci, staphylococci, Klebsiella, fungi of the genus Candida, clostridia, Helicobacter and other microorganisms.
In addition, there are pathogenic microorganisms whose presence in the intestines is not intended. They penetrate from the external environment and cause infectious diseases (shigellosis, salmonellosis, cholera, etc.). The activity of opportunistic pathogens manifests itself under negative exocrine (external) influence, against the background of weakened immunity.
What does ejaculate culture show?
All bacteria, viruses and other microorganisms that can be detected in semen are divided into groups:
- symbionts - physiological microflora that does not cause harm to the human body, takes an active part in maintaining the biocenosis;
- opportunistic - do not cause harm at their normal concentrations, but can cause the development of pathology if permissible standards are exceeded. For example, staphylococcus is found in any man, but in normal quantities the microbe does not pose any threat to the body. When exposed to various endogenous or exogenous factors, the microbe can begin active division. In such situations, staphylococcus in sperm culture in large quantities may indicate the development of cystitis, urethritis, vesiculitis, prostatitis;
- pathogenic – normally such pathogens should not be present. These are foreign bacteria that enter the body during infection. The most common pathogens detected are sexually transmitted diseases.
If a particular pathogen is detected, the doctor prescribes or adjusts a treatment regimen for the infection. When you receive the result, show it to your doctor.
Indications for the study
Reproduction in the intestines of opportunistic and pathogenic (pathogenic) bacteria is rare and asymptomatic. A shift in the balance of the flora is accompanied by:
- stool disorder (diarrhea);
- heaviness in the epigastric region and nausea;
- reflex release of stomach contents (vomiting);
- subfebrile (37–38 °C) and febrile (38–39 °C) body temperature;
- acute pain in the abdomen.
The presence of such symptoms is a direct indication for laboratory diagnosis of the state of the intestinal microflora. And also a stool test for UPF is prescribed:
- after contact with a potential source of infection (a person diagnosed with an intestinal infection);
- to differentiate the pathogen and select the most effective drug;
- as a control of ongoing therapy for intestinal diseases;
- within the framework of the medical commission for employment in catering establishments and medical institutions.
Upon admission to some preschool and educational institutions, an analysis of the UPF is carried out along with a mandatory coprogram. An imbalance in the ratio of harmful and beneficial bacteria in the intestines, otherwise dysbiosis is especially often detected in young children. Examination of stool for opportunistic flora is one of the most popular in pediatric practice.
To whom and when is semen culture prescribed?
Indications for bacterial culture of sperm are:
- acute and chronic infectious, inflammatory pathological conditions of the genital organs of any origin (urethritis, prostatitis, sexually transmitted diseases, etc.);
- detection of STI infections in a partner;
- violation of ejaculation, erection;
- pain, discomfort during sex, urination;
- prolongation of the time of ejaculation during sexual intercourse;
- a small amount of sperm during orgasm or its complete absence;
- peeling, itching, rashes, blisters, ulcers on the skin of the groin area, genitals, mucous membrane;
- discharge from the urethra;
- assessment of ongoing treatment.
The benefits of the test or why you shouldn’t avoid it or refuse to take it
In andrology, the main method for diagnosing seminal fluid is a spermogram. If elevated leukocytes are detected in it, then this is a direct indication for bacteriological seeding of sperm.
Only with the help of tank inoculation can one determine the nature of the pathogen and its quantity. Correct prescription of antibiotics and other anti-inflammatory medications is impossible without culture data.
Laboratory microscopy
Analysis of feces for opportunistic flora reveals the types and quantities of facultative anaerobic bacteria as the cause of intestinal disorder. In addition, the study determines the degree of resistance (resistance) of microorganisms to antibiotics. Such a detailed study helps the doctor choose the most effective drugs and effective treatment tactics.
In total, about twenty species of bacteria are analyzed in stool analysis
Examination of excrement is a bacteriological seeding of biomaterial in special containers, each of which contains a nutrient medium for one or another type of microorganism. The environment provides bacteria with breathing, nutrition and optimal conditions for reproduction. If pathogens are present in the test sample, they begin to actively increase their numbers, forming colonies.
The number of CFU (colony forming units) is counted and the specific active microorganism is identified. An antibacterial test is performed on the grown bacterial colony (assessment of the pathogen's resistance to different types of antibiotics). In parallel, taking into account pathogenic and opportunistic microbes, laboratory technicians assess the composition and number of beneficial microorganisms.
Important! It takes a certain amount of time to grow a bacterial colony. The duration of the study can range from 3 days to two weeks.
The short result may be “positive,” which means an excess of the norm for conditional pathogens or the presence of pathogenic bacteria that should not be in the intestines. A “negative” score indicates the stability of the microflora. In this case, to determine the cause of poor health, the patient is prescribed additional laboratory tests.
If necessary, they are supplemented with hardware and instrumental diagnostic procedures. The detailed result records data about a specific pathogen, that is, the name of the microorganism and the concentration - the number of CFU per milliliter of liquid medium (CFU/ml).
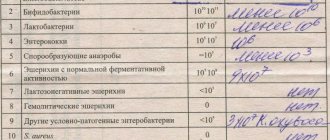
Analysis transcript
Bacteriosis analysis: sample sample
This analysis is carried out over seven days. It is during this period of time that all data on the composition of the microflora of the baby’s feces becomes ready. After receiving the biomaterial, laboratory specialists place it in a special container with a nutrient medium, in which all microorganisms found in the feces germinate. After some time, laboratory staff count germinated bacterial spores per gram of feces and study them in detail using a microscope. Then all data on the number of germinated microorganisms is entered into a special form. The number of germinated bacteria is documented using colony-forming units, based on one gram of the biomaterial under study (COG/g).
To analyze stool, the biochemical method is used, since it is more accurate and requires much less time to complete. A gastroenterologist deciphers the results of the analysis. In his work, he is guided by the norms of age indicators for the child’s body. Submitting biomaterial for analysis in order to identify dysbiosis in a child is a necessary condition for preventing the spread of various pathologies throughout the child’s body. Usually, on the form with the result of the analysis of the child’s feces, there are up to eleven indicators that indicate the presence of certain microorganisms in the child’s intestinal microflora and their number. The results of the analysis contain the following indicators:
- The number of bifidobacteria involved in the digestion of food. In a healthy baby, this indicator ranges from 1011 to 1012 CFU/g of feces.
- The number of lactobacilli that prevent the spread of decay processes in the organs of the digestive system. Normally, this indicator for children is 1011 to 1012 CFU/g.
- Escherichia coli or Escherichia, which are one of the first to settle in the baby’s intestines. Their amount is normally equal to 107 to 108 CFU/g. A decrease in the number of E. coli in the baby’s stool indicates the presence of helminthic parasites in his body.
- The content of bacteroids, necessary for the breakdown of fats and the fight against pathogenic bacteria, in a healthy child ranges from 107 to 108 CFU/g per unit of feces.
- The number of coccal bacterial microorganisms, among which up to five types of different species are distinguished, ranges from 105 to 108 CFU/g per unit of feces in a healthy child. The proportion of clostridia, which belong to the group of neutral microorganisms inhabiting the child’s intestines, should be no more than 105 CFU/g of feces.
- The content of representatives of the Candida genus, which affect the acidity of the baby’s intestinal environment, should be no more than 105 CFU/g of feces in a healthy child.
The reasons leading to a decrease in the number of E. coli are:
- Improper diet and diet, oversaturated with protein, fatty or carbohydrate foods, as well as artificial feeding;
- Taking antibiotics;
- The development of various intestinal infections in the body.
The number of pathogenic enterobacteria that cause the development of various diseases in a child should be minimal or practically absent. The presence of a large number of them in the feces of a child indicates the development of intestinal infections in his body.
Based on these indicators, you can compare the data of your analyzes and independently judge the degree of development of dysbiosis in the child’s body.
Preparation for analysis and collection of biomaterial
To obtain objective results of a stool analysis for UPF, the patient must adhere to specially developed rules. It is recommended to begin preparing the body 2–3 days before collecting biomaterial:
Urine microflora analysis
- eliminate from the diet fried foods, heavy fatty foods, sweets and sweet carbonated drinks, foods that cause intense gas formation (legumes, cabbage, milk and kefir, baked goods, brown bread).
- exclude alcohol;
- stop taking medications: antibiotics, medications that increase intestinal motility, laxative tablets, dietary supplements and medications containing iron, sorbents (Enterosgel, Polysorb, Alcoclean, etc.).
The use of sorbents and antibacterial therapy drugs can destroy part of the intestinal microbiota, which will lead to distortion of the study results. Infants are not allowed to introduce new complementary foods before analysis. A product that is unusual for the body can provoke an allergic reaction and dyspepsia (difficulty digestion).
In this case, the final data on the state of the intestinal flora will be inaccurate, and the analysis will have to be repeated. You cannot use rectal suppositories, microenemas, or oils that can change the microflora. Immediately before collecting biomaterial, it is recommended to carry out a hygiene procedure for the anorectal area (without the use of soap and gel). Preliminary preparation of the container for excrement is of great importance.
You must purchase a sterile container equipped with a special spoon from the pharmacy. For loose stools, use a pipette. Collecting stool in a non-sterile container is prohibited. If foreign impurities enter the test material, the result will be inaccurate. For the same reason, it is not recommended to collect biomaterial from the toilet.
An airtight container with a spoon for submitting excrement for analysis
It would be correct to use a vessel, sheets of paper, and plastic film. When collecting an analysis sample from a baby’s diaper, you need to make sure that no particles of hygienic material get into the container. Women are not recommended to take the test in the first seven days of the follicular phase of the menstrual cycle (the period of bleeding). The container is filled 1/3 full and tightly closed with a lid.
Reliable results are ensured by immediate transportation of the analysis sample to the laboratory. Exposure to high temperatures or freezing makes excrement unsuitable for research. The shelf life of the collected material should not exceed three hours at room temperature and eight hours in the refrigerator.
Norms for the content of intestinal microorganisms
Decoding the analysis of feces for opportunistic flora is carried out by comparing the results obtained with the reference values accepted in laboratory microscopy. The standards for the content of various microorganisms in the intestines are developed taking into account age characteristics - separately for infants up to twelve months of age and separately for adults and children over one year of age.
Reference! Since bacteria are counted in the millions, to make the analysis easier to read and understand, the forms indicate the number 10 and the power (example: 10 to the 6th power = 10^6 = 1,000,000).
Norms of beneficial microorganisms
| Bacteria | bifidobacteria | lactobacilli | coli | enterobacteria | enterococci |
| Babies | ⩾10^10 | 10^6 — 10^7 | 10^7 | 10^4 | 10^5 – 10^7 |
| Adults and children from one year old | ⩾10^9 | 10^7 — 10^8 | 10^8 | 10^5 | 10^5 – 10^8 |
The microflora of infants is influenced by the type of feeding. In breastfed babies, the number of bifidobacteria can reach 10^11. With mixed feeding, the values decrease from 10 to the 6th power to 10 to the 9th power. In artificial people the indicator is 10^8, which is considered normal. The value of bacteroids in children and adults ranges from 10 to the 7th power to 10 to the 8th power.
Standard values for opportunistic pathogens
| Bacteria | peptostreptococci | clostridia | candida | Klebsiella, graphnia, serration, proteus, saprophytic staphylococcus | Staphylococcus aureus |
| Babies | 10^3 – 10^5 | 10^3 | 10^3 | 10^4 | 0 |
| Adults and children from one year old | 10^9 – 10^10 | 10^5 | 10^4 | 10^4 | 0 |
If the number of opportunistic microorganisms does not exceed the permissible values, there is no basis for diagnosing dysbacteriosis. To clarify the cause of the ailment, it is necessary to undergo additional examination. A negative control result obtained after a course of treatment means the patient has recovered.
Reduced levels of beneficial bacteria indicate an imbalance of intestinal flora. The reasons may be:
- unhealthy diet, dieting, fasting;
- chronic diseases of the gastrointestinal tract;
- pathologies associated with congenital (acquired) disorders of enzyme production;
- distress (constant neuropsychological tension).
Taking certain medications can reduce the number of beneficial bacteria. In the form of a normal (negative) analysis for pathogenic intestinal flora, opposite all bacteria of the pathogenic group (Salmonella, Vibrio cholerae, Shigella, Yersinia, enteroviruses) there is a dash or “not detected”, “absent”, “not detected”.
If microorganisms causing infections are detected, the form indicates: “+”, “positive”, or the specific value of the identified microbes is given. If a stool examination reveals pathogens that do not correspond to the normal microflora, but there are no symptoms of the disease, the person is a carrier of the pathogen.
Direct contact with the carrier poses a risk of contagion (infection). A course of chemotherapy treatment, taking antibiotics, or untimely delivery of biomaterial to a medical laboratory can distort the final analysis data for UPF. If the results are unclear, the study must be repeated.
Culture analysis in gynecology
SPECIALISTS Gynecologist Gynecologist-endocrinologist Pediatric gynecologist Mammologist-oncologist Dermatologist Hirudotherapist Intimate plastic surgery Doctor Contour plastic doctor Ultrasound doctor SERVICES AND PRICES Gynecology Mammology Ultrasound diagnostics Paid tests Intimate surgery Contour plastic Treatment for women PROMOTIONS AND DISCOUNTS Students Teams Friends and subscribers am For residents of the region For pensioners Promotions in clinic
Bacteriological culture (bacteriological culture), in gynecology, means a study in which biological material taken from a patient by a gynecologist is placed on a nutrient medium to stimulate the growth of possible microbes. You can take material for bacterial culture from the genital tract, as well as from the oropharynx, urethra and rectum. These tests allow not only to determine the types of microbes that provoke a particular disease, but also to select effective antibiotics (to determine the sensitivity of microflora to them).
CULTIVATION FOR MYCOPLASMA
Mycoplasmas (Ureaplasma urealyticum and Ureaplasma parvum, Mycoplasma hominis) are opportunistic microorganisms. They occupy a leading place among STIs (sexually transmitted infections). Mycoplasma is often combined with gonococci, trichomonas and opportunistic microorganisms; transmitted through sexual contact. Under certain conditions, it can cause urethritis, cervicitis, cystitis, pelvic inflammatory diseases, infertility, as well as pregnancy complications, postpartum and post-abortion pathologies. The result of the analysis of the tank inoculating mycoplasma hominis and ach contains an antibiogram and a conclusion about the amount (concentration) of the microbe found in the material. The result is ready within 7 days.
How to take cultures for mycoplasma: • depending on the indications, women take a smear for culture of mycoplasma from the urethra, vagina, cervix, cervical canal; • in men - a smear from the urethra, urine (in an amount of at least 40 - 50 ml).
CULTIVATION FOR UREAPLASMA
Ureaplasma causes an inflammatory process in the genitourinary system. It is sometimes transmitted through household contact, most often through sexual contact. The incubation period is two to three weeks. In men, the infection manifests itself as urethritis, leading to damage to the testicles and appendages, and ultimately to infertility. In women, ureaplasma causes urethritis, cystitis, and inflammation of the internal genital organs as a complication of vaginal dysbiosis. The procedure for taking a culture test for ureaplasma and mycoplasma is similar for women and men. A culture test for ureaplasma should be taken if PCR smears detect urogenital infections, gynecological diseases, cystitis, or if the presence of Ureaplasma spp. is suspected, for control after treatment (on 10-14 days after discontinuation of antibiotics). Patients often ask the question, what is better to do - PCR or culture for ureaplasma? The fact is that this is a different essence and meaning of culture analysis in gynecology - the first reveals the presence of pathogen DNA, and the second - its clinically significant amount and the degree of susceptibility to antimicrobial drugs. These studies, taken together, will help the gynecologist or urologist choose effective treatment tactics. The results of culture analysis for ureaplasma contain an indication of the presence or absence of growth, and a semi-quantitative assessment is given. The sensitivity of ureaplasma to antibiotics is determined when the result of the search for a microbe in the material delivered to the laboratory is positive.
Interpretation of the result: normally, the culture result for ureaplasma is negative; in case of asymptomatic carriage, bacterial cultures may reveal a low titer (< 104 CFU/ml).
CULTIVATING FOR THRUST
Yeast-like fungi of the genus Candida, the cause of thrush, are one of the most common causative agents of genitourinary tract infections in women. They may be present in small amounts in healthy people. If, for certain reasons, their number increases, this causes the appearance of symptoms of candidiasis such as vaginal discharge, itching, burning, redness, swelling, etc. A culture test for candidiasis allows the gynecologist to identify and assess the degree of presence of Candida fungi and their sensitivity to antifungal drugs. Indications for the study in men and women:
- Presence of symptoms of the disease;
- Selection of antifungal therapy;
- Evaluation of treatment outcome.
CULTURING ON THE INTESTINAL GROUP
The study allows us to identify and differentiate the two most common pathogens of acute intestinal infection - shigellosis (bacterial dysentery) and salmonellosis - a disease caused by the Salmonella species complex. Material: rectal smear.
CULTURING FOR STAPHYLOCOCCUS
Staphylococcus aureus (Staphylococcus aureus) is known as a causative agent of infections in humans. The source is a sick person or a healthy carrier. Routes of transmission: airborne droplets, airborne dust, contact, food. When transmitted through the food route, S. aureus causes foodborne illness (poisoning), characterized by an acute, violent onset, severe intoxication, abdominal pain, and a possible increase in temperature. The material is taken from the rectum, pharynx, and nose. Culture for Staphylococcus aureus is performed to determine the sensitivity of the pathogen to drugs. The test result is ready within 7 days.
SOWING ON LISTERIA
The people most at risk from listeriosis are pregnant women, newborns, and people with immunodeficiency. Transmission of the infection occurs through fecal-oral (consumption of dairy and meat products, poultry products, vegetables and fruits), contact-household, and transplacental (during pregnancy) routes. Indications for taking a culture tank for Listeria: Cultures for Listeria are taken from the cervical canal and vagina, as well as aspirate of the uterine cavity, smear or discharge from the urethra (in women and men).
- Examination of persons with symptoms of the disease living in areas unfavorable for listeriosis;
- Diagnosis of pregnant women before childbirth, with a complicated medical history;
- Testing of persons with immunodeficiency;
- Examination of newborns if there are signs of intrauterine infection;
- Evaluation of the results of therapy.
CULTURING FOR STREPTOCOCCUS
Streptococcus agalactia (hemolytic) is an opportunistic microorganism; in the presence of risk factors, pathologies such as spontaneous abortion, premature birth, chorioamnionitis, pyelonephritis, urinary tract infections, adnexitis and endometritis, endocarditis, sepsis, as well as complications after caesarean section, mastitis and endometritis in postpartum women. A tank culture for streptococcus is taken before the start of antibacterial therapy or no earlier than 7-10 days after its completion. If streptococcus is detected in a throat culture or cervical smear, the test result (Streptococcus agalactiae B) is given in quantitative terms. Cultures for hemolytic streptococci in gynecology are taken from the cervical canal and vagina, throat, pharynx, aspirate of the uterine cavity, smear or discharge from the urethra (in women and men) are examined. The turnaround time for the analysis result is 6-7 days.
Diagnostic features: • taking material from the urethra no earlier than 3 hours after the last urination, • from the cervical canal and vagina - outside of menstruation
See the price of tank cultures in gynecology on this page.
Results
The task of fecal analysis for opportunistic pathogenic flora (OPF) is to determine the qualitative and quantitative content of bacteria that make up the intestinal microenvironment. The studied microorganisms are divided into three groups:
- beneficial aerobic bacteria;
- opportunistic microbes (allowed in limited quantities)
- pathogens (should not be contained in healthy microflora).
In addition to the number of bacterial colonies, the analysis evaluates their sensitivity to antibiotics of various groups. The obtained analysis results are compared with standard values. The norms for children's and adults' indicators differ slightly. In infants up to one year old, the number of beneficial microorganisms depends on the type of feeding (breastfeeding, mixed, artificial).
Therapeutic tactics and medications will be determined by the doctor. Self-medication can lead to complications, especially dangerous for infants. A stool test for UPF is prescribed by a therapist (for children - a pediatrician), a gastroenterologist, or an infectious disease specialist. The accuracy of the results is ensured by compliance with the recommendations for the preparation and collection of biomaterial.