Erosion is the name given to superficial damage to the gastric mucosa, in which the muscle tissue of the organ is not involved in the pathological process. Healing occurs without scar formation. Visually, gastric erosion consists of small areas of defects that vary in shape. Damage can be single, with 1-3 foci, or multiple, with more than 3 foci located in different parts of the stomach. The main danger of erosion is the potential development of ulcers, provoking tumor formations of the colon, pathological changes in the liver, etc. Therefore, at the first suspicion of pathology, you should immediately contact a specialized specialist.
Causes of gastric erosion
- Infection of the mucous membrane (usually Helicobacter pylori);
- various diseases of the gastrointestinal tract;
- unhealthy diet (abuse of hot, spicy, rough foods);
- taking certain medications that have a destructive effect on the walls of the stomach;
- frequent and prolonged stress;
- diseases associated with increased pressure in the vessels of internal organs, disruption of their blood supply;
- systematic entry into the gastrointestinal tract of toxic fumes (usually associated with work in hazardous industries).
Features of drug treatment
Maalox will help treat erosive gastritis.
The choice of treatment method for erosive gastritis directly depends on the causes of its occurrence. If the stomach is affected by Helicobacter pylori, treatment is carried out using antibiotics.
Most often, patients are recommended to take Amoxicillin, Tetracycline, Levofloxacin. The medications are taken over a fairly long period.
If therapy for the disease is interrupted, this will lead to re-production of pathogenic microorganisms.
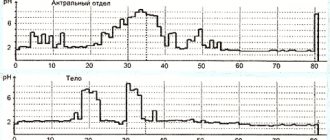
During treatment of the disease, it is necessary to regulate the acidity of the stomach. At this stage of treatment, the mucous membrane is protected from the aggressive effects of gastric juice on it. In order to cure erosive antral gastritis, it is necessary to take antacids and acid blockers.
In most cases, Maalox, Almagel, Rennie, Nizatidine, etc. are taken. Each drug is characterized by its own mechanism of action. That is why, if there is a need to change the medication, it is recommended to first consult a doctor.
If the patient's condition is critical, then he needs to take liquid antacids orally. A high effect in this case is observed with Famotidine, Ranitidine, Cimetidine. If the need arises, treatment is carried out using blood replacement solutions.
Symptoms of gastric erosion
There are acute or chronic forms of the disease. Symptoms of acute gastric erosion usually affect the fundus or body of the stomach. In a chronic process, the antrum is affected (located below all other segments of the organ).
Clinical manifestations of gastric erosion are divided into the following groups.
Ulcer-like. With this clinical picture, the disease is accompanied by severe pain, which usually begins after eating, but can also occur on an empty stomach. Other symptoms are belching, vomiting, heartburn. Ulcer-like symptoms can occur in both acute and chronic gastric erosion.
Hemorrhagic. These are symptoms associated primarily with anemia and bleeding. Often there are no obvious signs of the disease. This course of gastric erosion is characteristic of the acute form of the disease.
Symptoms of pathology
Heartburn is a symptom of erosive gastritis.
Erosive gastritis is accompanied by pronounced symptoms. In most cases, patients complain of a feeling of heaviness in the epigastric area.
When this disease appears, some patients experience heartburn. The patient's mouth usually smells unpleasant. The disease may be accompanied by flatulence and heartburn.
A fairly common symptom of erosive gastritis is bloating in the abdomen. Stomach pain when this disease appears is cyclical. This disease may be accompanied by nausea and vomiting.
Treatment of gastric erosion
The answer to the question “How to treat gastric erosion?” depends on the course of the disease and its symptoms. If therapy is prescribed in a timely and competent manner, healing of the affected areas takes an average of 3 to 7 days. Treatment of gastric erosion can be either inpatient or outpatient. The main reason for hospitalization is bleeding or the threat of bleeding.
If gastric erosion is chronic, first of all, treatment is prescribed for the primary disease against which it developed. In some cases, it may take 2-3 years for the affected areas to heal completely. Typically, therapy involves taking medications that have a targeted effect on eliminating the prevailing symptoms.
- In case of increased acidity, medications are prescribed to prevent the negative effects of hydrochloric acid.
- If the patient complains of nausea and fullness of the stomach, medications are prescribed to correct its motor function.
- If the main cause of the disease is Helicobacter pylori infection, complex therapy is prescribed (antimicrobial agents + drugs that reduce the production of hydrochloric acid).
- In case of bleeding, gastric lavage is performed with ice water and coagulation through an endoscope. If there is excessive blood loss, surgical intervention is necessary.
Only a doctor can accurately diagnose the disease, prescribe treatment and adjust nutrition. To make an appointment, call +7 (495) 223-38-83.
Causes of the disease
Erosive antral gastritis occurs due to the influence of the bacterium Helicobacter pylori.
Most often, erosive gastritis is diagnosed against the background of the negative influence of the bacterium Helicobacter pylori. The location of the disease most often is the antrum of the stomach.
Quite often, single lesions of the mucous membrane are observed. The formation of large areas of necrosis may also be observed.
Against this background, blood vessels are damaged, which leads to bleeding. Neoplasms on the gastric mucosa can appear against the background of:
- Smoking;
- Cancer;
- Burns;
- Stressful situations.
The pathological process quite often develops against the background of diseases of the digestive system of a chronic nature. Erosive gastritis is observed while taking certain medications. These include hormones, anti-inflammatory drugs, and cytostatics. Quite often the disease is diagnosed against the background of alcoholism or one-time consumption of large quantities of alcoholic beverages.
The causes of erosive gastritis are quite varied. In most cases, they depend on a person’s incorrect lifestyle.
Diagnostics
The main method for diagnosing heterotopia of the coolant in the upper third of the esophagus is esophagogastroduodenoscopy (EGD) with biopsy. Unfortunately, heterotopic lesions are often missed during endoscopy because the proximal esophagus is either ignored or skimmed over [15]. This fact probably explains the significant difference in prevalence data obtained from autopsy and endoscopic studies. With endoscopy, areas of the coolant in the proximal esophagus are visualized as round or oval spots of salmon color, velvety appearance, often single, less often paired and multiple. The surface may be smooth or grainy, flat or slightly raised. Infrequently, ectopic coolant is an area of mucosal depression. Most inlet patches are located on the lateral walls, usually a few centimeters distal to the upper esophageal sphincter (16–21 cm from the incisors). Dimensions can vary from microscopic to 3–5 cm (see Fig. 1, 2).
A number of studies show that narrow band imaging (NBI) endoscopy increases the detection rate of heterotopia by approximately 3 times compared with standard white light endoscopy (Fig. 7) [11, 16]. In a study by C. L. Cheng et al. [17], which included 99 patients with heterotopia of the coolant in the upper third of the esophagus, small foci of heterotopia were identified in 54% of subjects using a narrow spectrum versus 17% detected in white light. These results allow us to confidently recommend the use of virtual chromoendoscopy for diagnosing “inlet patch” [16].
S. Blanco et al. [15] proposed using the frequency of detection of heterotopic areas in the proximal esophagus as a criterion for the quality of upper gastrointestinal endoscopy, similar to the adenoma detection rate (ADR) criterion for colonoscopy.
Heterotopia of the gastric mucosa and adenocarcinoma of the esophagus
The most serious issue is to study the relationship between heterotopia of the gastric mucosa and adenocarcinoma of the esophagus. In a systematic review of the literature performed in 2022, M. Orosey et al. [27], a total of 43 cases of adenocarcinoma in the proximal esophagus, arising in the locus of gastric heterotopia, were described; the vast majority of patients were male. The average age of the patients was 63.6±11.3 years. Other authors also demonstrate a low frequency of neoplasia in the “inlet patch” - 0–1.56% [28]. Based on these data, in 2022, the British Society of Gastroenterology and the Association of Upper Gastrointestinal Surgery of Great Britain and Ireland concluded that the inlet patch does not require follow-up and routine biopsy [29]. Most studies show that the risk of malignant transformation of heterotopic gastric mucosa into the esophagus does not depend on age, race, body weight and alcohol consumption; smoking is significant (23.7 pack/years versus 16.3 pack/years, p = 0.006) [30 ]. In 2022, French researchers [31] reported that among patients with an identified mutation of the CDH1 gene, which is associated with a high risk of developing diffuse-type hereditary gastric cancer, an “inlet patch” was detected and morphologically verified in 50%. However, in this group of patients, not a single case of esophageal cancer due to “inlet patch” was recorded [31]. Following this publication, P. Leclercq et al. [24] suggested that an island of columnar cell epithelium in the upper third of the esophagus poses a potential risk for the development of adenocarcinoma in patients who are carriers of the CDH1 gene mutation, including those who have undergone prophylactic gastrectomy, which necessitates a targeted endoscopic examination with collection of histological material from the ectopic coolant in the proximal section of the esophagus [24].
Classification of forms of erosive gastritis
- Primary erosions (have no connection with previously identified pathology) and secondary (the result of progression, existing disease).
- Malignant (appears in the presence of an oncological process) and benign (can be single or multiple).
- Immature (young formations) and mature (have areas of tissue necrosis).
Based on the type and shape of formations on the mucous membrane, the following types are distinguished:
- superficial (small, flat in shape and with a distinct edge);
- full (raised above the surface of the mucosa);
- polypoid (can have a diameter of up to one and a half centimeters, do not heal for a long time and constantly worsen).
How is erosive gastritis diagnosed?
Erosive gastritis has symptoms similar to other gastrointestinal diseases. Therefore, to clarify the diagnosis, additional examination is prescribed. Most often, doctors recommend the following laboratory and instrumental studies:
- a general blood test to determine the presence of anemia;
- determination of occult blood in feces;
- taking a section of the mucosa for cytology and histology;
- PCR for diagnosing Helicobacter pylori infection;
- fibrogastroscopy (FGDS) with a biopsy of the inflamed area;
- radiography with contrast.
Sign up for FGDS
Don't delay treatment
Symptoms of chronic bleeding
Internal stomach bleeding leads to severe anemia
Symptoms of chronic blood loss are vague and depend on the degree of iron deficiency anemia. Often the body compensates for losses so well that the patient walks independently and lives a normal life with a hemoglobin level of 30-40 g/l. The main symptoms of chronic gastric bleeding are signs of anemic syndrome. Severe weakness and fatigue appear, which increases even from slight physical activity.
The condition of the skin changes: the skin is pale, dry, flaky, and “stubs” appear in the corners of the mouth. Women immediately notice brittle nails and cracks in the skin of their hands.
With severe anemia, patients feel tachycardia even at rest, and shortness of breath appears. The condition of the oral cavity changes - there is a burning sensation in the tongue, difficulty swallowing, redness of the tip of the tongue. Sometimes there is hoarseness, coughing, redness and itching in the palate.
In especially severe cases, olfactory tastes change - patients may fall in love with the musty air of the basement, the smell of shoe polish or car tires. Sometimes there is a desire to eat sand or earth.
Methods for collecting biomaterial
The purpose of a biopsy is to collect material (biopsy) for subsequent study. This can be done by 2 methods - surgical and endoscopic.
During surgery, the removed tissue is sent to the laboratory. A doctor examining it under a microscope makes a conclusion. The operation is resumed, if necessary, with adjustments.
One common method is endoscopy. Here they use a fiberscope, a flexible probe with a camera and an LED flashlight. This type of biopsy is called a targeted biopsy, where the doctor uses a control unit to control the movement of the fiberscope. Targeted biopsy significantly reduces risks.
Contraindications
All existing contraindications are included in 2 groups - absolute and relative.
The first include:
- Narrowing of the lumen of the esophagus, preventing the movement of the endoscope;
- Acute somatic diseases;
- Aortic aneurysm.
Indicators of the second group:
- Inflammation of the nasopharynx;
- Fever;
- Hypertensive crisis;
- Poor blood clotting;
- Epilepsy;
- Mental illnesses, some others.
Biopsy examination
A piece of tissue taken for analysis is placed in a special container and sent to the laboratory. In it, the biopsy specimen is fixed in formalin and embedded in paraffin or frozen.
Next, sections of the biopsy are taken and placed on a glass slide; after staining and drying, a microscope is used for examination.
The conclusion stated:
- Characteristics of epithelial tissue;
- Thickness of the mucous membrane;
- Epithelial dysplasia or metaplasia;
- Features of inflammation;
- Mutated cells, their characteristics and localization;
- Spiral gram-negative bacterium;
- Contamination level.
Stomach cancer may be indicated by:
- Cell shape;
- Their sizes;
- Size and fragmentation of nuclei;
- The presence of several cores;
- Pathologies in the cytoplasm.
As a rule, the results of the study are ready ten to fourteen days after it is conducted. If the biopsy is urgent - on the same day, but the probability of error is higher.
Medicines for ulcers and gastritis
Therapy for these diseases should be prescribed by a doctor, taking into account the existing symptoms. These pathologies are interrelated, so the drugs for their treatment are similar. Most often, their action is aimed at neutralizing H. Pylori. Tablets prescribed for abdominal pain can be divided into 4 categories.
Antibiotics
Gastroenterologists carefully select antibiotic treatment. It is necessary to compare the risks of side effects and the beneficial effect. Most often, a two-week course of antibiotic therapy is the only way to eradicate H. Pylori.
| CLARITHROMYCIN TAB. P/P/O 250MG No. 14 |
| AMOXICILLIN CAPS. 250MG No. 16 |
| AMOXICILLIN CAPS. 500MG No. 16 |
| AMOXICILLIN TAB. 500MG No. 20 |
| METRONIDAZOLE TAB. 250MG No. 40 |
Proton pump inhibitors
The action of these medications is aimed at blocking the release of bile acid, which accelerates the healing of ulcers.
Do not forget that using inhibitors in large dosages for severe stomach pain is too risky. Leukopenia, nervous disorders, and myalgia are highly likely to develop.
| OMEZ DSR CAPS. MODIF. HIGH 30MG+20MG No. 30 |
| OMEZ CAPS. 20MG No. 30 |
| OMEZ CAPS. K/R 10MG No. 10 |
| OMEZ CAPS. K/R 40MG No. 28 |
| OMEPRAZOLE CAPS. 20MG No. 30 |
| EZOMEPRAZOLE TAB. K/R P/O 20MG No. 28 |
| EZOMEPRAZOLE-SZ CAPS. K/R 40MG No. 28 |
| OMEVEL CAPS. K/R 20MG No. 30 |
H-2 histamine receptor blockers
Their action is aimed at reducing acid production in the stomach. Under the influence of drugs, acid is formed in minimal quantities, which does not allow the ulcer to grow.
| RANITIDINE TAB. P/P/O 150MG No. 30 |
Antacids
They neutralize stomach acid, reducing pain. But experts emphasize that antacids quickly eliminate pain without getting rid of its cause. That is, these drugs do not promote healing of ulcers. In addition, they are often produced in the form of suspensions, which can cause nausea, vomiting, and constipation.
| PHOSPHALUGEL GEL FOR ORAL TAKEN 16G No. 20 |
| ALMAGEL A SUSP. D/ORAL 10ML No. 10 |
| ALMAGEL A SUSP. FOR ORAL USE 170ML COMPLETE WITH MEASURING SPOON |
| MAALOX SUSP. D/ORAL 15ML No. 30 |
| MAALOX SUSP. D/ORAL 15ML No.6 |
| MAALOX SUSP. D/ORAL 250ML |
| MAALOX TAB. CHEW. №10 B/SUGAR |
| MAALOX TAB. CHEW. No. 20 |
| GASTAL TAB. D/RASSAS. No. 12 |
| GASTAL TAB. D/RASSAS. No. 12 MINT |
| GASTAL TAB. D/RASSAS. No. 30 |
| GASTAL TAB. D/RASSAS. No. 60 |
| RENNIE TAB. CHEW. 680MG+80MG No. 12 ORANGE |
| RENNIE TAB. CHEW. 680MG+80MG No. 24 ORANGE |
| RENNIE TAB. CHEW. 680MG+80MG №24 MENTHOL |
| RENNIE TAB. CHEW. 680MG+80MG No. 48 ORANGE |
| RENNIE TAB. CHEW. B/SAKH. 680MG+80MG No. 12 MINT |
| RENNIE TAB. CHEW. B/SAKH. 680MG+80MG No. 48 MINT |
| GAVISCON DOUBLE ACTION SUSP. FOR ORAL USE 10ML No. 12 MINT |
| GAVISCON FORTE SUSP. D/ORAL 10ML No. 12 D/PREGNANT. MINT |