An intestinal biopsy is one of the most informative ways to find out what changes are occurring in its mucosa. Histological examination allows not only to make an accurate diagnosis, but also to determine subsequent treatment tactics. Intestinal pathology can be diagnosed in both adults and children, but often symptoms and laboratory data are not enough. In such cases, a biopsy comes to the rescue - a histological analysis of the mucous membrane of the small or large intestine. Tissue for examination is obtained during intestinal endoscopy. The widespread use of intestinal biopsy as a valuable diagnostic method became possible not only thanks to the invention of the microscope. For a long time, only superficial tissues could be subjected to microscopy, and internal organs were examined only during open operations. The introduction of endoscopic technology and the improvement of methods of minimally invasive interventions have made it possible to make non-surgical intestinal biopsy a screening measure available to a wide range of patients. In cases where microscopy of the mucous membrane does not provide a complete answer to the questions of interest, pathomorphologists conduct additional immunohistochemical examination of a tissue sample, including the determination of disease-specific or a type of malignant tumor of proteins in intestinal cells. Colonoscopy or fibrogastroduodenoscopy with biopsy is carried out if indicated, as well as during routine preventive examinations. People of both sexes are at risk, starting from the age of 40. The older the subject, the more likely it is that the biopsy will show at least some abnormality. The procedure is prescribed by therapists, gastroenterologists, and proctologists. Taking an intestinal biopsy is not the most pleasant event, but you can reduce not only the likelihood of complications, but also minimize subjective discomfort by properly preparing both physically and psychologically.
Preparing for a biopsy
When performing a biopsy of the small intestine, you should refrain from eating 8-12 hours before the scheduled test. Preparation for a colon biopsy includes a slag-free diet for 3 days and the use of cleansing enemas (with a syringe or Esmarch mug) or special cleansing drugs (Fortrans, Endofalk) according to the regimen prescribed by the doctor. The day before the biopsy, you are allowed to drink broths, juices and water. On the eve of the test, you can only drink juices and water.
What else is prescribed with this study?
Histological examination of the gastrointestinal tract (biopsy material)
15.34. 3 days
3 days
2 900 ₽
Add to cart
Histological examination of the gastrointestinal tract (surgical material)
15.34.1. 3 days
3 days
2 900 ₽
Add to cart
Immunohistochemical examination of the gastrointestinal tract (biopsy/endoscopic material)
29.51. 7 days
7 days
11 000 ₽
Add to cart
Immunohistochemical examination of the gastrointestinal tract (surgical material)
29.25. 7 days
7 days
13 000 ₽
Add to cart
Multifocal gastric biopsy with OLGA classification
15.59. 3 days
3 days
4 410 ₽
Add to cart
Biopsy procedure
Small intestine
Most often, biopsy material is taken from the duodenum. Other parts of the small intestine are difficult to access for material collection. Before starting the procedure, the patient gives written consent to it. The progress of the study and possible complications are explained to him. They warn about the body’s reactions to the insertion of the endoscope (strong salivation occurs, which should not be prevented and you should not try to swallow saliva, the release of gas afterward, gagging, etc.).
- Half an hour before the test, a sedative is given, which allows the person to relax, but not fall asleep. During a biopsy of the upper small intestine (duodenum), the patient is conscious.
- Before inserting the fibroendoscope, the back wall of the pharynx is irrigated with an anesthetic to reduce the gag reflex. The anesthetic has a bitter taste and creates a feeling of swelling in the throat.
- A mouthpiece is inserted into the mouth to prevent the person from accidentally biting through the endoscope tube. The mouthpiece does not interfere with breathing.
- The person is placed on his left side and an endoscope is inserted through the mouth. Under visual control, the doctor reaches the desired area.
- The endoscope has a biopsy channel through which forceps are inserted and the desired area of tissue is grasped. Afterwards, the forceps with the biopsy material are removed.
- The biopsy is placed in a special prepared container with a solution and sent to the laboratory.
- The doctor checks for bleeding or perforations at the biopsy site and removes the endoscope.
- Taking a biopsy takes about 30 minutes. The procedure is more unpleasant than painful. When the endoscope passes through the initial parts of the digestive tract, the gag reflex is irritated, which causes unpleasant vomiting.
The procedure is more unpleasant than painful. When the endoscope passes through the initial parts of the digestive tract, the gag reflex is irritated, which causes unpleasant vomiting.
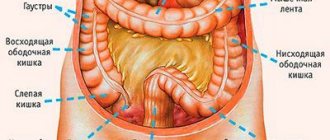
Colon
A biopsy of parts of the large intestine is performed using colonoscopy or sigmoidoscopy. Before the procedure, the patient gives written consent to it. The doctor explains the progress of the study and possible complications.
- The patient is placed on his left side with his legs brought to the stomach.
- Before the study, blood pressure and pulse are measured. They give sedatives to calm you down or anesthesia.
- Lubricate the tip of the colonoscope with Vaseline for better advancement and insert it through the anus.
- As the colonoscope advances, air is pumped in to better straighten the intestinal loops.
- When the colonoscope has reached the sigmoid colon, the person is turned on his back and the examination continues further.
- In the desired area of the intestine, tissue is collected using forceps.
- The resulting material is placed in a special container and sent to the laboratory.
- After checking for bleeding from the site where the biopsy material was taken, the colonoscope is removed.
Taking a biopsy from the large intestine is a painful procedure, so in most cases it is performed under anesthesia at the request of the patient.
How is diagnostics carried out?
In order for a colonoscopy with biopsy to be informative, it is necessary to properly prepare for the study. For this purpose, a few days before the study, the patient is prescribed a diet - foods that provoke the formation of gases and increase the volume of stool are excluded. Preparation also includes cleaning the intestines from feces. To do this, the day before they take special medications that have a laxative effect. Doctors at the Euroonko clinic use the drug Fleet Phospho-soda. It has a local effect and is designed specifically to prepare the patient for endoscopic examination.
Colonoscopy with biopsy is performed in the side lying position with the legs tucked to the chest. Depending on the scope of the study, the procedure may have some features:
- If a full colonoscopy with a biopsy of the colon is planned, the patient is first put into a medicated sleep. The area around the anus is then treated with an antiseptic solution, and the doctor carefully inserts the tip of the colonoscope into the rectum.
- In some cases, the study is not carried out in full. If you need to limit yourself to diagnosing the rectum or sigmoid colon, then intravenous anesthesia is not always advisable to use. In this case, a local anesthetic gel is used to reduce discomfort from the procedure.
To make the intestinal walls straighten and be accessible for visual inspection, gas is injected through the colonoscope. A more modern version of the study involves the use of carbon dioxide (CO2) to fill the intestines, since this procedure is easier to tolerate. This option is used when performing colonoscopy at the Euroonko clinic.
Depending on the features described above, the duration of a colonoscopy with biopsy can vary from 15 minutes to an hour. The maximum duration is observed in cases where it is necessary to perform therapeutic manipulations, for example, to remove a polyp or stop bleeding. The study can also be delayed when it is necessary to take a biopsy from several areas located at a great distance from each other.
After a colonoscopy with biopsy, the patient is taken out of medicinal sleep and remains under the supervision of doctors for some time, after which he can leave the clinic.
In what cases is a biopsy prescribed?
An intestinal biopsy must be performed in the following cases:
- tumor formation detected by CT, MRI, colonoscopy or other identification studies;
- multiple erosive and ulcerative processes in the intestines;
- long-term inflammatory processes of unknown etiology;
- intestinal symptoms (changes in stool, blood in the stool, flatulence, etc.) that do not fit into the clinical picture of common diseases and require a more thorough examination
Detailed description of the study
Colon cancer is a malignant cancer that develops in the lining of the large intestine. This tumor is also called colorectal cancer (CRC), combining the name for malignant lesions of the colon and rectum. Colon cancer is widespread in Russia and throughout the world - about 9-10% of all oncological pathologies are accounted for by this type of neoplasm.
The main, so-called “precancerous” diseases of colorectal cancer include:
- Colon polyps: in most cases they are asymptomatic, and bleeding from the rectum may be observed;
- Ulcerative colitis: attacks of diarrhea mixed with blood and cramping pain in the lower abdomen, which are followed by an asymptomatic period;
- Crohn's disease: chronic diarrhea, abdominal pain, fever, anorexia, weight loss.
Patients with the above pathologies have the highest risk of developing colon cancer. The following clinical picture is often characteristic of CRC:
- Long asymptomatic period (due to long tumor growth);
- General weakness, unmotivated fatigue;
- Abdominal pain (colic type);
- Stool mixed with blood;
- A large tumor can be detected by palpation of the abdomen.
For screening purposes - early diagnosis - of cancer, it is advisable to perform a colonoscopy - an endoscopic examination of the colon. If a pathological area is detected, the endoscopist can send a sample of it for histological examination (histology).
Histological, or pathomorphological, examination in detecting colon cancer is one of the main and most reliable diagnostic methods. The result of histology allows us to determine the nature of the tumor disease and assess the degree of malignancy of the above precancerous conditions.
Material for research is taken during colonoscopy using multifocal biopsy - a procedure during which the doctor uses endoscopic forceps to collect tissue from the large intestine in different areas, usually 3-5. This number of samples is necessary for a more accurate histological assessment of the material, since colorectal cancer can have a different morphological structure and degree of differentiation. The resulting biomaterials are formed into microslides for further microscopy. The result of histology allows us to determine the following important morphological characteristics:
- Tissue origin of the tumor (histogenesis);
- Tumor size;
- The degree of differentiation, or malignancy, of the neoplasm;
- Condition of the proximal and distal resection margins: whether tumor growth continues in them;
- The number and condition of the neighboring lymph nodes examined: whether there is metastasis;
- The presence of invasion - germination - tumors into nerve fibers or into adjacent blood/lymphatic vessels;
- Assessment of the effectiveness of previous therapy using the Mandard and Dworak scales.
Based on histological examination, the pathomorphological stage of colon cancer is established, as well as the degree of inflammatory infiltration of ulcerative colitis and Crohn's disease. The histological report allows the attending physician to assess the prognosis of the disease and select or change the treatment plan.
Indications and contraindications
The examination can be planned in advance in case of malignant tumors, ulcerative changes that are difficult to respond to medications, an unclear diagnostic picture, or if the person has complaints.
A biopsy is indicated for:
- suspected ulcer degeneration;
- polyps;
- erosion;
- scar changes;
- identifying Helicobacter;
- excluding celiac disease in children.
Contraindications are absolute and relative. The absolute ones include:
- acute severe conditions (myocardial infarction, stroke);
- decompensated somatic diseases (hypertension, respiratory, renal failure);
- stenosis and varicose veins of the esophagus;
- displacement of mediastinal structures due to neoplasms, aortic aneurysm.
Severe conditions, including those of the blood coagulation system, that can be corrected may be relative. In such cases, a biopsy is possible after corrective therapy.
References
- Chissov, V.I. Oncology: National Guide. Brief edition / ed. IN AND. Chissova, M.I. Davydova. - M.: GEOTAR-Media, 2022. - P. 297-307.
- Cancer of the colon and rectosigmoid. Clinical recommendations. Association of Oncologists of Russia, 2022. - 45 p.
- Kuipers, E., Grady, W., Lieberman, D. et al. Colorectal cancer. Nat Rev Dis Primers, 2015. - Vol. 1.
- Kagueyama, F., Nicoli, F., Bonatto, M. et al. Importance of biopsies and histological evaluation in patients with chronic diarrhea and normal colonoscopies. Arq Bras Cir Dig., 2014. - Vol. 27(3). — P. 184-187.
- Bateman, A., Patel, P. Lower gastrointestinal endoscopy: guidance on indications for biopsy. Frontline Gastroenterol., 2014. - Vol. 5(2). —P. 96-102.