Constipation is a common problem in childhood; it is usually associated with the child’s diet and goes away after some time. But if difficulty in defecation occurs regularly, you should take this problem more seriously. This manifestation is a symptom of a number of diseases. Dolichosigma is one of these pathologies.
Dolichosigma is a structural abnormality of the sigmoid colon. With this pathology, the sigmoid colon lengthens, but its lumen does not change in diameter, and the walls do not become thicker.
About the intestines
The intestine consists of the small and large intestines. They help your body absorb nutrients from the food and drinks you eat.
- The small intestine absorbs carbohydrates, proteins, fats, vitamins and minerals. It is about 15–20 feet (4.5–6 meters) long and divided into 3 sections. The first section is the duodenum, the second is the jejunum, and the last is the ileum. Each department plays its own special role in the digestion and absorption of nutrients.
- The large intestine absorbs water and minerals. It is about 5 feet (1.5 meters) long.
Once part of the intestine is removed, the remaining part can adapt. This means that the remaining part begins to absorb nutrients and fluids that would normally be absorbed by the removed part. This means that parts of your intestines can be removed without serious consequences to your body's nutrition.
However, the remaining intestines take time to adapt. For some time after surgery, your body may not absorb nutrients, fluids, vitamins, and minerals as well as it did before surgery.
to come back to the beginning
Reasons for the development of dolichosigma
The exact reasons for this anomaly have not yet been identified. Sometimes congenital pathology is the result of exposure to radiation, toxins, and various chemical and physical factors during fetal development. Dolichosigma can also develop if a woman has an infectious disease during pregnancy. The correct development of the fetus can be disrupted by the use of certain medications by a pregnant woman.
Acquired dolichosigma rarely appears in children. The reasons will be the following:
- long-term constipation, processes of fermentation and putrefaction in the intestines after prolonged dysbiosis or prolonged infection, frequent food poisoning;
- disturbance of intestinal motor activity due to a sedentary lifestyle;
- excessive consumption of meat products, carbohydrate diet;
- persistent nervous tension and stress.
Dietary recommendations
Follow these guidelines as your gut heals. You can also use the sample menus at the end of this material.
Eat 6–8 small meals a day
Eating small meals frequently will reduce the strain on your shortened intestines. Eating small portions of food helps control symptoms, and small portions are easier to digest and absorb into the body.
- Eat slowly and chew your food thoroughly.
- Once your gut adjusts, you can go back to eating 3 meals a day.
Drink no more than ½ cup (4 oz (120 ml)) of liquid at each meal
Drinking plenty of liquid with meals speeds up the passage of food through the intestines. This means that food may not be digested and nutrients may not be absorbed.
- Drink most liquids between meals, at least 1 hour before or 1 hour after meals.
To aid recovery, include adequate amounts of nutrients in your diet.
Your food should be:
- Rich in proteins. Protein-rich foods include: Poultry (chicken, turkey) Meat (beef, pork, lamb)
Fish - Eggs
- Tofu cheese
- Dairy products (milk, cheese)
- Smooth peanut butter and other nut butters such as almond
- Rich in refined or complex carbohydrates with low fiber content (starches). Examples of such fruits:
- White bread
- Breakfast cereals such as Rice Krispies® and Corn Flakes
- Potatoes without skin
- White rice
- Pasta
butter; |
|
|
For example, eating toast with butter or a sandwich with mayonnaise is fine, but it's best to avoid foods that are too fatty, such as deep-fried foods.
If you have had a large section of your ileum removed, you may be better off eating a high-fat meal for breakfast rather than later in the day.
- Low in sugar. Examples of foods high in sugar:
- Sweets (cookies, cakes, candies, chocolate, soda, instant teas, fruit drinks)
Corn syrup
- Syrup
- honey;
- Pancake syrup
You can use artificial sweeteners such as Splenda® or Sweet N'Low®. However, limit your intake of sugar-free candy or cough drops that contain sugar alcohols such as sorbitol, xylitol, mannitol and isomalt. Consuming them in large quantities can have a laxative effect (lead to bowel movements).
Include enough liquid in your diet
- Try to drink at least 8 glasses (8 ounces (240 ml)) of fluid per day.
- Avoid very hot or cold drinks.
- Choose drinks that don't contain a lot of sugar. This will prevent dehydration. These drinks include water, coffee, tea, milk or juices diluted with water. Be careful—coffee may have a laxative effect for some people.
If you are lactose intolerant, eat a low-lactose diet
Sometimes removing part of the intestine can cause lactose intolerance.
Lactose is a sugar found in dairy products. It can cause symptoms such as gas, colic and diarrhea. Such symptoms usually begin to appear within the first 30 minutes after consuming dairy products.
- To test if you can tolerate lactose, drink ½ cup of milk. If you experience any symptoms, try lactose-free dairy products, such as Lactaid® milk or almond, rice or soy milk. You can also take Lactaid® tablets or Lactaid® drops before consuming dairy products to help with dairy digestion.
- Some foods have lower lactose content than others. If you can't drink milk, try plain yogurt and mature cheeses (like hard cheeses like cheddar or Swiss). If you can eat it, try soft cheeses (like cream cheese or cottage cheese). If you still have symptoms, you can eliminate all dairy products for 1-2 months and then try eating them again.
Eat a low-oxalate diet
If you have had your ileum removed and have an intact colon, you should eat a low-oxalate diet. Oxalate is a substance found in many foods that can cause kidney stones. Avoid foods and drinks high in oxalates, such as:
|
|
|
|
If necessary, your doctor or dietitian will discuss this diet with you.
to come back to the beginning
Diagnostics
Correct diagnosis is important to determine effective treatment.
Numerous research methods are used to diagnose the disease.
Taking a life history and physical examination of the patient
During the interview, the doctor must obtain the following information about the patient:
- diet and diet;
- degree of exposure to stress;
- intensity of neuropsychic stress;
- information about the immunization performed;
- data on previous illnesses and food poisoning;
- information about concomitant diseases and allergic reactions;
- time of appearance of the first symptoms and the nature of their manifestation;
- subjective feelings and complaints at the moment;
- factors that alleviate or aggravate the condition;
- information about the treatment undertaken and medications taken.
The specialist then examines the patient. The abdomen, intestines and area of the sigmoid colon are carefully palpated. Percussion tapping is carried out on the areas where the compaction is found. Using the method of auscultation, sounds observed in the intestine are heard, this will allow one to determine the approximate direction of the dynamic processes occurring in the intestine.
The information obtained will allow you to make an approximate diagnosis. To confirm it, additional instrumental and laboratory studies should be carried out.
Laboratory research
A number of tests must be performed to make a diagnosis. In general blood and urine tests, you can see signs demonstrating the stage and nature of the pathology: the presence of inflammation, infection, intoxication. Biochemical analysis will show the characteristics of metabolism and the main processes occurring in the body. A stool occult blood test will reveal internal diseases. The presence of blood hidden in feces may indicate the presence of cancer at an early stage.
The coprogram provides information about the quality of food digestion. Examination of feces for helminth eggs is also mandatory. Analysis for dysbacteriosis is carried out if necessary.
Use of instrumental research methods
The results of instrumental methods will allow us to make a final diagnosis.
Only irrigography can detect an increase in the length of the sigma. Before starting the procedure, a barium enema is administered.
Ultrasound can be used to examine intestines clogged with dense feces. It is impossible to perform a CT scan on young children because they cannot remain motionless for a long time.
Using a thin pediatric probe, a colonoscopy is performed under short-term anesthesia, if necessary for differential diagnosis. This procedure makes it possible to examine the colon and assess the degree of damage to the mucosa.
To prepare a child for the study, it is necessary to give him a laxative and perform a cleansing enema.
Cellulose
After surgery, your body may have a hard time digesting fiber, especially insoluble fiber. Insoluble fiber is found mainly in whole grains and bran. It does not break down in water, so your body will not be able to break it down, and your stool (feces) will become bulkier because of it.
Soluble fiber is generally better tolerated because it breaks down in water and can be broken down by your body. It also helps slow down digestion. Soluble fiber products include:
|
|
|
*Before taking any fiber supplements, consult your doctor.
Many foods contain both soluble and insoluble fiber. Please refer to the list below.
| Products that are recommended to be included in the diet | |
Soluble fiber foods such as:
| Low fiber foods such as:
|
| Foods that should not be included in the diet | |
Insoluble fiber foods such as:
| Difficult to digest foods such as:
|
to come back to the beginning
Features of dolichosigma in young children
A child with dolichosigma becomes lethargic, capricious, cries all the time and refuses to eat. The main symptom is constipation with gradually increasing frequency. This is usually due to the transition to mixed feeding or the introduction of complementary foods, which entails a change in the consistency of stool and an increase in its quantity.
Most affected children have functional disorders of other parts of the gastrointestinal tract: diverticular disease, colitis, dysbacteriosis, pancreatitis, biliary dyskinesia, chronic gastroduodenitis, etc.
Stages
There are three stages of abnormal elongation of the sigmoid colon.
| Stage name | Characteristic |
| Compensatory | Constipation occurs periodically for about 3 days. There may be abdominal pain. Following a special diet and taking mild laxatives will help restore evacuation functions. |
| Subcompensation | Persistent constipation occurs in combination with abdominal pain and severe flatulence. It is impossible to restore evacuation functions with laxatives. Bowel emptying is achieved by using a cleansing enema. |
| Decompensation | Constipation lasts more than a week. There is severe pain in the abdomen. Fecal impaction causes an increase in the size of the large intestine. Intoxication develops, loss of appetite occurs, nausea and a general feeling of malaise appear. An exclusively siphon enema will help empty the intestines. In advanced cases, intestinal obstruction and complications develop. |
The sigmoid colon often increases in length even in childhood, and the stable progression of the disease over time leads to severe complications.
Colonoptosis
This is a prolapse of the transverse colon.
Occurs most often as a result of a defect that developed in utero. It is characterized by stagnation of fecal matter, persistent constipation, and nausea and vomiting. The pressure can damage the bladder. More often the right side becomes inflamed, but adjacent organs are involved in the inflammatory process. Without treatment, intestinal obstruction develops.
Colitis
This is an inflammation of the intestinal mucosa. With dolichosigma, colitis occurs against the background of many days of absence of stool, since fecal matter does not pass out and accumulates in the intestine. All this leads to the production of toxins, the development of intoxication, and irritation of the intestinal walls. The mucous membrane swells, hyperemia occurs (excessive blood flow into the vessels of the organ), and irritation occurs. The feces become dark in color and have a foul odor.
Dolichocolon
With this pathology, the large intestine lengthens along its entire course. The walls of the organ expand and thicken.
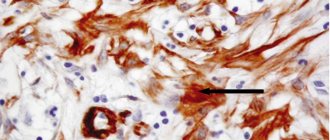
Manifestations include chronic stagnation of feces, intoxication of the body, irritation of the walls of the organ. As a result, inflammation develops. Over time, fibrosis occurs (thinning of the mucous membrane and its replacement with connective tissue). The depth of damage increases, the muscle layer, submucous membrane and nervous tissue are affected.
Constipation for more than 3 days, pain and spasms are the first signs of pathology.
Vegetables
You may have trouble digesting raw vegetables after surgery. Start by eating small amounts (½ cup) of well-cooked vegetables from the “Typically Well Digested” column in the table below. Chew them thoroughly. If you can tolerate cooked vegetables well, you can try raw vegetables in small quantities.
Avoid vegetables that cause gas or discomfort.
| Usually well absorbed | May cause gas or discomfort |
|
|
to come back to the beginning
Vitamins and mineral supplements
You may now not eat some foods that you ate before surgery. To get all the vitamins and minerals you need, you may benefit from taking 1 multivitamin tablet per day. Multivitamins should contain the recommended daily dose of vitamins and minerals.
You may need to take specific vitamins or minerals. Ask your doctor or nutritionist what you should take. Examples of such fruits:
- Vitamins A, D, and E You may need to take vitamins A, D, and E in water-soluble form. This is a rare occurrence and only occurs when a large portion of the ileum is removed.
- If you have had the end of your ileum removed, you will need vitamin B12 injections every 1 to 3 months.
- You may need extra calcium, especially if you have had most of your ileum removed but most of your colon remains intact.
- With excessive diarrhea, potassium levels may decrease. Ask your doctor if you should eat potassium-rich foods. These include oranges, potatoes, tomatoes and bananas.
- If you have a lot of diarrhea, ask your doctor whether you should take a zinc supplement.
Oral rehydration solution
- If you have a lot of diarrhea, your doctor may recommend that you drink an oral rehydration solution. This will replenish the fluid, sodium and potassium that leaves your body in stool.
- You can purchase an oral rehydration solution (such as Hydralyte®) at your local pharmacy without a prescription, or you can make your own. This is not the same as sports drinks (like Gatorade®), which do not contain the same amount of nutrients.
Liquid food additives
- If you are losing weight, high-calorie liquid nutritional supplements may help. However, depending on your surgery, some supplements may not be suitable for you. The main reason for this is the high sugar content.
- Your doctor or nutritionist may recommend a special low-sugar supplement whose ingredients are "pre-digested" and therefore easier to digest. He may also recommend medium chain triglycerides (MCT), a type of fat that is easily digested for extra calories. Always consult your physician before taking supplements.
- If you can eat or drink dairy, try the fortified milk recipe. It will increase the amount of calories and protein in your diet.
to come back to the beginning
Fortified milk recipe
- Mix 1 quart (4 cups (1 L)) milk with 1⅓ cup (320 ml) instant milk powder (usually 1 packet).
- You can use any milk (such as whole, 2 percent, 1 percent, skim or Lactaid®).
- Mix the ingredients thoroughly.
- Store in the refrigerator.
This will make about 4 servings of fortified milk.
Nutrition Facts per 8 oz (240 ml) serving when mixed with:
- whole milk: 230 calories, 16 grams protein;
- 2 percent milk: 200 calories, 16 grams protein;
- 1 percent milk: 180 calories, 16 grams protein;
- skim milk: 160 calories, 16 grams protein.
to come back to the beginning
Tips for keeping a food diary
Keeping a food diary is a good way to find out which foods suit you best. Keep a food diary, recording the following information:
- the time you ate, snacked or drank drinks;
- name of the product or drink;
- the amount of food or drink consumed;
- any symptoms you experience.
If you have had an ileostomy or colostomy, it is also useful to record the amount of discharge from your stoma. Measure the amount of stool in the receiver over 1 week. Measure it every time you change or empty the receiver. Later, if this amount is approximately the same every day, measure it once a month for 1-2 days. Record the amount of discharge and bring this information with you to appointments.
If you notice changes in stool consistency, measure the amount more often and tell your doctor.
to come back to the beginning
Menu (Power Mode)
The main rule of nutrition is to avoid overeating, so you should have several snacks throughout the day. Eating a large amount of food at night will only make the situation worse. Also remember that you need to consume 25-30 g of dietary fiber daily (their content in 100 g of product can be found on the websites). Do not forget about taking juices with pulp, water with honey, prune infusion, and dried fruit compote on an empty stomach.
Wheat bran is an effective remedy, but you need to take it, gradually increasing the amount until it produces an effect. Start taking it with a teaspoon 2-3 times, 20 minutes before meals, with 100 ml of liquid. Bran should swell in the gastrointestinal tract, so you should not fill it with water or add it to kefir or soup. After 5 days, the dose of bran is increased by 2 times, eventually brought to 1-2 tablespoons. When introducing bran, maintain a drinking regime; this is very important, since bran can cause constipation if you do not drink enough water.
If bile stagnates, you can drink 1 tbsp 20 minutes before meals. l. vegetable oil, since it has a choleretic effect and stimulates motor skills. Every night at night, drink kefir with several prunes, and exclude foods from the menu if they cause you increased gas (these are all legumes, raw white cabbage, carbonated drinks and whole milk).