A German surgeon, professor at the University Hospital in Greifswald, Erwin Payr, described the clinical picture of the disease, which is caused by a narrowing of the large intestine in the area of its inflection at the junction of the transverse colon with the descending colon. This symptom complex was manifested by cramping pain in the left hypochondrium, associated with impaired patency of intestinal contents and gases in the area of the splenic flexure of the colon. Subsequently, this disease (more precisely, the syndrome) was named after the scientist who discovered it - Payr's syndrome. One of the sphincters, located just below the splenic flexure, is named after this surgeon. Research shows that about 46% of cases of chronic colostasis are associated with Payr's syndrome. That is, the problem is quite common. Lack of awareness of doctors about this disease leads to the fact that patients are treated for a long time for other diagnoses.
Patients with pain in the left hypochondrium are often treated for completely different diagnoses.
Symptoms that are observed with splenic angle syndrome
1. Abdominal pain. This is the most common symptom of Payr's syndrome. The pain is usually localized in the left hypochondrium. Sometimes abdominal pain in localization resembles a heart attack. The pain is described by patients as severe and lasts several minutes. These pains may recur several times over several weeks and months. It is quite common for the pain to intensify during physical activity and after a heavy meal. Many patients note an increase in pain intensity with age. And although a number of authors classify Payr's syndrome as a clinical variant of irritable bowel syndrome (IBS, Irritable Bowel Syndrome), there are still studies confirming the presence of inflammatory changes in histological examination of the intestinal wall. 2. Constipation. Most patients report stool retention. The duration of constipation can reach 5 days. Obviously, the intensity of the pain syndrome depends on the duration of constipation. 3. Ileocecal reflux. Due to overstretching of the large intestine, reflux of the contents of the large intestine into the small intestine can occur - colonic reflux. Rejection can also be of a congenital nature: with a congenital anomaly of the ileocecal valve and its insufficiency. When colonic contents enter the small intestine (due to a significant difference in the composition and quantity of microflora), an inflammatory process occurs. The so-called reflux ileitis. Therefore, pain can also be observed in the right abdomen. 4. Nausea and vomiting. The reasons for the mechanism are reflex. 5. Fever, headache, irritability. And if a systemic reaction, an increase in temperature, is a rather rare symptom, then irritability and headache are constant companions of a patient with Payr’s syndrome. If you have chronic pain and stress, try to stay calm... Plus, intoxication is added to nervous exhaustion.
Examination and diagnosis
To correctly determine the stage (staging) of the tumor, it is necessary to undergo preoperative examination.
Standard screening for colon cancer includes:
- Fibercolonoscopy (FCS) with tumor biopsy;
- Histological examination of a biopsy sample (obtained during FCS);
- CT scan of the chest and abdomen;
- Blood test for CEA (tumor marker).
In diagnostically difficult situations, additional studies may be needed, such as virtual CT colonoscopy, PET-CT, and so on. However, in the vast majority of cases, the standard examination described above is sufficient.
The actual operation for colon cancer consists of partial removal of the colon, fatty tissue around the feeding vessels (mesentery) and lymph nodes of 1, 2, and sometimes 3rd order, these components are the oncological nature of the operation. Unfortunately, after resection of the colon, it is not always possible to restore the natural course of the intestine to the anus; in these cases, a colostomy is performed ("output" of the intestine to the abdominal wall). However, with colon cancer, the likelihood of a colostomy is much lower than with rectal cancer. Planned resections of the colon are relatively rarely accompanied by an ostomy, and in cases where this is necessary, as a rule, the possibility of reconstructive surgery is retained to restore the continuity of the colon.
Causes of Payr's syndrome
Pain and discomfort in the gastrointestinal tract have many different causes, pain in the splenic angle is no different. Here are a number of reasons: 1. Pronounced bending of the colon in the splenic angle. May be a consequence of coloptosis (low position of the transverse colon). Coloptosis can be either a congenital anomaly (for example, a long transverse colon) or observed in overweight patients. In general, coloptosis is often observed in obese people. Why is the large intestine also called Intestinum Crassum in honor of the commander Marcus Licinius Crassus (who suppressed the uprising of Spartacus), a very plump man.
The long transverse colon results in the formation of a very strong bend at the splenic angle
2. Accumulation of gases. This is believed to be the most common cause of splenic flexure syndrome and is due to excess gases in the large intestine. In order for the patient to get rid of discomfort, it is necessary to reduce gas formation and improve the release of gases. 2. Bloating. Here there is more due to neighboring organs, for example, the stomach. Excessive gas production can be caused by poor digestion of food in the stomach and small intestine. Or due to the so-called aerophagia - swallowing air. This is a fairly common cause of colic in newborns (aerophagia when screaming and crying). This can occur when drinking quickly, chewing gum, or breathing through the mouth. 3. Inflammatory bowel diseases (nonspecific ulcerative colitis and Crohn's disease). With these diseases, the intestinal mucosa suffers quite severely. 4. Food poisoning. Most often caused by various bacterial agents (salmonella, staphylococcus, clostridia, pathogenic strains of E. coli). 5. Postoperative period. Against the background of postoperative paresis (functional weakening of peristalsis). This can lead to pain in the left hypochondrium. 6. Various obstacles. This is usually cancer of the descending colon. 7. Functional weakening of peristalsis during peritonitis. 8. Intestinal obstruction. 9. Changing the composition of the diet. The presence of a large amount of short-chain carbohydrates in the diet: they can retain water in the intestinal lumen and enhance fermentation processes. Examples: apples, prunes, Brussels sprouts, cherries. Products that increase flatulence: potatoes, soybeans, peas, broccoli, alcohol.
Irritable bowel syndrome (IBS) is currently defined as a chronic functional disorder, the main descriptor of which is recurrent abdominal pain associated with defecation in inextricable association with disturbances in the frequency or shape (consistency) of stool [1]. The relevance of the process of active study of this nosological form is dictated not only by its significant prevalence, but also by a significant decrease in the quality of life of patients.
The diagnosis of IBS depends on a carefully calibrated interpretation of the temporal relationship of abdominal pain with the predominant type of change in the patient's bowel habits. At the same time, the authors of the Rome-IV criteria (Rome-IV) emphasize that although the main goal of developing the “criteria” was to provide a ready-made, easily applicable in practice structure for diagnosing IBS, there is still no ideal test specific only to this disease [2] .
The diagnosis of IBS is established when the patient’s complaints meet the diagnostic criteria of Rome-IV, and symptoms of “anxiety” must be excluded: unmotivated weight loss, nocturnal symptoms, onset in old age, constant abdominal pain as the only symptom of the disease, family history of colorectal cancer, celiac disease, inflammatory bowel disease, fever, organ changes on physical examination, blood in the stool in the absence of hemorrhoids or anal fissures, leukocytosis, iron deficiency anemia, accelerated ESR, changes in blood biochemical parameters [3].
Chronic abdominal pain syndrome with disturbances in transit through the gastrointestinal tract (GIT), characteristic of IBS, is similar to the symptoms that occur with a variety of diseases. In general, abdominal pain has been and remains a serious problem in internal medicine and gastroenterology [4]. Understanding the mechanisms underlying the formation of pain can partly help in establishing its cause and choosing a way to relieve it. The most common mechanism of abdominal pain is visceral pain, which is caused by increased pressure, stretching, tension, circulatory disorders in the internal organs and can be the result of both organic and functional diseases. The pain is usually dull, spastic, burning in nature, and has no clear localization. It is often accompanied by a variety of vegetative manifestations: sweating, anxiety, nausea, vomiting, pallor. Due to the large number of synapses between neurons, double innervation often occurs, which underlies irradiation: reflection of pain during an intense visceral impulse in the area of zones of increased skin sensitivity, at the site of projection of other organs innervated by the same segment of the spinal cord as the involved organ [5] .
Variable characteristics of abdominal pain syndrome in IBS [6, 7]:
- most often the pain is diffuse, without irradiation;
- localized in the lower abdomen (usually in the left abdomen);
- if there is a so-called gas pockets in the area of the hepatic or splenic flexures; pain can be localized in the right or left hypochondrium;
- episodes of acute pain are often superimposed on more constant dull pain;
- eating, as a rule, provokes or intensifies pain;
- defecation usually relieves the pain, but may not completely relieve it.
The visceral genesis of pain in IBS is often combined with psychogenic mechanisms. A deficiency of inhibitory factors and/or an increase in normal incoming afferent signals due to damage to central control mechanisms and/or a decrease in the synthesis of biologically active substances (bradykinin, serotonin, histamine, prostaglandins, etc.) lead to a change in the sensitivity threshold of sensory receptors or directly activate them. The same processes can provoke or aggravate spasm of intestinal smooth muscles, which in turn causes irritation of nociceptors and the sensation of pain [8].
Differential diagnosis for IBS is traditionally carried out with such diseases as [9, 10]:
- inflammatory bowel diseases;
- microscopic colitis;
- enteropathy (celiac disease, lactase deficiency);
- colorectal cancer;
- diverticular disease of the intestine;
- parasitic (infectious) colitis;
- gynecological pathology (endometriosis, ovarian cancer, inflammatory diseases of the pelvic organs).
In our opinion, this list needs to be supplemented with one more pathology, which is extremely rarely mentioned by internists. One of the causes of abdominal discomfort, including constipation, diarrhea and pain, may be an anatomical abnormality in the development of the large intestine.
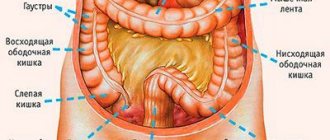
During embryogenesis, disturbances in the development of the large intestine can affect any processes of its formation. According to the classification of G.I. Vorobyova et al. (1989), distinguish anomalies of the intramural nervous system, congenital angiodysplasia of the colon, congenital elongation of the colon, congenital violation of the position and fixation of the colon, duplication of the colon, a combination of various anomalies [10].
Dolichocolon - elongation of the entire colon or one of its sections, is the most common anomaly of the development of the large intestine. Colon elongation is diagnosed in every second patient suffering from constipation for a long time. The incidence of this condition in newborns is more than 30%. According to pediatric studies, this anomaly occurs in 30–40% of children with chronic constipation and abdominal pain. In adults, dolichocolon occurs with almost the same frequency in different age groups (from 23.8 to 31.0%) [11].
According to the anatomical principle, dolichocolon is classified based on the section of the colon, the length of which exceeds the average statistical value.
The following types of dolichocolon are distinguished [10]:
- dolichosigma;
- left-sided dolichocolon;
- dolichotransversum;
- right-sided dolichocolon;
- subtotal dolichocolon;
- total dolichocolon.
From a practical point of view, the clinical principle of classification is of greater importance, on the basis of which dolichocolon is divided into the following forms [11]:
- dolichocolon without clinical manifestations (asymptomatic dolichocolon);
- dolichocolon with impaired transit through the colon;
- complicated dolichocolon.
Complications of dolichocolon include volvulus, intussusception and nodulation. At the same time, sigmoid colon volvulus firmly ranks 3rd among the causes of acute intestinal obstruction, and the mortality rate in the development of this complication reaches 15%, in the case of necrosis - 46%.
The leading clinical manifestation of dolichocolon is the picture of constipation. According to M.F. Osipenko [12], the diagnostic specificity of constipation with dolichocolon is 76%, sensitivity is 80%. The risk of constipation is significantly higher in the presence of elongation of the sigmoid colon compared to other types of dolichocolon. At the same time, stool retention for up to 3 days is often not accompanied by other complaints, while longer and more severe constipation is combined with abdominal discomfort, pain, flatulence, up to a deterioration in general well-being, social maladjustment, and the development of attacks of dynamic intestinal obstruction.
Abdominal pain syndrome, the second most important criterion for dolichocolon, is more often observed in women. In this case, abdominal discomfort in the form of dyspareunia may occur, which often leads to delays in establishing the true cause of the pain syndrome. Abdominal pain with dolichocolon fully meets the criteria for IBS: it is associated with bowel movements and is often associated with changes in stool consistency. Determination of rectal sensitivity in people with constipation using the balloon dilatation test did not reveal differences in the groups of patients with dolichosigma and IBS [12].
The most informative method for diagnosing anomalies in the development and position of the colon is x-ray. The study allows you to immediately determine the position of the colon in the abdominal cavity, the shape and size of all its sections, and mobility when conducting the study with the patient standing and lying down. The following clinical examples will demonstrate the diagnostic value of this diagnostic method.
Clinical case 1
Patient D., 26 years old, complained of pain in the lower abdomen without connection with the act of defecation or stool disorders; bloating, “belly like a stone.” During irrigoscopy (Fig. 1), the colon is elongated, forms additional loops in the area of the splenic and hepatic angles, and the transverse colon descends to the level of L4–L5. The ascending section is also elongated, the dome of the cecum in the small pelvis is at the level of the recto-sigmoid junction. In the vertical projection (Fig. 2), the hepatic angle is displaced to the level of the iliac wing, the dome of the cecum and part of the transverse colon in the pelvic projection.
Clinical case 2
Patient B., 37 years old, did not actively complain at the time of examination; she periodically noted discomfort in the mesogastrium and bloating. Previously, she was hospitalized due to a sudden attack of pain: bloating, pain in the right iliac region. During the examination, no evidence of acute surgical pathology was revealed; the use of antispasmodics was recommended; the effect was not persistent. A month later, mesogastric pain, nausea, and bloating reappeared. No stool abnormalities are noted. When irrigoscopy (Fig. 3) the colon is elongated, due to the transverse colon and ascending sections it forms additional loops in the area of the splenic and hepatic angles, the dome of the cecum is at the level of the entrance to the small pelvis, the additional loop of the hepatic angle descends to the level of S1–S2. In the vertical projection (Fig. 4), there is a downward displacement of the right flank; the dome of the cecum is located at the level of the rectal ampulla.
Clinical case 3
Patient S., 34 years old, complained of pain in the mesogastrium, lower abdomen, dipareunia, and bloating. Examined by a gynecologist - no organic pathology. When irrigoscopy (Fig. 5) the colon is lengthened due to the sigmoid colon, the transverse colon is also lengthened, which has additional bends in the area of the hepatic and splenic angles, the central part of the transverse colon is located above the entrance to the pelvis.
Discussion
The choice of treatment tactics for dolichocolon is based on the clinical form of the disease. Asymptomatic dolichocolon does not require conservative or surgical treatment, however, patients should be warned about the possible further development of slow-transit constipation and the potential threat of complications. Such patients require primary prevention of constipation, primarily nutritional correction [13]. The diet should be physiologically complete; it is recommended to exclude from the diet foods that enhance the processes of putrefaction and fermentation in the colon, rich in essential oils, and extra-active substances. The patient's diet should be enriched with hard-to-digest dietary fibers that improve propulsive intestinal motility (dietary prokinetics). However, it should be remembered that the condition of patients with dolichocolon on the background of a high-slag diet may worsen due to increased flatulence and heaviness in the abdomen.
Treatment of dolichocolon with impaired transit through the colon should be carried out in accordance with the principles of treatment of slow-transit constipation [14]. In addition to dietary measures, it is necessary to maintain a water and drinking regime, exercise therapy, physiotherapeutic treatment (cutaneous and rectal electrical stimulation of the colon, acupuncture, laser therapy), as well as drug therapy.
Drug therapy includes the prescription of drugs that increase the volume of intestinal contents (psyllium seed preparations, fine-crystalline cellulose), osmotic laxatives (lactulose, magnesium sulfate, polyethylene glycol), enterokinetics (trimebutine). For pain syndrome, the addition of selective antispasmodic drugs (pinaverium bromide, mebeverine) to therapy is indicated; the use of antidepressants is also possible. The prescription of each drug must be justified from the standpoint of effectiveness and safety [2, 14].
In case of ineffectiveness of conservative therapy for dolichocolon, accompanied by impaired transit through the colon, the possibility of surgical treatment may be considered [15]. The indication for surgical intervention is the ineffectiveness of conservative therapy in cases of severe impairment of quality of life. Surgical treatment of dolichocolon involves resection of the colon in the amount of subtotal resection, less often - performing fixing operations (mesosigmoplication, sigmopexy, cecopexy), however, the latter are usually accompanied by unsatisfactory functional results.
Conclusion
Despite the presence in the International Classification of Diseases Q43.8, other specified congenital anomalies of the intestine as a separate, independent nosological form, dolichocolon, as a rule, is not considered, and the diagnosis and treatment of this condition are discussed within the framework of other diseases. Clinical manifestations of dolichocolon according to a number of main markers correspond to the criteria for such a common functional pathology as IBS. However, dolichocolon, being a congenital anatomical anomaly, cannot be classified as a functional pathology, since it is often accompanied by the development of complications requiring urgent surgical intervention.
Patients with typical symptoms of IBS in the absence of alarming signs usually do not need additional instrumental examinations. However, when IBS is refractory to therapy, it makes sense to think about conducting a targeted examination - irrigoscopy, in order to explain the true cause of abdominal pain and gastrointestinal transit disturbances. Explaining the genesis of symptoms, primarily abdominal pain, leads to the establishment of a trusting relationship between the doctor and the patient and helps to increase adherence to treatment. The focus of therapy should be on eliminating symptoms and restoring patients' quality of life.
Diagnosis of Payr's syndrome
Currently there is no single diagnostic procedure that can accurately identify and confirm Payr's syndrome. 1. Taking an anamnesis. Like in a student's medical history. A characteristic “sketch” of a future diagnosis can be drawn up after a detailed questioning of the patient: how, where and what is bothering him. It is necessary to identify the connection between pain and body position, food intake, and movement. How and under what circumstances the symptoms appeared. Information about concomitant diseases is required. Therefore, asking the patient has always been and will be in the first place. 2. Inspection. By palpation you can determine the location of abdominal pain, its nature and intensity. Sometimes, when percussing in the area of the splenic angle, there may be a characteristic “drum” sound in the left hypochondrium. 3. Irrigography. No, not a colonoscopy. Nevertheless, for the recognition of Payra's disease, it is a decisive method. This is an x-ray diagnostic method that uses barium sulfate as a contrast agent. The barium suspension is diluted with saline in a ratio of 1 to 3 and injected into the rectum (the intestine is pre-cleansed with laxatives) under the control of an X-ray screen. In this case, they pay attention to the shape and position of the large intestine (and the method is quite visual). The images are taken while lying on your back (with a full colon) and standing - after emptying. Attention is focused on the bend of the colon at the splenic angle. 4. Colonoscopy. With this method, it is possible to identify a number of diseases that lead to disruption of the passage of intestinal contents (including adenocarcinoma of the colon). 5. Computed tomography and magnetic resonance imaging of the abdominal cavity.
What is colon cancer?
Colon cancer is a malignant tumor of the colon. As with neoplasms of other locations, for this type of cancer the prognosis and chances of cure depend on the stage of the disease. In the early stages, it is possible to remove the affected organ or part of it; in later stages, it is necessary to supplement it with chemotherapy. However, cure is possible even with metastatic forms (in the presence of distant “screenings” of the tumor in other organs, most often in the liver and lungs). Depending on the location of metastases, their number and the general condition of the patient, in some cases it is possible to remove not only the primary tumor with regional lymph nodes, but also metastases. However, this is not possible in all cases of metastatic cancer.
Treatment of Payr's syndrome
1. Diet correction. Actually, this is the first recommendation that is given to a patient with this problem. Foods that promote flatulence should be avoided. Foods high in fat, starch and sugar should be limited. It is recommended to increase the amount of fiber in your diet. Meals should be fractional, in small portions. 2. Normalization of stool. If diet does not provide adequate treatment, then mild laxatives are recommended. 3. Avoiding swallowing air. In addition to avoiding chewing gum and drinking soda, doctors advise taking prebiotic supplements before meals and chewing food thoroughly. 4. Medicines. For Payra's disease, the following is used: - Antacids. Reduces bloating. - Antispasmodics. Given to relieve abdominal pain. - Antihistamines. Some are used to relieve pain and intestinal spasms - Metoclopramide. Improves peristalsis and relieves abdominal pain. 5. Physiotherapy. Pain syndrome is relieved by electrophoresis with novocaine on the anterior abdominal wall, diathermy on the lumbar region. Therapeutic gymnastics gives a good effect.
Prognosis of splenic angle syndrome
The prognosis in the initial stages and with appropriate treatment is favorable. The effect of surgery is good, but there is a risk of complications from surgery. I remind you: do not self-medicate. Seek help from your doctor.
If you find a typo in the text, please let me know. Select a piece of text and press Ctrl+Enter.
Tags: anatomy, sphincter, colon
- Related Posts
- When the balance is out of balance: intestinal neural dysplasia
« Previous entry
MRSA: what doesn't kill us will make us stronger
Discussion: 4 comments
- Dmitriy:
2018-08-09 at 07:11Thanks for the review. Everything is clear and understandable. Is it possible to correct a defect using an endoscope? Is colon hydrotherapy used? I am a general practitioner, and my interest is not idle. I would be grateful for your answer.
Answer
Doctor:
2018-08-14 at 00:25
Hello! Do you mean laparoscopic surgery? Laparoscopic treatment is carried out. There are two options: laparoscopic reduction of the splenic flexure and resection of the elongated transverse colon. In the second option, it is technically very difficult to do completely minimally invasively, so a two-stage method was adopted. Mobilization of the intestine is performed entirely laparoscopically, while the anastomosis itself is performed extracorporeally. If by endoscope you meant colonoscope, then no - it cannot be adjusted “from the inside”. I have a rather reserved attitude towards colon hydrotherapy. But the siphon enema is our everything)).
2018-11-06 at 13:48
I also have Payr's syndrome (diagnosed by irrigography), well, the pain is in the ileocecal area, minor flatulence gives a severe pain. After the operation, how many months does it take to fully recover? (if a colon anastomosis was performed)
Answer
- Doctor:
2018-11-09 at 19:35
It all depends on the specific situation. The “strict” period after surgery is about 1.5 months (diet, limited physical activity).
Stages of Colon Cancer
Regardless of where cancer cells initially form, the cancer can begin to spread or metastasize through tissues, the lymphatic system, or the bloodstream. The stage of colorectal cancer indicates how far the disease has progressed, which will help guide treatment decisions.
Colon cancer has the following stages:
- Stage I: In this stage, only the inner layer of the walls (mucosa) of the colon or rectum contains cancer cells. The cancer has not spread to the walls of the organ.
- Stage II. Here, cancer cells have already spread through the inner layer of the wall of the rectum or colon, but have not reached the lymph nodes or nearby tissues.
- Stage III. Cancer cells have spread to one or more lymph nodes, but not yet to other organs. Most often, 3 to 4 lymph nodes are affected at this stage.
- Stage IV. Cancer cells have spread to distant organs such as the liver or lungs.