Reflux esophagitis is a chronic disease associated with inflammation of the esophageal mucosa due to the reflux of gastric contents into the esophagus (reflux). Reflux esophagitis is a manifestation of gastroesophageal reflux disease, which in turn most often develops against the background of a hiatal hernia.
Reflux esophagitis is perhaps the most common disease of the gastrointestinal tract. According to various studies, about 50% of the adult population of developed countries experience symptoms of reflux at one time or another, but only 9.5% are diagnosed. This is due to the fact that in mild cases people do not seek medical help.
Complaints with reflux esophagitis
The most common complaint with reflux esophagitis is heartburn. Most often it is perceived as a burning sensation in the chest, sometimes a sour taste in the mouth, and sometimes takes a debilitating form, significantly reducing the quality of life. It occurs when overeating, or eating certain foods, and is often worse when lying down or bending over. Heartburn can also occur on an empty stomach or during prolonged fasting. Heartburn worsens when lying down; in severe cases, it forces patients to sleep in a sitting position.
The second most common symptom of reflux esophagitis is chest pain. The pain is associated with inflammation in the wall of the esophagus. The pain intensifies while eating; patients literally feel the passage of a bolus of food through the esophagus. Analgesics do not relieve pain. Antacids and sometimes drinking cold water provide relief.
Also often with esophagitis, belching occurs, which is associated with a concomitant hiatal hernia.
Often, reflux esophagitis is accompanied by complaints characteristic of other diseases, the so-called extraesophageal manifestations of reflux esophagitis. A dry cough that gets worse after eating or lying down is common. When examining such patients, lung diseases are not detected, but sometimes chronic bronchitis or bronchial asthma are detected, which significantly complicates the diagnosis of reflux esophagitis.
Another common extra-esophageal manifestation of esophagitis is hoarseness and frequent pharyngitis, which are difficult to treat until medications are used to treat esophagitis. Also, with reflux esophagitis, heart rate arrhythmias and tooth decay are not uncommon.
Diagnosis of reflux esophagitis
Diagnosis of reflux esophagitis most often does not cause difficulties. For an experienced gastroenterologist, it is often enough to collect complaints and a medical history to suspect a diagnosis of reflux esophagitis.
The most important and informative diagnostic method is gastroscopy (FGDS) .
Reflux esophagitis, endoscopic picture
When examining the esophagus, inflammation in its mucous layer, erosion, and ulcers are revealed. According to gastroscopy, the degree of the disease is determined. Sometimes so-called endoscopically negative reflux esophagitis occurs, in which case the wall of the esophagus appears unchanged, although there are complaints.
X-ray of the esophagus with barium - used to diagnose a possible concomitant hiatal hernia; also during this study, it is possible to document the fact of reflux of gastric contents into the esophagus, its severity, and duration. The speed of passage of contrast through the esophagus is also assessed, which makes it possible to judge motility disorders and indirectly judge the presence of inflammation in its walls.
In difficult cases, daily pH measurements or daily impedance measurements are performed to clarify the diagnosis. These studies make it possible to measure acidity in the lumen of the esophagus and identify reflux of gastric contents, determine its nature and the time of contact of aggressive contents with the esophageal mucosa, this is of great importance for developing treatment tactics.
Sometimes, after several years of illness, heartburn either goes away completely or decreases significantly, without treatment, and this is a bad sign, most often indicating the development of complications.
Consequences
GERD is not a harmless disease; it does not go away on its own and requires mandatory correction. A common complication is inflammation of the mucous membranes of the walls of the esophagus due to constant irritation. Inflammation often leads to an ulcerative process and the formation of strictures - areas of scarring and narrowing of the lumen. If the patency of the esophageal canal is disrupted, it causes dysphagia with severe belching.
Ulcerative defects lead to damage to the deep layers of the esophagus and bleeding. The chronic course provokes strong morphological transformations of the mucous tissues of the esophagus with the replacement of their epithelial layer, typical of the stomach and intestinal tract. In this case, the motility of the esophagus is disrupted, and the transport of the food bolus becomes difficult. Another complication is the degeneration of the cells lining the sphincter and esophagus into an oncogenic type. In 5-7% of patients with chronic gastroesophageal reflux, esophageal cancer is diagnosed.
How to identify the disease
Diagnosis of GERD is usually not difficult and does not raise doubts. The main informative research method is esophagogastroduodenoscopy - endoscopic examination of the features of the esophagus and stomach. During the endoscopic examination, it is possible to perform a biopsy for histological examination of tissue, for example, if Barrett's esophagus is suspected.
Based on the results of an X-ray examination, it is possible to clarify the possible cause of reflux esophagitis. The images can clearly identify diaphragmatic hernias, neoplasms, and areas of strictures (narrowing). Sometimes an X-ray contrast test is prescribed to confirm reflux disease.
Another examination is manometry, which allows you to calculate the pressure of the lower part of the sphincter. Gastroesophageal reflux is characterized by a positive reaction to the Bernstein test. For this purpose, 0.1% hydrochloric acid is injected into the esophagus. Patients with reflux experience a burning sensation in the esophagus and stomach. Immediately after the administration of antacids, the unpleasant sensations are relieved. To examine the motor function of the upper gastrointestinal tract, electromyography is indicated.
For early detection of morphological changes in the esophagus, esophageal sphincter and stomach, it is recommended to undergo gastroscopy with a biopsy of the membranes. Considering that patients often complain of a dry cough, it is important to exclude ENT pathologies. If laryngopharyngitis is excluded, then a course of treatment with antacids is prescribed.
Classification of reflux esophagitis
The two most widespread classifications of esophagitis in the world are the Savary-Miller classification, adopted in 1977 and modified in 1997 at the 6th European Gastroenterological Conference, and the Los Angeles classification, also adopted in 1997. It is considered more complete and therefore more often used.
Savary-Miller classification
1st degree - one or more erosions occupying less than 10% of the circumference of the esophagus 2nd degree - merging erosions occupying more than 10, but less than 50% of the circumference of the esophagus 3rd degree - multiple erosions occupying the entire circumference of the lower third of the esophagus 4th degree - complications of reflux esophagitis: esophageal ulcer, stricture, Barrett's esophagus
Los Angeles classification of esophagitis
Grade A - damage to the wall no more than 5 cm long, within one fold of the mucosa Grade B - damage more than 5 cm long, but within one fold Grade C - damage more than 5 cm long, occupying up to 75% of the circumference of the esophagus Grade D - damage to the mucosa occupying 75% or more of the circumference of the esophagus
Complications of reflux esophagitis
With inadequate therapy, or its insufficient effectiveness, or in the absence of treatment, reflux esophagitis continuously progresses and can lead to quite serious complications. The most common complication is the development of Barrett's esophagus, in simple terms, this is a situation when the structure of the cells of the esophageal mucosa, under the influence of constant inflammation, begins to change its structure. This process is called dysplasia. Barrett's esophagus is considered a precancerous disease, as it significantly increases the risk of developing esophageal adenocarcinoma (cancer).
Also a frequent complication is the development of severe erosive ulcerative lesions of the esophageal mucosa, which in turn are complicated by either bleeding or stricture (narrowing) of the esophagus. Bleeding can be either chronic, invisible to the patient, or acute, quite profuse and life-threatening. With chronic bleeding from erosions and ulcers of the esophagus, the patient feels unmotivated weakness and, when taking a blood test, anemia is detected.
Stricture of the esophagus (narrowing of the lumen), as mentioned above, develops against the background of erosive esophagitis, or ulcerative lesions of the esophageal mucosa, in the absence of adequate treatment. Signs of a narrowing of the esophagus include difficulty swallowing and vomiting of food that has just been eaten. Esophageal stricture requires immediate treatment
Symptom complex
The clinical picture of GERD is typical for children and adults. The disease begins with constant heartburn, which intensifies after exercise, bending, or eating. Belching is sour with a bitter aftertaste. Young children begin to refuse food, as eating increases discomfort and pain. Other symptoms of the disease are:
- dysphagia or impaired swallowing due to decreased motility or esophageal stricture;
- vomiting, nausea;
- discomfort in the epigastrium, intestinal tract;
- excessive salivation;
- hoarseness;
- foul breath.
With chronic damage to the esophagus, patients suffer from bronchospasms and focal pneumonia. The development of pulmonary fibrosis and laryngotracheitis is likely. Due to disturbances in the microflora of the oral cavity, the enamel often undergoes demineralization and caries develops. GERD is dangerous due to the development of complications associated with chronic burns of the sphincter and esophagus. Patients with gastroesophageal reflux most often develop an ulcerative-necrotic process, perforated ulcers.
The danger is represented by the asymptomatic or sluggish form of GERD, when the appearance of active symptoms already indicates significant destruction of the membranes.
Treatment of reflux esophagitis
Treatment of esophagitis is carried out both conservatively and surgically. Of course, the overwhelming majority of patients are treated conservatively by a gastroenterologist. The goal of treatment is to remove symptoms, prevent the development of complications, and improve quality of life. You need to understand that it is often impossible to cure reflux esophagitis with conservative methods once and for all, and either constant or periodic maintenance therapy is required. The only way to radically get rid of esophagitis is through surgery.
Lifestyle change
The first thing a competent gastroenterologist will recommend when treating reflux esophagitis is optimizing the patient’s lifestyle, and it must be said that this is the most difficult thing in treating this disease. If you are overweight, you should lose weight. Patients are recommended to eat frequent meals, at least five times. Last meal 4 hours before bedtime. It is recommended to sleep with the head end raised, and you should not put pillows on it, but raise the head end of the bed. Alcoholic drinks, coffee, tea, and sour foods are prohibited. Limiting physical activity associated with heavy lifting and working in an inclined position.
So let's summarize what you need to change in your life:
- after eating, avoid bending forward and not lying down;
- sleep with your head elevated;
- do not wear tight clothes and tight belts;
- avoid large meals;
- do not eat at night;
- limit the consumption of foods that cause a decrease in LES pressure and have an irritating effect (fats, alcohol, coffee, chocolate, citrus fruits);
- stop smoking;
- normalize body weight, if it is excess;
- Avoid taking medications that cause reflux (anticholinergics, sedatives and tranquilizers, calcium channel inhibitors, beta blockers, theophylline, prostaglandins, nitrates).
Drug treatment
- Drug therapy for duodenogastric reflux aims to normalize all functions of the gastrointestinal tract and regulate the motor-evacuation function of parts of the digestive system. A drug that improves intestinal motility is Trimedat.
- Prokinetics (Domperidone, Cerucal) show good results in therapy. They help the rapid absorption and digestion of food, as well as the movement of its remains through the small intestine.
- To neutralize the effect of the contents of the duodenum on the gastric mucosa, drugs are prescribed - (Omez, Nexium).
- Antacid medications - Almagel, Gaviscon, Phosphalugel - help get rid of heartburn.
It must be remembered that treatment of duodenogastrol reflux should begin when the first symptoms of the disease appear. By consulting a doctor in the early stages of the disease, you prevent the development of a serious complication - reflux gastritis.
Conservative therapy
For conservative therapy, the following groups of drugs are used:
- antacids and alginates
- proton pump inhibitors
- prokinetics
Antacids and alginates
Antacids and alginates, topical preparations most often containing aluminum and magnesium salts, these drugs act locally, are not absorbed into the blood and do not have a systemic effect. Their advantage is safety of use, but there is also a disadvantage, a short duration of action. Antacids are not used as an independent method of treatment, but are used as first aid for heartburn, and as an intensification of therapy for the speedy healing of erosions and ulcers of the esophagus. Preparations in the form of gels with alginic acid have proven themselves to be the best, which, when interacting with acid in the lumen of the stomach, form foam, thereby increasing the duration of action of the drug and its effectiveness. Antacids are most often prescribed 40 minutes after meals and at night, or on demand in case of heartburn.
Proton pump inhibitors (PPIs)
Today they are the main drugs in the treatment of reflux esophagitis, these include the well-known omeprazole, lansoprazole, rabeprazole, etc. These are systemic drugs, they block the transport of hydrogen molecules into the parietal cells of the stomach, responsible for the secretion of hydrochloric acid, and how do we We remember from the school chemistry course, this acid consists of a molecule of hydrogen and chlorine, no hydrogen, no acid. These drugs have revolutionized the treatment of reflux esophagitis, significantly improving the outcome and reducing the number of complications. Previously, H2 histamine receptor blockers were used, which were much less effective and had more side effects. It must be said that these drugs are sometimes used now in combination with PPIs to enhance the effect. The main disadvantage of proton pump inhibitors (PPIs) is their fairly rapid removal from the blood, which requires repeated use throughout the day, and even with double use, so-called acid breakthroughs are described, when, more often at night, the acidity of gastric juice sharply increases. Most often, PPIs are prescribed 20 mg twice a day 20 minutes before meals, morning and evening for 6 to 8 weeks. Then maintenance therapy is prescribed at 10 mg per day or 10 mg twice a day.
Prokinetics
Prokinetics are drugs that improve and normalize peristalsis of the gastrointestinal organs, including the esophagus. The most commonly prescribed drug is itopride, which is considered the most effective and safe drug. Motilium is also prescribed. The previously popular cerucal has recently been deprecated due to its central effect on the brain. Prokinetics are prescribed 1 tablet three times a day 20 minutes before meals. A course of 2 weeks is recommended.
Problems of conservative therapy
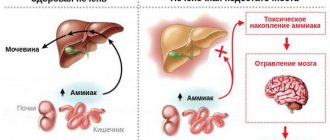
The vast majority of patients with reflux esophagitis are treated conservatively, achieving good functional results, but unfortunately, therapy is not always effective. As we wrote above. The cause of reflux esophagitis is the reflux of gastric contents into the esophagus. So the first problem with conservative therapy is that it does not eliminate the cause, but only relieves the symptoms. With conservative therapy, reflux remains, but is no longer acidic, and therefore patients do not feel any complaints. Although some researchers believe that due to the neutralization of acid, bile begins to flow into the esophagus, since it ceases to be inactivated in the stomach, and bile is an even more aggressive environment for the development of complications of esophagitis. Although it should be noted that this is still a theory that has not received sufficient confirmation. But at the same time, a number of scientists associate the growth of esophageal cancer with this hypothesis. Since, despite the widespread use of PPI drugs, the incidence of esophageal cancer is steadily increasing.
Taking medications in itself can cause complications. Evidence has been obtained that proton pump inhibitors increase the risk of stroke, osteoporosis and heart attack, and although the risk is not quite high, about 0.4 - 0.6% per year, it is still there.
Well, perhaps the main thing is that the effect of conservative therapy is temporary and is not always sufficiently effective. So, 6 months after stopping therapy, complaints return in 40-50% of patients, and after 12 months in 80-90%, that is, most patients are forced to take medications daily for many years. Considering the sufficient safety of the drugs, this may not be scary, although it certainly reduces the quality of life. But the problem lies in the fact that with long-term therapy, after three or five years, the effectiveness of the drugs decreases and in 20 - 30% of patients complaints reappear and complications of esophagitis develop, despite the constant use of the prescribed drugs.
The term "reflux" means the reflux of acidic stomach contents into the esophagus.
Reflux disease occurs when either symptoms appear for this reason or the lining of the esophagus changes. The scientific term for the esophagus is oesophagus. If the mucous membrane of the esophagus becomes inflamed due to irritation caused by exposure to aggressive stomach acid, then in this case doctors talk about reflux esophagitis.
The stomach produces hydrochloric acid to digest food and destroy pathogens. If the muscle at the end of the esophagus closes the entrance to the stomach (cardia) only insufficiently, then the acidic contents of the stomach can rise up and be thrown into the esophagus.
A relatively large number of people suffer from reflux disease. Reflux symptoms are among the most common gastrointestinal problems. It is estimated that 10 to 20 percent of the population in industrialized countries suffer from this disease. Inflammation of the esophagus occurs in about 40 percent of people with this problem. If reflux occurs over a long period of time, it can lead to irreversible damage to the esophagus. About 0.1 percent of people with this problem develop cancer for this reason.
What are the causes of reflux disease?
The causes of reflux disease include the following:
- Esophageal sphincter dysfunction
- Problems with gastric emptying due to nerve damage, such as diabetes
- Rheumatic diseases, such as scleroderma
- Hiatal hernia
- Reduced ability of the esophagus to cleanse itself
- Rejection of small intestinal contents into the stomach
- Pregnancy: About half of all pregnant women suffer from heartburn, a significant symptom of reflux disease. The reason in this case is increased pressure in the abdominal cavity and hormonal changes. In most cases, symptoms disappear after the baby is born.
First of all, dietary errors lead to sour belching or cause excessive production of stomach acid:
- Too large portions of food
- Excessive alcohol consumption
- Foods and drinks that are too fatty, too sweet or salty
In addition, certain medications may cause increased reflux symptoms. Such drugs may be, for example, the following:
- Acetylsalicylic acid
- Nitrates (areas of use for nitrate-based vasodilators include coronary insufficiency, cardiac weakness, and cardiac infarction)
- Products containing peppermint oil
- Psychotropic drugs
- Calcium antagonists (active ingredients in this group are used to treat high blood pressure)
Additionally, anything that puts pressure on the abdomen and stomach, such as being overweight, pregnant, wearing clothes that are too tight, or bending or lifting heavy objects, can lead to heartburn. Anger and stress also cause heartburn in many people.
What symptoms occur with reflux disease?
The main symptom of reflux disease is burning pain behind the breastbone, that is, heartburn. It often appears along with belching and the typical sour taste in the mouth. Typical signs of reflux disease are:
- Feeling of heaviness/pressure behind the sternum
- Pain in the epigastric region
- Difficulty swallowing
- Throwing leftover food
- Nausea and vomiting
- Burning and pain in the pharynx
- Coughing attacks
- Chronic hoarseness of voice
- Inflammation of the larynx and pharynx
These symptoms occur primarily after eating, drinking alcohol, eating fatty or sugary foods, or when abdominal pressure increases. Symptoms may be similar to those of a heart attack.
Constant inflammatory irritation of the esophagus over a long period of time can lead to scarring and narrowing. In addition, there is a danger that an irreversible change in the mucous membrane of the esophagus will occur and the so-called Barrett's esophagus will arise. About ten percent of patients with Barrett's esophagus develop esophageal cancer.
How do doctors treat reflux disease?
Your doctor can treat reflux disease with medications that block acid production in the stomach. In this case, the drugs of choice are the so-called proton pump inhibitors (for example, Omeprazole). In most cases, with this therapy, inflammation goes away, since the mucous membrane of the esophagus only occasionally comes into contact with the acidic contents of the stomach. If symptoms recur after successful treatment, long-term medication may be appropriate for patients.
In addition, to relieve symptoms, doctors have at their disposal, among other things, drugs that neutralize stomach acid. They are called antacids. In addition, medications may be used to help empty the stomach and therefore transport stomach acid into the small intestine. Which medications are needed in each specific case depends, among other things, on the severity and severity of reflux disease.
Only in a few cases is surgery necessary. In this, the surgeon places the upper part of the stomach, the fundus, around the sphincter in the form of a cuff to improve its function. This procedure is usually performed endoscopically, which is a tube through which the doctor inserts a miniature camera and the necessary surgical instruments.
If Barrett's esophagus already exists due to reflux disease, the doctor should regularly carry out control endoscopic examinations of the esophageal mucosa to detect malignant changes at an early stage.
How does a doctor diagnose reflux disease?
After a detailed questioning about complaints, possible concomitant diseases and general living habits, a thorough physical examination of the patient is carried out during a medical appointment.
Endoscopic examination
If a suspicion of reflux disease is detected, the doctor performs an endoscopic examination of the esophagus using an endoscope. In this case, the physician can examine the mucous membrane of the esophagus and clearly assess its condition. He can determine whether inflammation is present and how severe it is. At the same time, the doctor can take samples of the mucous membrane for subsequent histological examination. This study is necessary for the doctor to identify specific tissue changes.
pH-metry
Another possibility for diagnosing reflux disease is pH testing. In this test, the doctor inserts a thin tube through the nose into the esophagus. This probe remains there for up to 24 hours and is designed to continuously measure the degree of acidity (pH) inside the esophagus. Using this study, it is possible to detect whether there is reflux of stomach contents into the esophagus and what the amount of this content is.
Manometry
To measure pressure in the esophagus, the doctor inserts a thin catheter through the esophagus to the stomach. While the patient swallows the liquid, the provider again pulls the catheter back to the lower esophageal sphincter.
To accurately assess the act of swallowing, in some cases the doctor prescribes an x-ray examination, during which the patient must swallow a special mushy contrast agent. For symptoms that indicate damage to the respiratory tract, for example, hoarseness of the voice, obsessive coughing, sore throat, additional otolaryngological examination is advisable.
What independent actions can patients take?
The following tips will help patients avoid heartburn or alleviate mild symptoms:
- Eat fatty, sweet or spicy foods as little as possible.
- Avoid eating large portions of food. Instead, eat small portions of light foods spread throughout the day.
- The last meal should be no later than three to four hours before bedtime.
- Eat as little as possible of hard-to-digest foods that remain in the stomach for a long time, such as legumes or various types of cabbage.
- Instead of sour fruit juices and carbonated drinks, drink still water or tea.
- Avoid drinking strong or acidic alcoholic drinks such as vodka (schnaps) or wine.
- Reduce the amount of coffee you consume.
- Stop smoking.
- Reduce your weight.
- When sleeping, keep your upper body elevated.
- Don't wear clothes that are too tight.
- Move more: This helps reduce excess weight, improves digestion and relieves stress.
- As a quick-acting remedy after a large meal, you can avoid heartburn by walking rather than by taking a light nap.
If you have trouble with the symptoms described in this article, consult a doctor or undergo a basic comprehensive examination of the entire body Check-Up.
Contact us
Consultations, diagnosis and treatment are carried out in the gastroenterology department. In order for you to receive effective treatment, the Academic Hospital Solingen has created an international department for working with foreign patients. We will translate for you from German into your native language and accompany you while you are in the clinic.
Contact us by email or phone: Email: [email protected] Tel.: +49 212 5476913 Viber | WhatsApp: +49 173-2034066 | +49 177-5404270 For your convenience, please save the phone number in your phone book and call or write to us for free on WhatsApp, Viber or Telegram. Applications made on weekends or holidays will be processed on the first business day. In urgent cases, request processing is carried out on weekends and holidays.
Source - https://www.tk.de