Gastritis is an inflammation of the gastric mucosa. It is accompanied by bloating and sharp or aching pain in the upper abdomen. Common symptoms include nausea, vomiting, and belching. The patient has no appetite and weight loss.
It is no secret that a diet for gastritis is a prerequisite. Since there are different types of this disease, the diet includes different foods. And yet, no matter what stage of gastritis, the patient should give up alcohol, fried, fatty and spicy foods. In addition, smoking is also undesirable. Meals should be regular, 5-6 times a day.
What does “Table number 5” mean?
This is a special mode that consists of special dishes, systems and cooking methods. This mode is suitable for use by people of the older and younger generations. The main task of therapeutic diet number 5 is to improve and restore the functioning of the biliary and hepatic systems.
For what ailments is it prescribed:
- Liver inflammation and gallbladder disease (chronic stage).
- Hepatitis in the chronic phase.
- Proliferation of connective tissue of the liver.
Also, table 5 diet is prescribed during the recovery period after surgery on the gallbladder (2 weeks after its removal). In addition, the 5th therapeutic diet is prescribed to pregnant women during toxicosis (mild phase). It is used only in cases of chronic illnesses (without a relapse stage), and during the recovery period.
Contraindications for use:
- Relapse of chronic diseases.
- Complications.
- Associated ulcers, hepatitis.
How is nutritional therapy prescribed and how long does it last?
Any therapeutic nutrition is not prescribed for a day or two. The minimum period of the 5th table is a week, with constant monitoring of the patient. If the patient’s body successfully adapts, the diet is extended. Usually the maximum period of treatment is 1.5 years. There are some factors for the success of the diet, such as the dynamics of treatment. If necessary, the table is adjusted or changed.
The diet prescribed to patients with diseases of the gastrointestinal tract improves their functioning, brings metabolism and digestion back to normal and in balance. But table No. 5 is also useful in that it additionally serves as a prevention of other ailments, improving the functioning of organs.
Three components of success:
- Balance of the chemical composition of products.
- Method of mechanical processing.
- Optimal food temperature.
Nutrients and nutritional value
The purpose of the table is not to eat food that negatively affects all functions and performance of internal organs and the gastrointestinal tract. But we should not forget that food should give a feeling of satiety and completeness, without allowing the feeling of hunger. Everything that the patient eats should not have a high percentage of fat, oils and cholesterol. BJU must be present, but in a small dosage. The daily amount of salt is a teaspoon. The daily calorie intake is 2500 (2800 during pregnancy).
BJU - proteins, fats, carbohydrates.
Temperature
The optimal cooking temperature is up to sixty degrees. If you have diseases of the digestive organs, you should not eat excessively chilled or hot foods. All this irritates the mucous membrane, and can lead to an exacerbation of the current disease and condition.
Mechanical restoration
This process involves reducing the desired products to the state of small pieces. In this form, food is most easily absorbed by the digestive organs, and the digestion process is easier. Diet number 5 also includes whole pieces. Constant grinding and grinding is not necessary.
Type of mechanical processing for some types of products:
- Finely chopped, rubbed with gauze, using a grater (raw and cooked vegetables with high fiber).
- Meat is the same.
- Baking, boiling, steaming (dietary dishes).
Approximate principle of operation: for example, you rarely eat dishes prepared by stewing (vegetable stew, finely chopped meat). Fried foods are prohibited, as they contain processed fats that interfere with the normal secretion of bile. And this is fraught with deterioration of the condition.
The optimal frequency is five times a day, in medium portions. Below you can consider an approximate diet for therapeutic diet 5.
Diet plan 5
The biggest misconception of many patients is that is allowed on diet number 5 . This is a misconception. This regime includes a fairly extensive list of acceptable products. The feeling of hunger will definitely not be familiar to the patient.
Ingredients with a high content of fat, pungency, salt and acid are limited in the table, as they provoke increased secretion of pancreatic juices and also cause irritation of the gastric mucosa. For a list of acceptable and unacceptable products, see the list provided.
what is possible and what is not possible with diet number 5
Diet for gastritis with low acidity
Unlike the previous diet for gastritis, in this case the main task is to stimulate the secretion of gastric juice. In the first days after an exacerbation, the use of meat and fish broths is recommended. After the acute pain passes, pureed soups and cereals can be added to the diet.
The diet for gastritis excludes fatty and fried foods. Do not avoid vegetables rich in dietary fiber, tough meat, and whole milk. You should also avoid freshly baked bread and pastries (the best option is the day after baking).
Dr. Pevzner has developed fifteen therapeutic diets that can be prescribed for both acute and chronic gastritis. The most popular are diet No. 1 and No. 5. Your doctor will tell you which diet for gastritis is right for you.
Table 5 diet
Below is a basic list of do's and don'ts for diet number 5 . Your doctor will give you more detailed information, focusing on the individual characteristics of your body and diagnosis:
- Soups. Light vegetable and cereal meatless first courses are allowed. Decoctions of meat and fish and cold first courses are prohibited.
- Root vegetables and other vegetables. It is allowed to consume some of the pumpkin, nightshade and cabbage families, and kelp. Vegetables that increase stomach acidity and irritate its internal walls, canned vegetables, and regular cabbage are prohibited.
- Meat. It is allowed to eat low-calorie meat (the skin is removed), low-fat beef, as well as homemade semi-finished meat products. A categorical no - all fatty sausages, fatty meats, offal, etc.
- Fish and seafood products. You can eat fillets of lean fish and crustaceans. Not allowed: fatty fish fillets, canned fish, Japanese dishes, caviar.
- Flour products, bakery. You can eat all types of bread, toast, and unsoaked biscuits. You can’t eat butter and puff pastries, store-bought crackers, home-fried pastries.
- Cereals. Cereals boiled until very soft, the addition of dried fruits and lean meat to pilaf, flaxseeds, and muesli are allowed. All types of legumes, barley, corn and barley cereals (in small quantities) are prohibited.
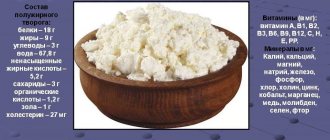
- Milk and its derivatives: natural milk and low-fat products of its oxidation, cottage cheese, hard cheese without seasonings are allowed. High-fat milk and salted cheeses are prohibited.
- Eggs and their derivatives - only foods made from proteins are allowed. Dishes made from whole eggs are prohibited.
- Fruits and berries. Ripe apples, some types of dried fruits, and fruit and berry compotes are acceptable. All types of nuts, seeds, citrus fruits, and raw fruits and berries are unacceptable.
- Sweets. You can eat low-calorie and non-acidic sweets, honey. Not allowed - some types of oriental sweets, chocolate-cream products, hematogen, chocolate.
- Non-alcoholic and alcoholic products. It is allowed to drink rosehip and chamomile infusions, weak black teas, and berry and fruit drinks. Prohibited: any alcoholic beverages, soda, concentrated juices, coffee, etc.
Based on the above, you can create an interesting, healthy and satisfying menu. Try to make a list of dishes in advance - it will be easier. You can immediately buy what you need and create a recipe. And it will take less time and effort to cook.
Enzymes
Enzymes help the digestive organs cope with their direct functions. Gastritis and pancreatitis are precisely the reason for their lack. Special medications, the choice of which in pharmacies is extremely wide, can fill the gap. A popular medicinal enzyme is pancreatin. It is part of such drugs as Mezim, Festal and Creon.
Pancreatin components stimulate the production of pancreatic and intestinal enzymes that break down food at various stages of digestion.
Sample menu for the week
If you don’t understand how to create a menu and what it consists of, see the approximate list for the day.
Day 1
- First time: milk oatmeal with the addition of pureed fruit, tea.
- Repeated breakfast: tea, grated low-fat cottage cheese.
- Second meal: beetroot soup, buckwheat porridge with meatballs, bread, sour cream (10 grams).
- Third method: baked zucchini pancakes, sour cream (10%).
Day 2
- First time: manna, tea with milk (a little).
- Repeated breakfast: toasted wheat bread, jam, slightly acidic jam, weak tea.
- Second meal: lean cabbage soup, a piece of bread.
- Third meal: berry drink, buckwheat cereal. How to prepare it: bring 200 grams of buckwheat until boiled. Cottage cheese (200 grams) wipe, add 1 tbsp. l. sugar, beat in an egg, add 100 ml of milk. Next, combine all the ingredients, add to the buckwheat, and bake in foil in the oven.
Day 3
- First time: steamed carrot pancakes, tea.
- Repeated breakfast: regular cookies, dried fruit compote.
- Second meal: pearl barley soup, low-fat sour cream (a little), bread.
- Third method: boiled cauliflower, steamed chicken dumplings.
Day 4
- First time: semolina casserole, low-strength black tea. How to prepare the casserole: make thick semolina, leave to cool (dosage - two hundred grams). Next, add sugar, 1.5 eggs and a little dried grapes (optional, finely chopped dried plums). Whisk the mixture until fluffy, pour onto a pre-greased baking sheet, and bake until golden brown.
- Repeated breakfast: unsoaked sponge cake, fruit compote.
- Second meal: rice and vegetable soup, separately cooked chicken.
- Third method: chamomile or rosehip infusion, boiled raisin couscous.
Day 5
- First time: milk oatmeal, tea.
- Repeated breakfast: cucumber-carrot salad with the addition of lettuce leaves.
- Second meal: lean borscht, a slice of bread, a small amount of sour cream.
- Third meal: stewed vegetables, some lean beef.
Day 6
- First time: baked pears, honey, tea.
- Repeated breakfast: wheat bread, soft curd mass.
- Second method: milk noodles.
- Third meal: mashed potatoes, meatballs with sour cream sauce, rosehip drink.
Day 7
- First time: protein scramble with the addition of boiled green beans, tea.
- Repeated breakfast: carrot salad with dried apricots.
- Second meal: oatmeal soup, with potatoes and carrots, bread.
- Third meal: meat soufflé, rye toast, chamomile infusion. How to cook: take beef (200 grams), boil, run through a blender a couple of times, add the yolk. Next, add 100 ml of milk and mix. Whisk 2 whites until foamy and add to meat. Steam cooking.
If you still feel hungry, you can snack and have an afternoon snack.
The presented menu is not the main one; you can adjust it yourself. The main thing is to follow the rules: food is only warm; portions are small; ingredients are acceptable.
Diet for gastritis: Table 1
This table is intended for patients with acute gastritis. The diet of this diet involves protecting the stomach from mechanical, thermal and chemical irritants. The consistency of ready-made meals for this diet for gastritis should be liquid or semi-liquid.
Recommended products: day-old wheat bread, dry or biscuits. Dairy or vegetable pureed soups. Lean meat or fish (boil or steam). Soft-boiled eggs, cottage cheese, non-sour kefir. Carrots, potatoes, cauliflower, beets, sweet fruits. Porridge (rice, oatmeal, buckwheat, semolina). Butter, refined vegetable oil (added to prepared dishes).
Therapeutic diet 5a
This regimen is prescribed to patients with exacerbation of the internal digestive organs. It “calms” the digestive organs, the entire gastrointestinal tract, and improves the functioning of the gallbladder.
There is a nuance in the diet: all food should be soft and mushy. The products are the same, but there are a few more restrictions. For example, soups are lean and low-fat, the vegetables in them are grated or chopped to the maximum, finely chopped, and the grains are pureed. You can add milk and spider noodles. Fruits, berries and root vegetables with high fiber are completely removed from the diet. Undesirable: pear, quince, whole cabbage. Millet is prohibited.
Other restrictions: consumption of young calf meat and chicken fillet is undesirable. Bread made from type 2 grade flour is allowed, in the form of toast. The daily norm is about three. Sweets and drinks - similar to the list above. General menu (in brief): porridge, boiled vegetables, mashed potatoes and meat, lean first courses. Other: jelly, jam, steamed cutlets. Maintain a balance of BZHU. It is strictly forbidden to eat in large quantities or, conversely, to starve. This table is assigned until improvement occurs, then they move on to another. Self-adjustment is strictly prohibited.
Therapeutic diet 5b
It is added in addition to conservative treatment for inflammation of the pancreas (chronic course). This type is prescribed during the healing period after acute inflammation of the pancreas or at the “quiet” stage after chronic inflammation.
The list of products on table 5b is similar to the previous one.
The food is warm, the cuts are very small.
Other points: foods that are high in fat and too sweet are removed from the diet. Instead of sugar, use a substitute. What is not allowed with diet 5b : all types of alcohol and soda containing caffeine, sweets and products made from flour. Also prohibited is the consumption of products prepared by smoking, frying and pickling, fruits and berries, and root vegetables that have not been thermally treated. The cottage cheese should be ground, and the rest of the “milk” should only be used in dishes.
Regime: you need to eat up to seven times a day, in small portions. Frequency: 3-3.5 hours after each dose. Type of processing: boiling, steaming, baking. Salt is limited (8 grams per day). This nutrition option is the optimal solution for patients with concomitant chronic gastritis.
Therapeutic diet 5p
As soon as the patient experiences a recurrence of inflammation of the pancreas, he is prescribed a therapeutic diet 5p. Products are introduced no earlier than the seventh or eighth day after the relapse. The list is similar to the previous one.
The daily calorie intake is 2500.
Basic diet: food with a high protein content.
Removed: legumes, nuts. Egg yolk - 1 per day.
The main rule for lunch is lean first courses. It is allowed to use white crackers from dried or day-old bread. “Milk” - only ready-made, infrequently. Allowed desserts: jelly, semolina pudding, jelly. Raw vegetables and fruits are strictly prohibited. When improvement occurs, the patient is transferred to diet 5 or another. If the patient risks breaking his diet, a relapse is possible.
Diet for gastritis with high acidity
The main task of such a diet for gastritis is to reduce the activity of gastric juice. To do this, you need to adhere to three basic principles of a gentle diet for gastritis:
- mechanical - exclusion of foods with coarse fibrous fiber (turnips, radishes, stringy meat, muesli, bran bread), frying in oil;
- chemical - exclusion of strong pathogens of gastric secretion (alcohol, carbonated water, citrus fruits, black bread, strong broths, coffee, white cabbage);
- thermal - eating not very hot and not very cold food (optimal temperature 15-60 degrees).
Reviews and results
Recently, there has been a shift away from the need for strict adherence to dietary nutrition for gastritis. Patients themselves feel the need for it during an exacerbation and exclude those foods that provoke pain. This diet option has been significantly expanded in terms of products and processing methods. This makes it possible to eat a varied and healthy diet, and the complete composition of the main substances allows you to stay on this therapeutic diet for a long time. Reviews from patients indicate its positive effect not only on the condition of the stomach, but also the intestines and pancreas.
- “... If there is a mild exacerbation (it happens in spring and autumn or after errors in food), I switch to diet food for a month or less. This is due to certain difficulties and additional hassle associated with preparing steamed dishes and dietary soups. Of course, steamed cutlets are almost tasteless (I don’t add onions, garlic or spices to them), but you can withstand it for three weeks. I eat a lot of porridges (I don’t include pearl barley, millet and corn, as they make my stomach feel heavy), potato pumpkin and squash puree. Within a month, stool improves, heartburn and heaviness in the stomach disappear. Then I try not to eat spicy, salty, pickled and fatty foods - all this causes heartburn and belching. I’m losing a little weight on this diet”;
- “... I observe it only during periods of exacerbation. I noticed that I haven’t been able to eat onions, garlic, or radishes at all lately—it immediately gets worse. I eliminated mayonnaise a long time ago because it makes my stomach feel bad. Somehow I manage to go on a diet on my own, because pain appears not only in the stomach, but also in the intestines. I brew chamomile and calendula, eat boiled meat and fish, steamed cutlets, and porridge. I exclude cabbage - it increases pain and bloating in the intestines, and this affects the stomach (it immediately puts pressure). Overeating doesn't have the best effect either. And in general, I noticed that with age you have to give up many foods and the list of those that are poorly tolerated is becoming wider. If I’m on a diet for 2 months, I can lose 4-5 kg”;
- “...I have frequent exacerbations because I eat irregularly, often eat dry food and allow myself far from dietary foods. Moreover, this immediately affects the state of health: heaviness in the stomach, heartburn, belching and bloating. I manage without hospitalization, since there are no severe exacerbations. The “gastric” diet works well. After 2 weeks, all unpleasant sensations disappear. The problem is that I can’t keep a diet for a long time, since it’s difficult to combine it with work, and I don’t have time to cook for myself separately. My family doesn’t want to support me in this diet for now.”