Catarrhal reflux esophagitis is the initial stage of the development of a pathology such as gastro-food reflux. Our intestinal tract is designed in such a way that normally food passes through it from the esophagus to the stomach and cannot get back. However, in many pathological conditions, the reverse process is observed and gastric juice, which includes enzymes and hydrochloric acid, can again enter the esophagus, burning its delicate mucous membrane.
As a result of the reflux of gastric contents into the esophagus, changes occur in the tissues of its mucosa, which causes a pronounced inflammatory process. Not every person knows that if catarrhal reflux esophagitis is not treated, then over time it can become chronic and degenerate into a serious disease, including cancer.
According to medical statistics provided by Moscow, the catarrhal form of the disease, although the mildest, is most common in patients.
Types of chronic and acute esophagitis
Symptoms and treatment methods for esophagitis depend on the morphological type.
Both acute and chronic types are divided into several types, differing in manifestations and causes. Acute esophagitis occurs in three cases - when the mucous membrane is damaged by bacteria, after direct exposure to too hot food/drink or toxic substances, and when a foreign body enters it, injuring the surface. Bacterial inflammation occurs most often with scarlet fever, diphtheria, typhoid, and fungal infections.
Based on morphological characteristics, there are 8 types of acute esophagitis:
- Catarrhal - occurs when there is a sharp impact of negative factors (high temperature food, spiciness, marinades, spices, toxic substances, hard foods). Foods high in alkali and iodine also provoke inflammation of the mucous membrane. In the presence of physiological abnormalities (hiatal hernia, stenosis or insufficiency of parts of the esophagus, achalasia, pressure in the peritoneum), hydrochloric acid from the stomach can enter the esophagus and cause irritation and manifestations of catarrhal form.
- Edematous – catarrhal esophagitis develops into it without proper attention. The existing swelling increases significantly, the lumen of the esophagus decreases, eating becomes difficult or impossible.
- Erosive - caused by acute infectious diseases or irritating substances that corrode the wall of the esophagus. In the erosive form, ulcers appear on the surface of the mucosa, which can subsequently lead to bleeding, suppuration and even rupture of the wall of the esophagus.
- Hemorrhagic – provoked by viruses and bacteria (typhus, influenza). A rare type of erosive form. It manifests itself as inflammation of the III-IV degree according to Bassett. In some cases, the mucous membrane peels off, severe bleeding and hematemesis may occur.
- Pseudomembranous - caused by bacteria and viruses (scarlet fever, diphtheria), fibrous exudate appears on the inner surface of the esophagus in these cases.
- Exfoliative – a consequence of a chemical burn (acid, alkali), the presence of sepsis. It can result in complications in the form of wall perforation or abscess.
- Necrotic - occurs as a reaction to infectious diseases - typhus, measles, uremia, scarlet fever. It is characterized by necrosis of large areas of the mucous membrane. When they are separated, deep ulcers appear that do not heal for a long time.
- Phlegmous - provoked by a mechanical effect on the esophagus, for example, it can occur when a foreign body gets stuck, an attempt to do esophagoscopy, etc. Expressed in diffuse purulent inflammation.
Depending on the location, esophagitis is also divided into total, proximal and distal sections of the esophagus. If you experience pain in the esophagus, burning sensation, or inability to swallow food, which is observed against the background of fever or general malaise, you must consult a doctor promptly. Timely prescribed therapy will allow you to get rid of unpleasant symptoms in 1-2 weeks (depending on the form of the disease).
The etiology and pathogenesis of chronic forms also differ. As a rule, they are caused by prolonged and regular exposure to negative factors on the esophagus:
- nutritional – with abuse of alcohol, hot and spicy foods;
- stagnant - occurs in the presence of stenosis of the esophagus and other diseases/damages in which food gets stuck in the esophagus and causes irritation;
- dysmetabolic – is a consequence of iron deficiency, for example, Plummer-Vinson syndrome, tissue hypoxia, portal hypertension;
- allergic – provoked by food allergies or bronchial asthma.
In addition to the listed types of chronic and acute esophagitis, there are a number of specific types, for example, idiopathic ulcerous esophagitis, granulomatosis of the esophagus, reflux esophagitis. Primary esophagitis (not caused by other diseases or abnormalities) occurs in only 0.3% of cases, secondary lesions are observed much more often. 80-90% of all cases are superficial forms; ulcerative or erosive esophagitis rarely occurs.
The causes of the disease in children include the same factors as in adults, however, the risk of inflammation in children increases, firstly, due to frequent infectious diseases, and secondly, due to careless handling of chemicals (for example, detergents). means).
In newborns, symptoms manifest themselves against the background of weakness of the lower sphincter, due to which acid from the stomach enters the esophagus, or weakness and immaturity of the entire neuromuscular system. The presence of the disease can be determined by restlessness and regular regurgitation. In adolescents, the cause may be asynchronous growth of the esophagus and trunk as a whole, or problems with the sphincters between the esophagus and stomach.
general characteristics
Esophagitis is the general name for all pathologies accompanied by inflammation of the esophageal mucosa. The disease is acute if inflammation occurs due to short-term exposure to aggressive environmental factors. However, it usually lasts from several days to a couple of weeks. If such exposure is constant, chronic esophagitis occurs, in some cases lasting for many years with periodic exacerbations. This occurs when stomach contents constantly enter the esophagus due to pathologies of the esophageal sphincter. In this case, the mucous membrane of the esophagus becomes inflamed, and erosions, hemorrhages, or areas of tissue necrosis may form on it.
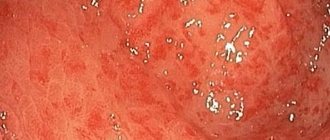
The mildest course of the disease is catarrhal superficial esophagitis. It is accompanied only by redness of the mucous membrane due to irritation by aggressive food, as well as slight swelling. The entire surface of the esophagus can become inflamed, but most often the disease affects its distal parts adjacent to the stomach.
This disease is quite common, it is believed that it occurs in every second person. But there are no exact statistical data on this, since patients rarely go to the doctor. After all, it is the catarrhal form of esophagitis that is most often secondary, appearing in other gastrointestinal pathologies. Therefore, doctors can attribute such inflammation to their symptoms, and not to a separate disease.
In this case, terminal esophagitis develops - inflammation of the mucous membrane of the lower esophagus. Most often it is a concomitant pathology with GERD - gastroesophageal reflux disease. The constant entry of stomach contents into the esophagus leads to irritation. At first, the inflammatory process does not develop, but without treatment, inflammation of the mucous membrane occurs over time. As a result of a chronic inflammatory process, the cells of the esophageal mucosa degenerate, which can result in the appearance of a malignant tumor.
Symptoms
Symptoms of the disease vary in detail depending on the morphological type, but common features can still be traced. There is pain when swallowing and at rest, burning, heartburn, lump in the throat, painful sensations in the mouth. In complicated cases, nausea and vomiting may occur. Patients note an unpleasant aftertaste, hoarseness, mouth ulcers, pain not only in the esophagus, but also in the sternum, radiating to the back, and bad breath. Symptoms and clinical picture are the basis for making a diagnosis of esophagitis; its form is clarified after research.
Diagnostics
Diagnostic procedures begin with examination and history taking. At this stage, it is possible to quite accurately determine the form and give recommendations on diet and pain relief, since the disease has clear clinical symptoms. To identify the extent and root cause of the disease, endoscopic or additional hardware examination may be indicated:
- upper endoscopy shows changes in the mucosa (the endoscope is inserted into the esophagus);
- esophagomanometry shows impaired motor functions of the esophagus;
- X-ray of the upper gastrointestinal tract with contrast - shows ulcers in an erosive or advanced necrotic form, their size and location.
To clarify the analysis, a histological examination can be used, which examines a biopsy specimen from the mucous membrane of the esophagus.
During the diagnostic process, it is important to identify the root cause of the disease against which it developed. Since pathology often manifests itself against the background of a bacterial and viral infection, without elimination it is impossible to successfully cope with the symptoms of the disease in question.
NEARMEDIC clinics are equipped with the necessary equipment to clarify the diagnosis. The appointment is conducted by a general practitioner, and in case of complicated forms, by a gastroenterologist. Patients are successfully treated in our clinics and receive advice on diet and lifestyle.
Answers to popular questions
- How to identify reflux esophagitis in a child?
Reflux occurs 3 times more often in children than in adults. The esophagus of babies has mechanisms to protect against the development of esophagitis, so this condition rarely develops in childhood. Its main symptoms are: causeless crying of the baby, increased anxiety after eating, increased body temperature, chest pain. The disease can be managed without medications. After each feeding, you need to hold the baby upright. If this does not help, then you need to use adapted formulas that have a thick consistency to feed the baby, for example, Nutrilon, Frisovo, Enfamila.
- How long does it take to be treated for reflux esophagitis?
Throughout your life you will need to follow recommendations regarding lifestyle and nutrition. The duration of taking the drugs is determined individually. As a rule, proton pump inhibitors are taken in a monthly course. They will need to be repeated 2 times a year.
- What is biliary reflux esophagitis?
If a person has diseases of the biliary tract and gallbladder, and also has weakness of the sphincters, this can lead to the reflux of duodenal contents into the esophagus. In this case, the organ will suffer from the destructive effects of bile. This disease is often combined with severe gastritis and peptic ulcers. Therapy is carried out according to a similar scheme. At the same time, it is important to additionally focus efforts on treating the biliary system.
- Can reflux esophagitis cause an esophageal ulcer or organ cancer?
If the disease exists for a long time without treatment, then the risk of developing these complications is extremely high.
Author of the article:
Gorshenina Elena Ivanovna |
Gastroenterologist Education: Diploma in General Medicine received from the Russian State Medical University named after. N. I. Pirogova (2005). Postgraduate course in the specialty "Gastroenterology" - educational and scientific medical ]Our authors[/anchor]
Treatment
Treatment, preventive measures, and diet are selected depending on the cause of the disease. Let's look at a few examples:
- if the causes of the development of the disease lie in infection, therapy begins with taking drugs that cope with it;
- for acid reflux, medication is selected depending on the type of reflux, for example, heartburn medications that suppress acid production;
- If a problem arises due to regular use of medications of a certain group, another drug is selected.
Treatment is performed either conservatively or surgically. Conservative treatment consists of taking medications (prokinetics, alginic acid, antisecretory drugs), physiotherapy (electrical stimulation of the cardia, electrophoresis with novocaine) and laser treatment (endoscopic laser therapy). Surgical intervention is used when conservative intervention does not produce the desired results. To avoid degeneration into oncology, surgical intervention is chosen for Barrett's esophagus, complications in the form of bleeding, and partial pneumonia.
Effective treatment is impossible without a proper diet. The diet is selected depending on what problems provoked the onset of the disease. For reflux, tomatoes, tea, coffee, citrus fruits and chocolate are prohibited. It is recommended to eat small meals, eat non-hot food without pronounced salty, spicy and sour tastes. It is necessary to choose soft foods that will easily pass through the inflamed esophagus.
Some foods can speed up the healing process, including mashed potatoes, rice porridge, oatmeal, buckwheat, egg whites, lean chicken, soups and broths, herbal and green tea.
What medications are prescribed for gastroduodenitis?
Phosphalugel will help protect the gastric mucosa.
If the attack is acute, then medications (as well as food) are not taken. However, there are exceptions. Which?
Drugs that can and even should be used during an acute attack include:
- activated carbon;
- adsorbents - substances that absorb and remove toxins from the stomach (Smecta and the like);
- “Kvamatel”, “Omeprazole” - drugs that help normalize the synthesis of hydrochloric acid, which helps reduce irritation in the stomach and relieves inflammation;
- "Maalox" and "Phosphalugel" have an enveloping effect and form a protective film on the gastric mucosa.
These drugs can improve the patient’s well-being and normalize the condition of the stomach and the body as a whole. There are severe cases in which gastric lavage and the use of a cleansing enema are effective.
Of course, in order to avoid complications, these manipulations should be prescribed by the attending physician. If indications for these procedures are given, then you can begin to perform them. An enema and gastric lavage will help quickly eliminate irritation on the walls of the stomach, which will significantly alleviate the patient’s condition.
Also, a patient with aggravated gastroduodenitis is placed on bed rest, sometimes this is done in a hospital setting. Bed rest helps stabilize a person’s physical and psychological condition, and observation in a hospital setting helps monitor the patient’s condition and well-being, as well as his compliance with all medical prescriptions.