Aerocolia is the presence of too much gas in the intestines.
• Bloating and a feeling of distension in the abdomen, appearing 1 hour after eating. • Flatulence, bloating and constipation; difficult passage of gases.
Aerocolia may be a consequence of ingesting food that causes increased gas formation (garlic, peas, cabbage, sweet foods, too many raw vegetables and fruits). It can be caused by too active bacteria in the intestines, leading to the accumulation of large amounts of gas. Often the cause may be intestinal infections and incipient gastroenteritis. Finally, aerocolia can be a consequence of constipation, intestinal obstruction or intestinal paralysis. It is often observed in restless, stressed people.
Treatment with herbs
The same types of plants are used as for aerogastria. Cumin, navel, peppermint, lemon balm, mixed in equal parts: infusion, 1 teaspoon per 1 cup of boiling water, add 2 drops of essential oil of caraway, cumin, coriander or cardamom or 50 drops of ginger extract. Take after meals.
– Choose a diet based on dairy products and easily digestible proteins (boiled fish, potatoes). – Avoid carbonated drinks and choose foods with little fiber. – Lead an active lifestyle, such as walking more. – Keep your bowel movements regular.
Source: https://na-info.ru/zametka/120-kak-raspoznat-i-lechit-aeroko.html
User comments
Aerocolia
Aerocolia is the formation and presence of excessive amounts of gas in the intestines. It is characterized by voluminous bloating, which appears approximately 1 hour after eating, as well as flatulence, constipation and difficulty passing gas.
Aerocolia can occur as a result of the use of https://www.zoovet.ru/text.php?newsid=607, which causes increased gas formation or excessive activity of intestinal bacteria, leading to the accumulation of a large amount of gas.
I think it happens to every second baby, but I don’t understand what the pelvic x-ray has to do with it.
Source: https://www.baby.ru/blogs/post/223528721-60936885/
Colitis of the intestines
- Causes
- Symptoms
- Classification
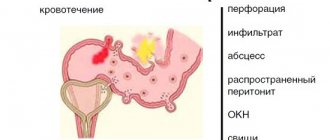
- Complications
- Treatment
- Video on the topic
Colitis is an inflammation of the large intestine. Among diseases of the gastrointestinal tract (GIT), pathology occupies a leading position in terms of prevalence. Intestinal colitis is considered a polyetiological disease, that is, a large number of reasons can lead to its development. Inflammation causes dystrophic changes in the intestinal wall.
The disease occurs more often in women than in men. The disease tends to become chronic in the absence of timely assistance. A bacterial infection, after contact with the mucous membrane of an organ, has a damaging effect. This causes swelling of the intestine and disruption of its functional activity.
Colitis can lead to the development of dangerous complications, which is why it is extremely important to detect the disease in time. What causes the disease, how does it manifest itself and how to deal with it correctly? We'll talk about all this and much more in this article.
Causes
The causes of intestinal colitis are divided into exogenous and endogenous. First, let's talk about the first group of provoking factors:
- parasites;
- infectious agents: viruses, mycobacterium tuberculosis, shigella, fungi;
- salmonellosis, dysentery;
- errors in nutrition. This includes eating dry food, addiction to alcohol, spicy, fatty, salty foods;
- exposure to mercury, arsenic, lead, heavy metal salts;
- dysbacteriosis;
- radiation exposure;
- passive lifestyle;
- mechanical damage to the intestines;
- chronic stress;
- uncontrolled use of antibiotics or laxatives.
Endogenous causes include the following:
- genetic factors;
- allergic reaction;
- hepatitis, liver cirrhosis, ulcer, pancreatitis;
- features of the anatomical structure of intestinal vessels;
- weakened immune system;
- autoimmune processes;
- impaired blood supply to the intestines;
- chronic liver and kidney diseases;
- intoxication.
Causes of reactive pancreatitis in children
Unlike adults, children more often react to infections and inflammations by disrupting the functioning of the pancreas.
The most typical causes of reactive pancreatitis in children are1:
- gross violation of diet;
- regular consumption of fatty and sweet foods, foods high in preservatives and dyes;
- long-term treatment with antibiotics;
- frequent ARVI, flu, colds;
- repeated infection with helminths;
- allergic reaction (to food or medicine);
- congenital pathologies of the gastrointestinal tract, contributing to the development of inflammation of the pancreas;
- stress, emotional overload.
Medical practice shows that the key causes of reactive pancreatitis in children are related to nutrition. Namely, with violation of his regime, introduction of harmful foods into the diet, and passion for fast food.
Products that can provoke reactive pancreatitis in children:
- fried foods (both vegetable and butter);
- fatty foods;
- smoked meats;
- spicy seasonings;
- fast food (burgers, chips, French fries, crackers);
- sweets with dyes and artificial additives;
- carbonated drinks;
- packaged juices.
Symptoms
Colitis in adults manifests itself in the form of general and local symptoms. General symptoms include signs of intoxication of the body:
- headache;
- irritability;
- sleep disturbance;
- temperature increase;
- chills;
- weakness, fatigue.
Loss of body weight and hypovitaminosis may also be observed. Local manifestations include abdominal pain. The painful outbreak is often dull and aching in nature and is localized in the lower and lateral parts of the abdominal cavity. A characteristic symptom is increased pain after eating and weakening after defecation.
Patients complain of bloating, heaviness in the abdomen, and rumbling. Depending on the cause and type of inflammatory process, patients suffer from diarrhea or constipation. Abdominal pain with intestinal colitis may intensify after a cleansing enema, when eating, as well as when walking and shaking while driving. Signs of colitis directly depend on the type of disease. Manifestations of acute and chronic forms have a number of differences.
The acute process is characterized by the appearance of the following symptoms:
- discomfort in the abdomen;
- diarrhea. There are streaks of blood and greenish streaks in the stool;
- false urge to defecate during the daytime. As the pathology progresses, this symptom appears at night, is accompanied by painful sensations and ends with the release of a small amount of hard feces;
- bloating in the abdomen;
- flatulence;
- heaviness in the stomach.
Chronic colitis causes increased gas formation even without eating specific foods. The disease manifests itself in the form of severe spastic constipation. About an hour after eating, there is a loud rumbling in the stomach.
The chronic process is characterized by changing stools, when diarrhea alternates with constipation. Patients complain of a feeling of fullness, heaviness in the stomach, nausea, vomiting, dizziness, weakness, and bitterness in the mouth. Inflammation of the colon occurs in three main stages:
- Initial. There are minor deviations from the norm. Thirst, skin rash, dry mouth, and irregular bowel movements appear.
- Average. An increase in clinical symptoms is observed. General malaise occurs and body temperature rises. Patients complain of cramping abdominal pain.
- Heavy. Occurs at high temperatures. In addition to severe abdominal pain, rapid heartbeat, ragged breathing, and pale skin are added.
results
The treatment strategy for children with different variants of SCM was determined in each case individually depending on the variant of SCM, age, nutritional status and identified complications. For the practical implementation of treatment protocols, the following algorithms were used.
1. Children 1 year of life ( n
=12) with various variants of SBS, but without surgical complications, were treated using a home PN system until the age of 1.5-2 years.
During the initial hospitalization, after eliminating various complications and stabilizing the patient’s condition, the variant of SCM was determined, permanent venous access was established, a scheme of parenteral and enteral nutrition was selected, caregivers were trained and adapted to the home PN system. Subsequently, online monitoring, correction of PP, prediction and preventive therapy of complications were carried out. Planned hospitalizations were carried out once every 6 months, unplanned hospitalizations were carried out in case of development of life-threatening complications. In the absence of signs of restoration of enteral autonomy, children aged 1 to 3 years ( n
= 10) underwent autologous intestinal reconstruction.
2. Children 1 year of life ( n
=4) with various variants of SCM in the presence of signs of intestinal obstruction, preoperative preparation was carried out in a shorter period of time in a hospital setting, followed by surgical treatment, including both elimination of the causes of intestinal obstruction and enteroplasty to lengthen the intestine.
3. Patients of different ages ( n
=18) without a tendency to achieve enteral autonomy after restoration of nutritional status and elimination of complications, surgical treatment was also performed.
4. Patients of different ages ( n
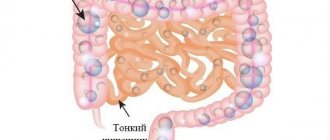
=6) with complex variants of SBS without clinically significant growth of the ultrashort small intestine and the expected effect of autologous reconstruction continue to receive long-term treatment according to the home P.P. system. The general scheme of treatment results for children with SCS is shown in Fig. 1.
Rice.
1. Results of treatment of children with short bowel syndrome (scheme). PN - parenteral nutrition; SBS - short bowel syndrome; STEP—sequential transverse enteroplasty; reSTEP - repeat enteroplasty; Bianchi's LILT - longitudinal lengthening and narrowing of the intestine using the Bianchi method. A total of 37 operations were performed on 32 patients with various variants of SCS: staged autologous reconstruction of reSTEP was performed on 5 patients with complex variants of the syndrome. In 1 case, enteroplasty was performed using the STEP method after an ineffective LILT operation using the Bianchi method.
The maximum number (20 out of 37) of autologous reconstruction operations was performed in 2015-2017, during the period when proven tactics for managing patients with SBS and the introduction of a home PN system made it possible to perform these operations “on the fly.” Surgical complications were noted in 2 (5.4%) patients: intestinal bleeding in the early postoperative period developed in a patient with an extensive abdominal hemangioma and was stopped conservatively; In the first patient, who underwent STEP enteroplasty without intubation of the reconstructed intestine, failure of one of the intestinal anastomoses was observed. The complication was eliminated by restoring the integrity of the anastomosis on the intubated colon.
Analysis of the results of autologous intestinal reconstruction operations was carried out in two time periods: in the mid-term observation period (12-24 months after surgery) and in the long-term period (>24 months after surgery).
A good result of the operation was considered to be a decrease in dependence on PN in the medium term and/or the formation of complete enteral autonomy in any period after surgery in the absence of signs of increasing nutritional deficiency and progression of complications caused by the pathophysiology of SBS. To date, 10 (31.3%) patients have achieved complete enteral autonomy after autologous intestinal reconstruction; in 13 (40.6%) children operated on over the past 2 years, PN reduction was achieved: they receive maintenance therapy 2-4 times a week in the home PN mode; another 4 (12.5%) patients with complex variants of SBS (more than 2 years after reconstruction) require reduced parenteral nutritional support, but without a tendency to restore enteral autonomy.
To estimate the time to achieve PP reduction and the occurrence of complete enteral autonomy, a survival analysis was performed using the Kaplan-Meier method.
The median (Me) reduction time was 8 months with a 95% confidence interval (CI) from 5.8 to 10.2 months. In Fig. 2 presented
Rice. 2. Kaplan-Meier curve: assessment of the time to achieve reduction of parenteral nutrition after autologous intestinal reconstruction. PN—parenteral nutrition. survival function to achieve reduction of P.P. It can be seen that the proportion of patients in whom reduction of the PP is achieved among all operated patients is approximately 30% by 20 months, and then remains virtually unchanged. The time required to achieve complete enteral autonomy was 32 months. From Fig. 3 is visible
Rice. 3. Kaplan-Meier curve: estimation of time to achieve enteral autonomy after autologous intestinal reconstruction. that by approximately this time the proportion of patients who have achieved enteral autonomy is about 45% and does not change subsequently.
Among the parameters that could be used as predictors of achieving enteral autonomy after surgery were the following: the patient's age at the time of autologous intestinal reconstruction; length of the small intestine before surgery; presence or absence of the colon; length of the small intestine after reconstruction; nature of complications before surgery.
When assessing the influence of age on the formation of enteral autonomy using the Mann-Whitney test, it was found that the statistical significance of the test was 0.273. Thus, it has been proven that age does not affect the formation of enteral autonomy. The impact of different types of preoperative complications (complications or no complications) on the achievement of enteral autonomy was assessed using the χ2 test of independence. No statistically significant effect of type 1 complications was found ( p
=0.919), as well as the 2nd (
p
=0.558) and 3rd (
p
=0.055) types.
According to the SCS variant, 2 groups of children were performed: in 18 (36%) patients, the length of the small intestine before surgery was less than 30 cm, in 32 (64%) - more than 30 cm; 38 (76%) had a completely or partially preserved colon and 12 (24%) children had no colon. According to the results of the χ2 test, the length of the small intestine before surgery influences the achievement of enteral autonomy ( p
=0.004, Cramer coefficient 0.48).
All patients with small bowel length less than 30 cm did not achieve complete enteral autonomy. The proportion of patients with small bowel length greater than 30 cm who achieved enteral autonomy was 56.5%. This difference in proportions is statistically significant by z test ( p
< 0.05).
The effect of the presence of a large intestine on the formation of enteral autonomy has not been statistically proven (χ2; p
= 0.156).
To analyze the nature of complications that occurred before and after surgery, a modification of the χ2 test for dependent samples was used - the McNemar test. In patients who underwent autologous intestinal reconstruction, a statistically significant ( p
<0.001) dynamics of reducing the number of complications of types 1 and 2.
The reduction in type 2 complications was not statistically confirmed ( p
= 0.581).
Catheter-associated blood infection caused deaths in 5 (11%) patients. The patients died at different times after successful autologous intestinal reconstruction; four of them were treated before the active introduction of the home PN system and were constantly in the hospital from the moment of birth.
Classification
Experts distinguish two main forms of colitis:
- spicy Characterized by progressive and intense pain syndrome. Certain symptoms do not subside even after taking an antispasmodic. Often accompanied by inflammatory processes in other organs of the gastrointestinal tract;
- chronic It usually develops in cases where timely actions to neutralize acute inflammation were not taken. It develops over a long period of time and can develop without clear clinical symptoms. Along with this, gradual destruction of the mucous membrane occurs. Chronic colitis occurs with frequent relapses.
Ulcerative
Ulcerative colitis is a chronic inflammation of the colon, which is characterized by the formation of ulcers and hemorrhages on the mucous membrane. The causes of the disease are not fully understood. There are several hypotheses regarding the occurrence of the disease: hereditary predisposition, infectious nature, autoimmune process.
Discussion
Multicomponent treatment of patients with short bowel syndrome allows us to develop an individual intestinal rehabilitation plan for each patient, taking into account age, variant of SBS, and somatic and surgical complications. It is optimal to manage patients with SBS by one “team” of specialists (nutrition support team, multidisciplinary team for the rehabilitation of patients with intestinal diseases, multidisciplinary intestinal rehabilitation team), adhering to a single treatment concept and carrying out multidisciplinary supervision [13, 14].
Long-term treatment within the framework of the home PN project makes it possible to wait-and-see for patients in the first years of life with hypothetically possible physiological growth of the small intestine in length and opens up prospects for children with complex variants of IBS who require long-term parenteral nutritional support. Undoubtedly, the desired outcome of treatment for children with SBS is the restoration of full enteral autonomy. In this regard, autologous intestinal reconstruction, which allows, on the one hand, to completely move away from PN and, on the other hand, to avoid intestinal transplantation, has great potential [15]. Currently, two methods of autologous intestinal reconstruction are widely used - STEP (Serial Transverse EnteroPlasty, sequential transverse enteroplasty) and LILT (the Longitudinal Intestinal Lengthening and Tailoring, longitudinal lengthening and narrowing of the intestine, Bianchi operation), the result of which is the lengthening of the residual intestine by an average of 70% [16] with restoration of enteral autonomy in 47 and 55% of cases, respectively [15-18]. According to foreign authors [19—21], the time to achieve enteral autonomy is approximately 21 months after surgery using the STEP method and 18 months after surgery using the LILT method.
Our 12-year experience shows the promise of the STEP technique, which we perform in our modification, which helps to minimize a number of surgical complications and unhindered performance of repeated reconstructions in patients with complex variants of SCC.
The length of the residual small intestine has a statistically significant effect on the achievement of enteral autonomy: patients with a preoperative length of the small intestine of less than 30 cm remain dependent on parenteral nutritional support, although we achieve reduction of the PP. Despite the unproven impact of the presence of a colon on the restoration of enteral autonomy, in clinical practice we note more promise in patients with SBS and the presence of at least half of the colon. To date, 3 out of 4 patients receiving PN for more than 2 years after surgery have a reconstructed small bowel length of 80 to 200 cm in the absence of colon and remain dependent on fluid therapy and PN.
It is important that the main causes of death in patients with SBS are catheter-associated blood infection [22, 23] and liver diseases associated with intestinal damage (IFALD, Intestinal Failure Associated Liver Disease) [24]. The latter have a multifactorial genesis: in addition to phytosterols contained in 1st generation fat emulsions and being the main cause of the development of intrahepatic cholestasis, recurrent infectious processes also play a significant role [25, 26]. Thus, a statistically significant reduction in the number of life-threatening complications after autologous intestinal reconstruction emphasizes the importance and necessity of the surgical stage of treatment of SBS.
Treatment
Treatment of intestinal colitis includes not only the use of medications, but also adherence to a strict diet, which will be prescribed individually by a gastroenterologist. Supportive assistance is provided by folk remedies that work well against the clinical manifestations of colitis.
If the cause of inflammation is an infectious process, patients are prescribed antibiotics. When identifying parasites, you cannot do without anthelmintic drugs. Doctors often prescribe painkillers for intense pain. Colitis is accompanied by stool disturbances, so the treatment complex includes means to normalize stool. For diarrhea, astringent medications are used.
A decoction of oak bark, tanalbin, and white clay have binding properties. For constipation, laxatives and cleansing clay are indicated. Probiotics are used to normalize intestinal microflora. They populate the body with beneficial bacteria that fight pathogens. This helps restore the natural qualitative and quantitative balance of the flora.
Why is it important to see a doctor at the first symptoms?
Adhesive disease is dangerous and often goes unnoticed until it develops into a pathology that is difficult to reverse.
If you have a history of surgeries, abdominal injuries, congenital intestinal abnormalities, or an umbilical hernia, then you should not be ashamed of constipation, bloating and other delicate signs of the disease. You shouldn’t rely on folk remedies either - in the case of adhesions, they will only relieve the symptoms for a short time and give time for the strands to grow even deeper. The Yusupov Hospital provides a full range of medical services, including inpatient treatment, examination, surgery and rehabilitation. Diagnostic procedures of any level of complexity are provided. An individual approach is provided to each patient, which guarantees positive dynamics in treatment.
To make an initial appointment with a specialist, call the numbers listed on the website or fill out a standard online form, leaving contact information for feedback.
Symptoms and Treatment
Erosive intestinal colitis is a pathological process during which inflammatory damage to the mucous membrane of the stomach and duodenum occurs. This disease is characterized by the formation of ulcerative tumors on the mucous membranes of the internal organs of the human gastrointestinal tract. Erosive colitis is considered a more common and dangerous pathological process compared to any other diseases of the human digestive system.
This gastrointestinal disease can occur in both acute and chronic forms. The latter is considered the most dangerous because with the development of a chronic inflammatory process without the necessary medical care, gastric ulcers can develop. In addition, the duodenum adjacent to the stomach can also be affected by ulcerative tumors.
Treatment options
The main vector of action in the treatment of intestinal adhesions is the return of the normal location and functionality of intestinal loops by separating adhesions and removing severely affected areas.
It is performed surgically - open or laparoscopic methods. Loose adhesions are separated bluntly, while denser and vascularized adhesions are separated using instruments followed by suturing. If an area of the intestine is irreversibly damaged by adhesions, this conglomerate is completely removed, and the wall is sutured with maximum preservation of the anatomical shape. Areas of affected damaged organs may also be excised.
The use of a nasointestinal tube is indispensable in the treatment of intestinal adhesions. The main objective of using this method is to straighten, eliminate obstruction, and restore normal blood circulation in the intestinal wall. The use of a probe accelerates the healing process, stimulates the return of motility and other functional abilities to the affected intestine. The probe is inserted during the operation jointly by the surgeon and the anesthesiologist through the nasopharynx, esophagus, into the stomach cavity, duodenum and directly into the intestine. It causes some discomfort to the patient, but speeds up recovery. Usually placed for 3-5 days. Maximum 7. The decision to withdraw is made by the attending physician based on observation and the results of clinical studies.
Forms of the disease and its causes
Depending on the factors that caused inflammation of the gastrointestinal mucosa, the following main forms of the pathological process are distinguished:
- nonspecific ulcerative colitis (UC) - occurs as a result of poor nutrition;
- ischemic colitis - formed as a result of damage to any pathology of the human vascular system;
- infectious colitis - occurs when there are various infectious diseases in the human body;
- radiation colitis - is a consequence of prolonged exposure to background radiation on the human body;
- toxic colitis - can occur due to the use of certain medications or exposure to any chemical substances on the body.
Based on this, the main etiological factors that contribute to the development of colitis are:
- unhealthy diet, which consists of excessive consumption of smoked, fatty, salty and spicy foods. In addition, the development of colitis is facilitated by constant overeating, especially at night, as well as failure to adhere to the correct diet during the day;
- abuse of strong alcoholic drinks and smoking;
- the presence of any congenital pathologies of the intestinal tract;
- long-term use of various antibacterial and other medications that have a detrimental effect on the microflora of the gastrointestinal tract;
- the presence in the human body of any pathological processes in the gastrointestinal tract of a chronic nature, such as gastritis and lack of production of digestive enzymes by the pancreas;
- the impact on the human body of constant stress and nervous tension;
- autoimmune disorders that are accompanied by the occurrence of chronic allergic reactions;
- the presence of any parasitic infestations in the body;
- the occurrence of various types of intestinal infections, such as salmonellosis, shigellosis and yersiniosis.
In addition, inflammation of the mucous membrane of the intestine and duodenum can occur as a result of mechanical damage to these internal organs, which, in turn, can form as a result of the action of various pathogenic microorganisms on the mucous membrane of these organs.
Material and methods
The retro- and prospective cohort study presented in the article contains an analysis of the results of treatment of 45 children with SBS aged from 1 month to 17 years, who received and are receiving treatment in the Department of Surgery No. 2 of the Russian Children's Clinical Hospital of the Federal State Budgetary Educational Institution of Higher Education "Russian National Research Medical University named after. N.I. Pirogov" of the Russian Ministry of Health over the past 12 years. The study included only those patients with SBS who, after initial surgical interventions and/or their complications, required long-term (more than 6 months) parenteral nutrition (PN), including home PN.
At the time of initial admission to the clinic, children of the 1st year of life made up 58% of the total number of observations. Girls predominated among the patients—the boys:girls ratio was 17:28.
Depending on the type of SCM that arose after initial operations, patients were divided into four groups: group 1 ( n
=16) - small intestine shorter than or equal to 30 cm with completely or partially intact colon;
Group 2 ( n
=2) - small intestine shorter than or equal to 30 cm, with a complete absence of the large intestine;
Group 3 ( n
=20) - small intestine longer than 30 cm with completely or partially intact colon;
Group 4 ( n
=7) - small intestine longer than 30 cm with complete absence of large intestine.
The development of SCC in most cases is caused by congenital anomalies of the intestinal tube ( n
=35), in 3 of them - in combination with gastroschisis. There were also more rare causes: mesenteric thrombosis against the background of an extensive infantile hemangioma of the abdominal cavity (1 child), mesenteric thrombosis as a consequence of an undifferentiated form of connective tissue dysplasia with aneurysmal-stenotic lesions of the vessels of the abdominal cavity (1); mesenteric thrombosis, which complicated operations on the abdominal and retroperitoneal organs (3). In 5 patients, SBS arose as a result of extensive intestinal resections caused by necrotizing enterocolitis of newborns.
All patients before admission to the Department of Surgery No. 2 of the Russian Children's Clinical Hospital of the Federal State Budgetary Educational Institution of Higher Education "Russian National Research Medical University named after. N.I. Pirogov" of the Ministry of Health of the Russian Federation. operated on. The average number of operations was 3 (range 1 to 15). The most common reasons for repeated operations after initial resections were intestinal perforation, failure of the created anastomoses, and intestinal obstruction of various origins. Six patients were operated on 4 times or more due to various surgical complications. The number of patients with an ostomy at the time of initial hospitalization was 16 (35.6%). At all stages of treatment of children with SBS, the diagnostic algorithm consisted of 3 main components: analysis of nutritional status; assessment of the anatomical and functional state of the gastrointestinal tract; identification and prediction of possible complications.
Nutritional status was assessed using anthropometric data, energy requirements and diet. To analyze anthropometric indicators (height, body weight and body mass index), the World Health Organization (WHO) programs WHO Anthro for children under 5 years of age and WHO AnthroPlus for children from 5 to 19 years of age were used.
When forming a clinical diagnosis, we used the following classification of nutritional status disorders, proposed in 1992 by C. Waterlow, modified by B. Koletzko [5] (Table 1).
Table 1. Classification of nutritional status disorders [5]
In the absence of a daily opportunity to use a metabolograph, energy calculations for patients with nutritional deficiency of II and III degrees were carried out according to the formula recommended for determining the general energy needs of seriously ill children: resting energy expenditure (REE) × 2 ± 0.3 (kcal/day) [5 ]. REE was calculated using the W. Schofield formula.
To assess the anatomical and functional state of the gastrointestinal tract, radiopaque methods of visualization of the intestine were used (x-ray contrast study of the gastrointestinal tract with delayed images, irrigography), examination of the mucous membrane of different parts of the gastrointestinal tract (fibroesophagogastroduodenojeunoscopy with biopsy of the jejunal mucosa), and the absorption capacity of the intestine was studied (the level of citrulline in a dry drop of blood using the tandem mass spectrometry (TMS) and morphometric indicators of intestinal adaptation.
Typical complications for patients with SBS are grouped as follows: complications of the 1st type - catheter-associated complications, type 2 - complications associated with the treatment (liver diseases associated with intestinal damage: intrahepatic cholestasis, refeeding syndrome, invasive candidiasis , consequences of repeated catheterization of the central veins), type 3 - complications caused by the pathophysiology of SBS.
Adequate nutritional support was considered the basis of treatment for children with SBS at all stages. PN and enteral nutrition were selected for each individual patient individually, based on recommendations for therapeutic nutrition [1, 5–12]. We used both individually prepared bags with PP and infusion solutions, and ready-made multi-chamber containers with mandatory subsidies of complexes of vitamins and microelements.
Enteral nutrition for patients older than 6 months most often corresponded to the following scheme: basic oral feedings on an individually designed diet, siping of oral rehydration solutions and nutritional mixtures during the waking period, fractional nightly administration of nutritional mixtures through a gastrostomy tube for patients with a gastrostomy tube (12). The question of the possibility of introducing certain food ingredients into the diet was decided personally, trying to make it more diverse and eliminate mononutrition with specialized mixtures.
The process of adaptation of the caring parent to the home PN system lasted from 1 to 4 months. Training took place on the basis of the department during hospitalization and included the basics of PN, care of a device for permanent venous access, principles of feeding through a gastrostomy tube and its care. At the same time, a conclusion was drawn up from the medical commission, containing information about the monthly need for medications, consumables, elements of parenteral and specialized enteral nutrition to organize the supply of the patient at his place of residence.
Surgical treatment consisted of autologous intestinal reconstruction. The term “autologous intestinal reconstruction” means a combination of techniques for lengthening the small intestine or their modifications with other reconstructive operations, which together lead not only to an increase in the absorptive surface of the small intestine, but also to the elimination of other complications of SBS and/or combined gastrointestinal pathology. The main type of operation we use to lengthen the small intestine is “sequential transverse enteroplasty” (Serial Transverse EnteroPlasty, STEP), which we perform in our modification. This modification includes mandatory intubation of the reconstructed intestine through a gastrostomy, manual suture with a monofilament thread, the beginning of the formation of anastomoses immediately behind the duodenal bulb in ultra-short variants of SCC, the formation of anti-reflux valves at the sites of small-colic anastomoses.
Statistical processing of the research results was carried out using the IBM SPSS Statistics 21 program. For indicators with a close to normal distribution, the arithmetic mean and standard deviation were used as measures of descriptive statistics, and for heterogeneous data and small samples, the median and interquartile range were used. To establish patterns, the following methods were used: χ2 test of independence; z test to compare proportions; Mann-Whitney test; McNemar test; Survival analysis using the Kaplan-Meier method. The critical level of statistical significance for testing the null statistical hypothesis was taken equal to 0.05.
Signs of pathology
The symptoms of erosive colitis are not specific and, therefore, may be similar to the symptoms of other diseases of the gastrointestinal tract.
But in any case, you should consult a doctor if the following symptoms appear:
- painful sensations in the abdominal area. Due to the fact that erosive colitis in most cases is localized in the area of the sigmoid colon, it can prick in the lower left part of the peritoneum;
- severe nausea accompanied by frequent vomiting;
- the appearance of an unpleasant taste in the mouth, most often bitter;
- loss of appetite;
- a feeling of heaviness in the stomach and incomplete bowel movements;
- a disorder of the digestive system, which is expressed in the form of stool disorders;
- the presence of blood streaks in the stool. The amount of blood observed depends entirely on how large an area of the internal organ is affected by the inflammatory process;
- symptoms of poisoning of the body, such as fatigue, weakness, change from normal skin tone to pale and increased body temperature;
- flatulence - excessive formation of gases in the gastrointestinal tract, which is expressed in the form of bloating.
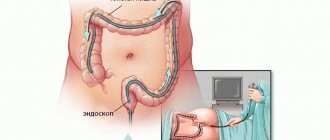
Diagnostics
Adhesive processes can be asymptomatic. The doctor should be alerted by complaints of problems with stool (constipation or diarrhea), bloating, belching, early satiety, pain in the intestines, painful bowel movements, infertility in women, a history of abdominal surgery, umbilical hernia.
There are no laboratory tests to determine adhesions. To establish a diagnosis, clinical studies are carried out:
- X-ray with contrast agent;
- ultrasonography;
- CT scan;
- colonoscopy;
- laparoscopy.
Methods for diagnosing inflammation of the mucous membranes of the gastrointestinal tract
The method of diagnostic examination to detect the presence of erosive colitis in the human body consists of conducting laboratory and instrumental studies.
These include:
- taking a general blood test. Carrying out this laboratory test allows us to detect in the blood of a sick person the presence of signs of intoxication of the body, characteristic of the development of erosive colitis;
- bacterial culture. Makes it possible to detect the presence of any pathogenic microorganisms of an infectious nature in the human body;
- macroscopic and microscopic examination of feces. Using this laboratory analysis, it is possible to estimate the concentration of mucus, blood and remnants of undigested pieces of food in the test sample of feces;
- examination of stool for the presence of parasitic microorganisms. Makes it possible to detect the development of certain helminthic infestations in the human body;
- colonoscopy. Using this instrumental diagnostic method, you can visually assess the condition of the mucous membranes of the gastrointestinal tract;
Treatment of the pathological process
If a person is diagnosed with erosive intestinal colitis, treatment primarily depends on the form of the pathological process. The course of therapy can be surgical or conservative, however, whatever the treatment method, it must necessarily include the use of special dietary nutrition.
As a conservative treatment, the patient is prescribed medications to relieve the symptomatic manifestations of the disease, such as pain. In these cases, various types of analgesic drugs are used. To relieve inflammation of the gastrointestinal mucosa and speed up their regeneration, immunosuppressive medications, such as corticosteroids and cytostatics, are used. The dosage and method of use of these drugs are prescribed only by a doctor individually for each patient.
If the use of local therapy does not have the desired effect, then the patient is prescribed a surgical operation during which the affected parts of the intestine are removed.
Source: https://niz-info-spravki.ru/ajerokolija-kishechnika-prichiny-i-lechenie/
topics of questions
- Hi-Tech Other
- Components and accessories
- Computers
- Cell phones
- Laptops
- Office equipment
- Software
- Repair and service
- Photo and video equipment
- Car loans
- For women
- IFRS
- Weight
- Copyright
- Spring
- Pregnancy
- Household chemicals
- Upbringing
- Women Health
- Safety
- Other
- Leisure
- Other
- Accessories
- Higher education
- Rent
- State
- Depression and stress
- Air travel
- Earnings
- Diseases and pests
- Parenting
- Martial arts
- Interior renovation
- Documentation
- Banks
- Hand-made
How to recognize and treat aerocolia?
Aerocolia is the presence of very large amounts of gases in the intestinal tract.
• Bloating and a feeling of distension in the abdomen, appearing 1 hour after eating. • Flatulence, bloated tummy and constipation; difficult passage of gases.
Aerocolia may be a consequence of ingesting food that causes increased gas formation (garlic, peas, cabbage, sweet foods, very large amounts of raw vegetables and fruits). It can be caused by very active microbial activity in the intestinal tract, leading to the accumulation of huge amounts of gases. Digestive infections and incipient gastroenteritis can often be a prerequisite. Ultimately, aerocolia can be a consequence of constipation, digestive obstruction, or paralysis of the intestinal tract. It is often observed in restless, stressed people.
Healing with herbs
The same types of plants are used as for aerogastria. Cumin, navel, peppermint, lemon balm, mixed in equal parts: infusion, 1 teaspoon per 1 cup of boiling water, add 2 drops of essential oil of caraway, cumin, coriander or cardamom or 50 drops of ginger extract. Take after meals.
- Choose a diet based on milk products and easily digestible proteins (boiled fish, potatoes). - Beware of carbonated drinks and choose foods with little plant fiber. — Lead an active lifestyle, for example, walk more. - Watch for regular bowel movements.
Materials provided from the website www.otvetin.ru
If you find an error, please select a piece of text and press Ctrl+Enter.