Diverticular disease (diverticulosis) is characterized by a hidden, insidious course of this disease, when, against the background of complete well-being, a person suddenly finds himself in a hospital bed in intensive care wards and, often, in the operating room. The reason for this situation is diverticular disease with a complicated course.
Currently, it remains the topic of numerous discussions, seminars, and conferences, due to the fact that the problem has not been completely resolved.
Many problems can be avoided if a person understands what diverticular disease is, whether he is at risk for diverticulosis, and how to prevent the development of the disease and its complications.
In this section, we will try to analyze in more detail what is included in the concept of diverticular disease, what are the most acceptable methods for diagnosing and treating the disease, and methods for preventing complications.
Epidemiology
Applicable to Russia and the former USSR, one can note the rapid increase in the incidence of diverticular disease. In 1970, the incidence of the disease did not exceed 2-3 per 100 thousand population. In 1979, this number increased almost 6 times. According to data published by the State Research Center in 2002, the number of diverticulosis detected during X-ray examination was 14.2% of all coloproctological patients, and already in 2012 this figure doubled and amounted to 28.8%.
The growth of this disease is clearly visible along with the process of industrialization and urbanization due to changes in people’s way of life, lifestyle and nutrition. A decrease in the amount of dietary fiber consumed, a large amount of carbohydrate foods and consumption of red meat led to a significant jump in cases of diverticulosis.
In contrast, in developing agricultural countries, diverticular disease is characterized by isolated cases, which is determined by the nature of the diet, which includes a significant amount of plant foods.
The aging of society is another reason for the increase in the incidence of diverticular disease. It is noted that under the age of 40 years, the risk of developing diverticulosis varies between 5-10%. Whereas at the age of 60 years, the percentage of detected cases of the disease is already 30%, and by the age of 80 it exceeds 66%.
Thus, diverticular disease was, is and remains a serious problem posing difficult challenges for doctors and patients.
To understand the term diverticular disease, a brief description of the anatomy of the colon is necessary.
Indications for irrigoscopy
The following indications for irrigoscopy are distinguished:
- bleeding from the anus;
- pain in the intestines;
- mucous or purulent discharge from the intestines;
- problems with bowel movements;
It is recommended to perform irrigoscopy if colonoscopy does not give accurate results. X-ray diagnostics reveal various symptoms of diverticulitis. The size of the formations in diameter does not exceed 10 centimeters. If the protrusions are single, it is much easier to cure the pathology. Multiple protrusions extend beyond the contour of the intestine. In the presence of inflammation, the edges of the diverticula have irregularities.
When a diverticulum ruptures, a fistula forms on the surface of the intestine. This complication is demonstrated both during irrigoscopy and colonoscopy. Often, during inflammation, adhesions form from the connective tissue, which affect the narrowing of the intestines.
Anatomy of the colon
The colon consists of the following sections: cecum, ascending colon, transverse colon, descending colon, sigmoid colon. The cecum has the widest lumen, and the sigmoid colon has the smallest. The junction of the sigmoid colon and the rectum is designated as the rectosigmoid junction. It is important to note that this section of the intestine has the narrowest diameter.
The wall of the colon consists of three layers: serous, muscular and mucous. The function of the mucous membrane of the colon is the absorption of water, the formation of feces, preparing them for evacuation by secreting a large amount of mucus and the synthesis of vitamins B and K. Under the epithelium of the colon mucosa there is a submucosa, represented by loose fibrous connective tissue in which blood vessels and lymphatic vessels and submucosal nerve plexus.
The muscular layer has a frame function and is responsible for the progressive movement of feces to the rectum. The muscular layer consists of a continuous inner circular layer, divided into three ribbons of the outer longitudinal layer.
The serous membrane consists of a connective tissue base covered with mesothelium, into which outgrowths of adipose tissue, the so-called fat pads, penetrate from the muscular layer.
Indications for colonoscopy
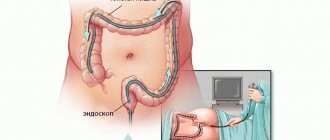
Colonoscopy is performed if there is a suspicion of cancer, ulcer or diverticulitis. Diagnostic testing also helps to diagnose the cause of internal intestinal bleeding, gastrointestinal disorders, and inflammation of the colon.
Colonoscopy is performed to detect deformation of the mouth of the diverticulum, an inflammatory or infectious process. The screen clearly demonstrates the presence of redness, swelling, and dilated blood vessels. The procedure determines the location of bleeding and determines the intensity.
What is intestinal diverticulum?
Diverticula are pouch-shaped protrusions of the intestinal wall that form in “weak” areas of the intestinal wall. There are true diverticula, which have all layers of the intestinal wall in their structure, and false ones, in which there is no muscle layer.
The diverticulum is divided into the mouth, the neck, the body and the bottom of the diverticulum. The blood supply to the diverticulum is carried out from the vessels of the submucosal layer from which thin vascular branches extend, piercing the intestinal wall and heading to the bottom of the diverticulum.
When a diverticulum forms in the projection of the fatty suspension and mesentery of the colon, it is covered on the outside with adipose tissue; when a diverticulum forms in the free edge of the intestinal wall, it is covered on the outside only with a serous membrane.
Based on the number, a single diverticulum and multiple diverticula of the colon are distinguished.
Based on the location of diverticula, right-sided, left-sided and total damage to the colon is distinguished.
Diverticulosis of right-sided localization, as a rule, is congenital in nature with a predominance of true diverticula.
With left-sided localization, diverticulosis is in most cases acquired and there is no muscle layer in the structure of diverticula.
Symptoms of diverticulitis
When the disease begins, there are no symptoms in most cases. Only when the disease enters the chronic stage do signs appear by which it can be identified. Among the warning signs indicating problems are:
- Bloating, excessive gas formation.
- Traces of blood in the stool.
- Increased body temperature.
- Pain in the lower abdomen and back.
- Nausea, vomiting.
- Decreased appetite.
- Cold sweat.
Causes of diverticulosis
The reasons for the development of diverticular disease remain a topic of much debate to this day. There are several theories about the occurrence of diverticula.
The most likely and most often discussed reasons include: increased intraluminal pressure in the intestine, increasing weakness of the intestinal wall, impaired colon motility and congenital predisposition.
Increased intraluminal pressure in the intestine:
Currently, the most recognized factor in the occurrence of diverticulosis is food. A decrease in the proper amount of plant fiber in the diet reduces the volume of feces, which in turn leads to a disruption in their evacuation with an increase in intraluminal pressure in the intestine. The evidence base is based on observations of vegetarians and residents of agricultural countries who consume significant quantities of fiber, in whom the incidence of diverticula is 42% lower than in a group of people who do not consume plant fiber in sufficient quantities.
Increasing weakness of the intestinal wall:
The fact that diverticula appear in old age confirms the theory of weakness of the intestinal wall, which is a consequence of the aging process of the body, when degenerative changes in muscle tissue and collagen fibers develop in the intestinal wall.
Colon motility disorders:
Impaired intestinal motility leads to constipation and increased pressure in the intestinal lumen when it is necessary to evacuate feces. Loss of elasticity of the intestinal wall leads, when it is stretched, to micro-tears of the circular muscles, through which diverticula begin to form.
Vascular disorders in the intestinal wall:
It is impossible not to indicate the vascular component in the formation of a diverticulum. Impaired blood supply leads to structural changes in the intestinal wall, while at the site where the vessel passes through the muscular layer to the intestine, an expansion is formed, which over time transforms into the mouth of a diverticulum.
Congenital predisposition:
Various congenital systemic connective tissue diseases and collagenoses are a provoking factor in the development of diverticular disease.
Localization of diverticulitis
The disease can affect different parts of the intestine:
- Diverticulitis of the small intestine
is multiple protrusions of the mucous membrane through weak spots in the walls. In this area, diverticula appear much less frequently than in the colon. The cause is considered to be a failure of peristalsis. - Diverticulitis of the large intestine
- formations up to two centimeters, often affects elderly patients. The reason is poor nutrition, the predominance of animal food over plant food. - Diverticulitis of the sigmoid colon
is a degenerative tissue disorder that appears as a result of impaired peristalsis and vascular pathologies.
Diagnosis of diverticulosis
Irrigoscopy:
One of the most accessible diagnostic methods is irrigoscopy, which allows one to reliably identify the location, size and number of diverticula.
! This method is not recommended for use in complicated cases due to the high risk of perforation of the inflamed diverticulum.
Colonoscopy:
A method that allows you to visualize diverticula and identify complications is colonoscopy. With this procedure, it is possible to fairly reliably diagnose inflammatory changes in the area of the mouth of the diverticulum and detect bleeding from the diverticulum.
! This method cannot be recommended as a mandatory procedure if the patient has a clinical picture of acute surgical disease of the abdominal organs.
Multislice computed tomography:
The safest method for diagnosing diverticular disease, both during the latent period and when diagnosing complications, is computed tomography, which allows not only to confirm the presence of diverticula in the patient, but also to determine the nature of the complications. These include acute diverticulitis with perforation, abscess, and peritonitis.
! Despite its safety, this method is used to a limited extent due to the high cost of the study and inaccessibility due to the lack of MSCT equipment in a number of hospitals.
Ultrasonography (ultrasound of the abdominal cavity):
An effective and accessible method for diagnosing complications of diverticular disease, it allows us to identify inflammatory changes in the wall of the colon, signs of abscess and peritonitis.
Laparoscopy:
Among the invasive methods for diagnosing complications of diverticular disease, laparoscopy should be noted, which can be considered not only as a diagnostic procedure, but also of a therapeutic nature. With this method, it is possible to perform sanitation measures for local peritonitis, drainage of the abdominal cavity.
Treatment of the disease
There is resolution of diverticulitis without special treatment due to normalization of nutrition and diet. In case of a serious stage of the disease, how to treat it is determined individually and often in a hospital. In this case, the patient is given antibiotics and other supportive medications. The operation is performed to separate the affected part of the intestine. This measure is rarely required:
- If the disease is very advanced. There are fistulas, perforations, abscesses.
- When antibiotics do not help get rid of the problem.
- Bleeding and peritonitis are observed.
The mechanism of development of complications of diverticulum
Diverticular disease is a progressive disease. Diverticula do not undergo reverse development. The risk of developing diverticulitis after a diverticulum persists for 5 years is approximately 10%. If the disease lasts more than 10 years, the risk increases to 25%.
Diverticulitis:
With diverticular disease, inflammatory changes develop in the wall of the diverticulum. The absence of a muscle layer leads to the fact that intestinal contents stagnate in them without the possibility of evacuation. This leads to the formation of fecalitis (fecal stone) in the lumen of the diverticulum, followed by inflammation in the wall of the diverticulum.
Diverticulum perforation:
Inflammatory changes may be limited to the diverticulum wall with its swelling and infiltration. With aggressive microbial flora, inflammation takes a malignant course and can lead to perforation of the diverticulum wall, which in turn can be delimited by the adjacent fatty tissue of the intestinal suspension or mesentery with the formation of an abscess.
Violation of the integrity of the diverticulum wall can lead to serious complications in the form of peritonitis when the diverticulum is localized on the free edge of the intestine.
Relapses of diverticulitis:
When acute inflammation is relieved, restoration of the diverticulum wall does not occur. The damaged mucosa is replaced by granulation tissue, coming into close contact with the tissues surrounding the diverticulum, creating favorable conditions for a chronic inflammatory process and subsequent relapses of acute diverticulitis.
Bleeding from a diverticulum:
Damage to the inflamed mucous membrane of the diverticulum by fecalitis when it comes out of the mouth or the development of a bedsore can lead to bleeding.
Fistula formation:
When inflammatory changes spread to nearby abdominal organs and/or the anterior abdominal wall, fistulas may form. Through such anastomoses, intestinal contents can spread into the lumen of the bladder, the uterine cavity, and even onto the anterior abdominal wall.
Risk factors
A predisposing factor for the occurrence of a protrusion (diverticulum) is a violation of the motor-evacuation function of the intestine:
- its constant overflow with frequent constipation;
- hardening of the intestinal contents (hard stool);
- structural features of the intestinal wall, weakness of the connective tissue framework;
- uncontrolled, unreasonable use of laxatives;
- previous gastrointestinal infections (dysentery, salmonellosis, etc.);
- obesity;
- excessive gas formation in the intestines, flatulence.
These events lead to prolapse of the weak section of the intestinal tube and the formation of a diverticulum.
Classification and treatment of complicated diverticular disease
To characterize the complicated course of diverticular disease, the Hinchey EJ classification proposed in 1978 is widely used.
! Only a DOCTOR can determine the nature of the complication and prescribe appropriate treatment. Do not self-medicate, this can lead to serious consequences!
Hinchey I.
Pericolic abscess or infiltrate: an acute condition caused by inflammation of the diverticulum with the possible formation of a limited abscess (abscess) in the mesentery of the colon or in its fatty suspension. Treatment of this complication is conservative and consists of prescribing a strict diet and antibacterial drugs.
Hinchey II.
Pelvic, intra-abdominal or retroperitoneal abscess. This condition is characterized by the formation of an abscess in a limited space in the abdominal cavity or in the peritoneal space outside the intestinal wall. Treatment consists of hospitalization in a surgical or coloproctology hospital, prescription of bed rest, strict diet, antibacterial therapy and detoxification treatment. If there is no effect, surgical treatment is indicated. As a rule, a sufficient volume of surgical intervention is puncture of the abscess for the purpose of its evacuation. However, if ineffective, emergency surgery is indicated to remove the source of purulent infection. At this stage of the disease, it is possible to perform a one-stage resection intervention with restoration of intestinal continuity.
Hinchey III.
Generalized purulent peritonitis. A serious complication that develops when an abscess breaks into the free abdominal cavity. Treatment is only surgical. In case of this complication, resection of the affected area of the colon is performed with the formation of a stoma, sanitation and drainage of the abdominal cavity. Subsequently, reconstructive intervention is performed aimed at restoring natural passage through the intestines.
Hinchey IV.
Generalized fecal peritonitis. The most severe complication that develops in advanced cases, when patients seek medical help late, in weakened patients, and in elderly people. The scope of surgery is similar to treatment for Hinchey III, but the postoperative period requires long-term intensive care in an intensive care unit.
Complications of diverticulosis and prevention
If the patient does not consult a gastroenterologist and does not decide together with a specialist how to treat diverticulosis, the risk of complications increases. Among them are inflammation of the diverticulum (diverticulitis) and the formation of infiltrate, the development of acute intestinal obstruction, intestinal perforation and perforation. In the chronic course of the disease, against the background of blurred symptoms, the formation of internal and sometimes external (extremely rare) fistulas is possible.
To prevent the appearance of diverticula or stop their progression, it is recommended to adhere to a balanced diet and drink at least 2 liters of water per day. Moderate physical activity aimed at accelerating peristalsis and improving digestion will also help to avoid stool thickening.
If diverticula do form, but do not cause significant discomfort, patients are advised to regularly visit a gastroenterologist (at least twice a year) and periodically undergo a complete intestinal diagnostics.
In conclusion, a brief overview of diverticulosis, its symptoms and complications:
Planned surgical treatment of diverticulosis
As a rule, after a single attack of diverticulitis, surgical treatment is not indicated, but may be recommended for persons under 45 years of age. The decision to perform an operation is made individually.
After successful conservative treatment of two or more episodes of diverticulitis, elective surgery is recommended. The indications for elective surgery are limited by the high anesthetic and surgical risks identified during examination of the patient.
Elective surgical treatment is mandatory after conservative treatment of complicated diverticulitis.
Planned surgical treatment is indicated in the presence of fistulas.
Which doctor should I contact?
Diverticulosis is a gastrointestinal disease, and treatment is most often carried out by a gastroenterologist. The primary task of the doctor is:
- Excluding diagnoses with similar symptoms;
- Purpose of examination;
- Determining a strategic approach to treatment.
During the treatment process, you may need to consult other specialists: a proctologist, a surgeon, a therapist, a pediatrician and geriatrician, an endoscopist and a nutritionist.