Causes of the disease
The cause of the disease is a violation of the natural outflow of bile. The secretion stagnates, corrodes the walls of the gallbladder, blood supply to tissues deteriorates, pathogenic microflora is activated. When the bile ducts become clogged with a stone, the patient becomes inflamed.
Factors that increase the likelihood of disease:
- obesity;
- sudden weight loss;
- starvation;
- long-term parenteral nutrition;
- taking medications belonging to the category of synthetic hormones, antibiotics (contraceptives, estrogen- and progesterone-containing drugs, ceftriaxone).
The likelihood of occurrence and exacerbation of the disease is observed during pregnancy and childbirth. Risk factors also include advanced and middle age, hereditary predisposition, a history of diabetes mellitus, liver cirrhosis, Crohn's disease, etc.
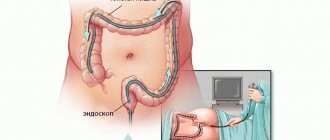
Diagnostics
A gastroenterologist can prescribe the necessary examinations for the patient. During the appointment, the doctor will ask the patient about complaints and study anamnestic information. A physical examination may reveal jaundice, bloating, and tenderness in certain areas of the body. Based on the data received, the doctor will prescribe the necessary instrumental and laboratory tests.
Necessary diagnostic procedures:
- Ultrasound examination of the gallbladder and bile ducts. The advantages of the method are safety and real-time imaging of organs. The doctor can immediately detect stones in the gallbladder, changes in the walls of the organ and other pathological signs indicating cholecystitis.
- Blood tests to identify inflammatory and infectious processes. With severe inflammation in the blood, the number of leukocytes increases. Also a diagnostic criterion is the concentration of liver enzymes.
- Collecting bile from an organ using duodenal intubation. The specialist sends the resulting material to the laboratory to detect pathogenic microflora.
- X-ray contrast examination of the gallbladder (cholecystography). The doctor receives information about the size, shape and functional activity of the organ. Using this study, you can detect anatomical abnormalities, gallstone disease or other ailments.
If the doctor is unable to make a diagnosis after requesting the results of the listed tests, an additional gastroscopy, computed tomography or survey laparoscopy may be prescribed. It is necessary to determine the cause of inflammation as accurately as possible.
Types of diseases and their symptoms
There are acute and chronic calculous cholecystitis. In the chronic form, symptoms manifest themselves moderately, discomfort occurs in the acute phase.
The chronic form is characterized by the following symptoms:
- Drawing, aching and dull pain in the right hypochondrium. The pain can radiate to the lower back, under the shoulder blade, right shoulder, or side of the neck.
- Hepatic colic is a symptom of the onset of an exacerbation of the disease. The patient experiences acute cramping pain in the right hypochondrium.
- Due to intoxication with bile acids, the patient exhibits signs of jaundice: the sclera, skin and mucous membranes become yellow, the urine darkens, and the feces become discolored.
- Gastrointestinal disorders: unstable stool, heartburn, belching, vomiting, bitter taste.
- Low-grade fever.
Acute calculous cholecystitis begins when stones block the bile ducts. As a result of obstruction, an inflammatory process begins, which is accompanied by severe symptoms:
- sharp pain in the right side;
- nausea, bouts of vomiting;
- increased temperature;
- weakness.
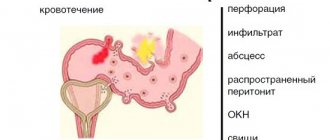
In an acute process, the injured mucous membrane secretes a larger amount of fluid, stretching the walls of the bile duct. In this case, inflammation intensifies and the likelihood of a secondary infection increases. An untreated acute process either worsens or subsides, as a result of which the gallbladder tissue degenerates and it ceases to fully cope with its functions. This is how the patient develops chronic cholecystitis.
The disease is also classified depending on the nature of the inflammation. There are the following types:
- purulent;
- catarrhal - the patient complains of severe pain in the right side of the body;
- phlegmonous calculous cholecystitis manifests itself in the form of increased pain when coughing and changing body position;
- gangrenous - a dangerous form that develops from phlegmonous;
- mixed type.
Treatment
For chronic cholecystitis, the main treatment method is a special diet that reduces the negative impact on the organ. Medications may be prescribed to eliminate infection and inflammation. If the disease causes dangerous complications, such as gallbladder gangrene or peritonitis, surgical intervention is necessary.
Main purposes:
- Therapy with a therapeutic diet. The patient needs frequent small meals. It is necessary to avoid constant consumption of fatty foods, alcohol, beans and fried meat. The diet should be followed for a long time to prevent relapse of the disease. When the gallbladder is removed, patients are prescribed a lifelong diet.
- Antibiotics and anti-inflammatory drugs. For chronic infection, it is recommended to obtain a sample of the microflora by probing and select an effective antimicrobial agent using a laboratory test.
- Antispasmodics and pain relievers to relieve symptoms.
- Choleretic medications. Medicines in this group are used to improve the excretion of bile into the duodenum.
Doctors include removal of the gallbladder or removal of stones blocking the ducts of the organ as the main methods of surgical treatment of cholecystitis. Severe complications of the disease may require complex open surgery in the abdominal cavity.
Medicines
Conservative treatment involves the use of broad-spectrum antibiotics (Norfloxacin, Cephalexin, Spiramycin) and intravenous administration of antispasmodics (No-Shpa, Papaverine, Spazmalgon).
To support digestive function, enzyme-containing supplements are used: Pancreatin, Mezim, Festal.
To support liver function, hepatoprotectors are indicated: Gepabene, Chofitol.
Doctors also recommend choleretic agents of natural origin Allochol, Cholenzym and sorbents Activated carbon, Atoxil, etc.
Diet after cholecystectomy
Patients operated on for calculous cholecystitis are prescribed a diet after surgery. In the absence of the gallbladder, which serves as a physiological reservoir, frequent unloading of the biliary tract is necessary. Therefore, the patient is forced to follow fractional meals throughout his entire life. Otherwise, stones may form again in the bubble stump or in the passages themselves. Meals should be at least 5-6 times a day.
After cholecystectomy, there is a deficiency of bile acids responsible for the digestion of fats. Therefore, it is necessary to exclude lard, lamb and beef fat from the menu. The consumption of fatty dairy products and butter should be limited. To compensate for the lack of lipids, more vegetable oil is included in the diet. It can be used to season porridges, salads, and vegetable purees.
Popular questions about calculous cholecystitis
What is calculous?
The term means that the cause of an acute or chronic inflammatory process lies in stones formed inside the gallbladder.
How much water should you drink if you have cholecystitis?
During an attack, it is recommended to drink as much mineral water as possible without carbon. Water is especially useful after a bout of vomiting.
What can you eat with acute cholecystitis?
Doctors recommend limiting food intake and eating foods that do not cause increased bile secretion.
Work of the organ
The gallbladder is an anatomical part of the liver. This sac-like organ is necessary for storing bile synthesized by liver cells and removing fluid into the small intestine during digestion. The release of bile into the cavity of the duodenum promotes the absorption of fatty foods and improved absorption of nutrients. There is a constant accumulation of secretion in the organ, leading to an increase in the viscosity of the fluid. After food enters the intestines, hormones stimulate the relaxation of special valves and the release of bile into the gastrointestinal tract through special ducts.
Other organ functions:
- Maintaining metabolism.
- Improving small intestinal motility.
- Release of excess cholesterol and bilirubin from the body.
- Activation of enzymes necessary for the absorption of protein foods.
The gallbladder is often subject to pathological influences. Disruption of the muscular lining of the organ can impede the secretion of bile - this process not only harms digestion, but also contributes to the formation of stones that can subsequently completely block the bile ducts and damage the internal lining of the gallbladder. Normally, the organ does not contain microflora, but with diseases and anatomical defects, pathogenic and conditionally pathogenic microorganisms from the intestine may penetrate into the gallbladder.
Diet therapy
Diet and nutrition directly affect the functioning of the biliary system. For diseases of the gallbladder and liver, therapeutic diet No. 5 is prescribed. The basic rules of such nutrition are fractionalization and rationality. The energy value of the diet must meet the individual needs of the body. The difference between therapeutic nutrition is the absence of choleretic products and difficult-to-digest foods. Fats are not completely excluded; it is preferable to consume them in the form of vegetable oils and butter. Simple carbohydrates are eliminated and the amount of fiber increases.
It is important to eat every two and a half hours and before bed. Hunger for more than 4 hours negatively affects the condition of the gallbladder. Portion sizes must correspond to the physiological needs of a person. It is important to avoid overeating. Errors in nutrition during cholelithiasis and chronic cholecystitis can cause exacerbation.
- fatty meat and fish, offal, rich broths;
- alcohol;
- strong coffee and tea, carbonated drinks, undiluted sour juices;
- vegetables with a high content of oxalic acid and essential oils: fresh garlic and onions, radishes, turnips, sorrel, spinach, white cabbage;
- sour fruits, berries;
- rye bread, baked goods, desserts with cream;
- chocolate, cocoa, snacks, nuts, mushrooms;
- legumes, corn, millet cereals.
Cooking methods are limited: fried and sautéed foods are excluded, preference is given to boiled and steamed food. If cholelithiasis occurs without symptoms, stewing and baking can be allowed.
During the period of exacerbation of cholecystitis, the diet becomes more strict. During an attack, the patient is advised to fast for one to two days. After stopping the attack, diet No. 5a is prescribed. Food is crushed and ground; porridges and vegetarian pureed soups are preferred. Dishes are served warm; cold and hot foods, which can cause spasm of the sphincter of Oddi, are excluded. In addition to the prohibitions of diet No. 5, fresh vegetables and fruits are excluded from the diet. Only boiling and steaming are allowed. Salt and sugar are limited as much as possible. Two weeks after the attack subsides, the patient can switch to a basic diet.
Mineral water therapy
Drinking treatment for cholecystitis has a beneficial effect on the functioning of the liver, effectively improves the composition of bile, helps normalize gallbladder motility, and cleanses the biliary system of inflammatory fluid. You can be treated in this way in a sanatorium and at home. Waters of low and medium mineralization containing magnesium, sodium, chlorine ions, and organic substances are useful. The choice depends on the state of the digestive system. For cholecystitis, it is recommended to take warm and hot water up to 45 degrees.
Typically, treatment begins with a serving of 50–100 ml three times a day 1–1.5 hours before meals. During the first week, the single dose is gradually increased to 250 ml. The course of therapy is 35–40 days. The break between treatment with mineral waters should be long, at least 4 months. In case of impaired motility of the gallbladder and stagnation of bile, drinking tubes quickly help. The patient drinks a glass of warm mineral water in the morning on an empty stomach, then performs a set of physical therapy exercises. After this, he drinks another 200 ml of water and lies down with a heating pad on his right side. When the procedure is carried out correctly, pain, nausea, and bitterness in the mouth quickly decrease. At home, tubing is carried out 1–3 times a month, under the supervision of doctors – 1–2 times a week. This treatment is contraindicated in case of cholelithiasis. In the calculous form of cholecystitis, tubages and mineral waters that have a pronounced choleretic effect or with a high level of mineralization are not recommended. After cholecystectomy, you can be treated in this way after 3-4 months at home, but under the supervision of a doctor.