A healthy stomach determines the overall positive condition of the body. Here food processing processes take place for its further absorption by other organs. Disruption of the stomach leads to both external and internal negative changes.
Gastroduodenitis is a gastrointestinal disease characterized by inflammation of the lower part of the stomach and upper duodenum. Under the influence of negative factors, the functioning of the secretion regulation system is disrupted, which leads to excessive activity of gastric juice and bile entering the stomach cavity. Under the influence of these aggressive chemicals, irritation and inflammation of the mucous membrane occurs.
In the advanced phase, neighboring organs are affected: the pancreas and bile ducts. Without proper treatment, a stomach ulcer or malignancy may develop. In the system of therapeutic measures for gastroduodenitis, diet occupies a special place. Systematic proper and balanced nutrition helps to cope with the unpleasant symptoms of the disease and completely eliminates its cause - inflammation.
Causes of gastroduodenitis
Improper nutrition can cause gastroduodenitis.
The disease can occur under the influence of both external and internal factors. External factors:
- Incorrect diet, violation of diet.
- Side effects of medications.
- Stress
- Drinking alcohol and cigarettes.
Internal factors:
- The bacterium Helicobacter pylori.
- Caries.
- Tonsillitis.
- Diseases of the endocrine system.
- Biliary tract diseases.
- Congenital pathology of the gastric mucosa.
Causes of childhood gastroduodenitis:
- Infection with salmonellosis, E. coli, campylobacter through unwashed and insufficiently processed foods: eggs, meat, seafood, vegetables.
- Rotovirus infection.
- Intestinal Giardia.
- Lactose deficiency.
- Consumption of allergenic foods.
- Drug treatment.
- Poor nutrition: consumption of sausages, chips, carbonated drinks, etc.
Therapeutic course
Treatment of duodenitis is carried out under the supervision of a gastroenterologist. The patient is prescribed a strict diet: foods that are difficult to digest (milk, cereals) and dishes with spices are excluded from the diet. Drug therapy is based on drugs that suppress excessive secretion of hydrochloric acid in the stomach. Normalization of digestion is carried out by taking enzyme agents by a child or adult. Protecting the walls of the duodenum from irritation requires the use of gastroprotectors - drugs that coat the mucous membranes of the gastrointestinal tract.
In case of a complicated course of the disease, the gastroenterologist may insist on surgical intervention. Surgeons will eliminate intestinal obstruction and remove adhesions formed due to secondary duodenitis. In such cases, treatment requires hospitalization of the patient.
Types and symptoms of the disease
Gastroduodenitis causes acute pain.
There are:
- Chronic gastroduodenitis with increased acidity. Children and patients under 30 years of age are at risk.
- Chronic gastroduodenitis with low acidity. Middle-aged and elderly patients are at risk.
- Superficial gastroduodenitis with initial signs of the disease.
- Erosive gastroduodenitis with more serious damage to the mucosa (presence of erosion).
Symptoms: acute pain in the abdominal area (on an empty stomach or within 2 hours after eating), bowel dysfunction (diarrhea, constipation), heartburn, bloating, belching, nausea; fatigue, loss of appetite, dizziness.
The need to follow a diet
Compliance with therapeutic nutrition for duodenitis can relieve unpleasant symptoms during an acute process or exacerbation (pain, nausea, vomiting). In addition, proper nutrition during the period of remission allows you to delay the exacerbation of the disease.
A diet for duodenitis refers to proper and healthy food, normalizes the functioning of the entire digestive tract, prevents complications, and also disciplines the patient. In addition, the principles of a healthy diet have a beneficial effect on the patient’s well-being and appearance.
Dietary nutrition for gastroduodenitis
Diet is the best treatment for gastroduodenitis.
Food should be healthy and not burden the diseased organ with unnecessary work of digesting it. Basic rules for eating:
- 5-6 times a day in small portions.
- Dishes of liquid (semi-liquid) consistency.
- Minimize the temperature load on the stomach: no less than 15 and no more than 65 degrees.
- Products undergo mandatory heat treatment (especially for the erosive stage of the disease). Raw vegetables rich in fiber are acceptable for a preventive diet or for the superficial manifestation of the disease.
- Avoid fried foods.
- Maintain a drinking regimen: plenty of regular and mineral water.
- Taking folk remedies.
Diagnostic measures
Diagnosis of duodenitis is carried out during gastroscopy - immersion of an endoscopic probe into the patient’s stomach and intestines. Additional ways to confirm the diagnosis are:
- X-ray examination of the gastrointestinal tract;
- biochemical analysis of gastric juice;
- duodenal intubation;
- general clinical and biochemical blood tests;
- coprogram.
If signs of malignant degeneration of duodenal tissue are detected, the doctor takes a biopsy - biomaterial that is subjected to histological examination in the laboratory.
Diet products
Semolina porridge is the best product for dietary nutrition.
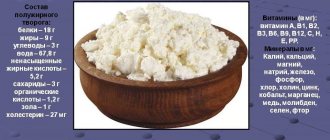
For high acidity: crackers, stale gray and white bread, dairy and fermented milk products (cheese, cottage cheese, kefir), pasta made from durum wheat.
Lean meat (rabbit, beef, turkey), cereals. Heat-treated vegetables and fruits, soft-boiled eggs, olive, sunflower, flaxseed, butter.
For low acidity (in addition to the above products): raw vegetables, meat, mushroom and fish broths, chocolate in small quantities.
The first place in the diet menu is occupied by porridges: semolina, oatmeal, rice. The natural mucus of this product envelops the walls of the stomach and protects the inflamed organ from the effects of hydrochloric acid.
On the second - cereal and vegetable soups, puree soups and broths, with finely chopped or grated ingredients. Lean meat, boiled sea fish, stewed vegetables. Drinks: jelly, mousse, kefir, milk, rosehip infusion.
The choice of one product or another for the diet menu depends on the type and stage of the disease. With superficial gastroduodenitis, restrictions apply to too hard and heavy foods, semi-finished products. The menu includes lean meats, seafood, fish, and dairy products rich in protein. Raw vegetables and fruits are allowed.
All ages are susceptible to duodenitis
Duodenitis often occurs in representatives of the stronger sex. Young women are often affected (in them it can be severe and be accompanied by various disorders in the central nervous system and the activity of the endocrine glands). It happens that the disease occurs in childhood, which is favored by inherited, in particular, weakness of the hormonal apparatus of the duodenum.
The causes of the disease are generally the same as for gastritis. Thus, inflammation can develop as a result of eating rough and poorly chewed food, alcohol, as well as smoking and prolonged neuropsychic stress. If a patient is diagnosed with parasitic diseases (infection with Giardia, roundworms, hookworms, etc.), then he is also in the “risk group” for duodenitis. The cause can be either exogenous (as a consequence of treatment with cytostatic drugs) or endogenous (for example, with gout, uremia).
Duodenitis “gets along” well with chronic gastritis, peptic ulcers, chronic pancreatitis, duodenal diverticulosis and some diseases of the liver and biliary tract. An increased content of hydrochloric acid and pepsin in gastric juice also contributes to the occurrence and development of the disease. It is also favored by impaired motor activity of the duodenum (characterized by long-term retention of contents in it). The disease can be triggered by activation of pathogenic microflora in the upper digestive tract. The development of the disease is facilitated by chronic infections in the mouth, pharynx, genitals and gall bladder, including kidney failure and tuberculosis.
Baby food for gastroduodenitis
To treat gastroduodenitis, you need to follow the milk consumption rate.
The diet for a sick child is formed depending on the age characteristics of the body.
Diet for babies
- Increase the frequency of feedings while maintaining milk consumption rates.
- For symptoms of dehydration (dry lips, rare urination, lack of tears), additional complementary foods and water are introduced (15-20% of the daily food intake).
- Water is given separately from the mixture (to preserve the nutritional value of the latter).
- If signs of the disease appear after the introduction of complementary foods, then the new product should be abandoned for a while.
- A nursing mother also needs to be more attentive to her diet: do not eat new foods or allergenic foods.
Diet for children from one year old
- Eliminate all types of sugary drinks, leave only water.
- Remove recently introduced or new products from the menu.
- Increase the number of meals to 6. At the same time, the load on the stomach is reduced due to the nutritional value of the products. Give more vegetables and fruits.
Products approved for use: bananas, lean meats, buckwheat, millet, semolina porridge, apple and pear puree; fresh vegetables, brown rice, water, mousses, milk jelly.
Prohibited foods: tea, full-fat milk and meat, fried and spicy, carbonated drinks and juices, gelatin, chips, ready-made crackers, sausages. Sample children's menu for the day:
- Breakfast: buckwheat (millet) porridge with butter, cookies or dried bread, children's drinking water.
- Second breakfast: fruit (green apple, pear or banana).
- Lunch: cream soup, meat dish (turkey, beef, chicken), side dish - coarse wheat pasta with tomato sauce.
- Afternoon snack: fruit puree or salad.
- Dinner: meat dish, broccoli puree, fresh vegetable salad. Before bed: kefir (milk jelly)
What should be the diet for gastroduodenitis, you will learn from the video:
https://www.youtube.com/watch?v=o1V2ST8LHeo
How should a patient eat without an exacerbation?
After the elimination of acute symptoms, the further course of gastroduodenitis largely depends on the patient’s endurance. The patient will have to get used to:
- avoid foods that irritate the mucous membranes;
- drink more fluids;
- to the exclusion of pickles, marinades, canned hot sauces and spices;
- to the lack of onions and garlic, pearl barley and millet porridge, fresh fruits and vegetables, strong coffee and tea.
Vegetables are necessary, but in boiled or stewed form, fruits in compote or jelly.
Prevention of gastroduodenitis
Having achieved relief, it is important to prevent the disease from returning. To do this you need to follow simple rules:
- Lead a healthy and active lifestyle.
- Continue to follow basic diet recommendations.
- Do not self-medicate.
Gastroduodenitis must be treated to prevent serious complications. Proper and healthy nutrition is an effective means for treating and preventing disease in children and adults.
Comments from nutritionists
For symptoms of gastroduodenitis, treatment with diet is a necessary condition for recovery. During this period, avoid taking non-steroidal anti-inflammatory drugs ( diclofenac , indomethacin , and buprofen , and spirin etc.), which are often prescribed for joint diseases. If there is a need to take them, then it is recommended to take them only after meals.
During an exacerbation, it is mandatory to take aloe and B of nicotinic acid for elderly patients .
Exacerbations of gastroduodenitis in children are often provoked by psycho-emotional factors, therefore, the comprehensive treatment of a child must necessarily include psychotherapy to eliminate stress and nervous overload.