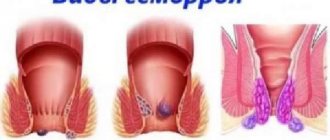
Hemorrhoids are one of the most common diseases and are diagnosed in every fifth person over 35 years of age. Despite the “popularity” of the disease, many men and women are afraid to seek help from a proctologist because of a feeling of shame. This decision has a negative impact on a person’s life, since hemorrhoids can provoke the development of not only painful sensations, but also serious diseases. From our article you will learn how forms of hemorrhoids exist, how to distinguish them from each other, how each of them is diagnosed and treated.
Haemorrhoids
Causes of the disease
Experts say that the patient has external and external hemorrhoids due to a genetic tendency to weakness of the venous walls. The following factors can increase the likelihood of developing hemorrhoids:
- Insufficient physical activity
- Systematic constipation, causing increased intra-abdominal pressure,
- Lack of water and foods enriched with plant fiber in the diet,
- Bearing a child and giving birth. During these processes, the pressure of the uterus on the intestines and adjacent organs increases. In parallel with this, an increase in blood flow is observed in the uterus, which can also provoke the development of internal hemorrhoids,
- Heavy physical activity.
Prolonged sitting often provokes the development of hemorrhoids
Excessive force loads are the cause of hemorrhoids in many people.
The above phenomena cause stagnation in the pelvis, a large blood volume puts strong pressure on the venous walls, causing its degenerative changes.
Be careful! According to statistics, internal hemorrhoids are more often diagnosed in women.
In women, hemorrhoids occur during pregnancy
types of meniscal tears
types of meniscal tears
Based on their location, the rupture of the posterior (develops most often), anterior horn and body is distinguished. Based on the main development mechanism and causative factor, the classification includes pathological processes and traumatic injuries.
Symptoms
If a patient has developed hemorrhoids, he can independently determine its type, since each form of hemorrhoids has separate symptoms.
Symptoms of external hemorrhoids
The initial stages of the disease may be accompanied by painful sensations even before the development of external bumps. The patient may suffer from:
- Continuous discomfort, burning and itching in the anus. If you scratch an itchy area, the epithelium becomes very irritated,
- Blood marks on paper used after defecation. This symptom is a sign of advanced disease, since external hemorrhoids have already increased in size and are injured by dense feces. Also, bleeding may appear due to anal fissures.
- Severe and sharp pain after defecation. It occurs due to exacerbation of the disease,
- Hemorrhoids are located on the outside of the anus. They resemble elastic balls that the patient can touch.
Read also: Is it possible to run with acute or chronic hemorrhoids, pros and cons, running rules and prohibitions
In most cases, NG is almost always in remission and worries the patient only during an exacerbation.
Symptoms of internal hemorrhoids
The symptoms of CH and the strength of their manifestation in the patient depend on the stage of the disease: the more advanced it is, the stronger its symptoms appear. The very first symptoms of the internal form of the disease include:
- Feeling of a foreign object in the PC,
- Feeling of incomplete bowel movement
- Development of pain in the anus, intensifying after emptying. When the disease enters the final stage, the pain manifests itself sharply and with greater intensity, greatly aggravating the patient’s condition. This happens due to the increase in hemorrhoids,
- The presence of bloody discharge after bowel movements. Initially, a small amount of blood is visible in the feces, but as the disease worsens, the bleeding intensity increases. In some patients it can be so severe that it can only be stopped by surgery.
- Itching and burning in the anus. These sensations negatively affect the patient’s emotional state and greatly deplete his nervous system.
While experiencing the above symptoms, the patient may not realize that he has developed CH. At the initial stage, the bumps appear only when the patient pushes, but over time they are noticeable even with normal intra-abdominal pressure.
Clinic
Symptoms of changes that develop as a result of trauma appear acutely, their intensity is proportional to the degree of impairment. Among them:
- Pain that develops mainly on the inside of the knee and intensifies when trying to carry out active or passive movements in it.
- Restriction of mobility, which can reach a complete block when part of the cartilage is torn off and wedged. Any attempts at movement usually lead to a sharp increase in discomfort.
- Inflammatory manifestations in the form of redness, swelling of soft tissues. They lead to a visually noticeable increase in the knee. There is a local increase in temperature (the knee joint becomes hot to the touch).
In pathological disorders leading to degeneration of internal cartilage, symptoms develop gradually over a fairly long period of time. The pain may be absent at first, then it appears and intensifies with loads on the leg. Movements may be accompanied by characteristic “clicks” and “crunches,” which indicates the development of degenerative processes in cartilage tissue.
Diagnosis of the disease
Diagnosis and treatment of hemorrhoids is carried out by a proctologist.
Diagnosis of NG
In 98 percent of cases, a routine examination of the patient is sufficient to diagnose external hemorrhoids.
Diagnosis of CH
Compared to diagnosing external hemorrhoids, determining the internal form is somewhat difficult, since in the first stages the lumps practically do not appear. In this case, the proctologist applies:
- Rectal examination of the patient. This diagnostic method is used without fail. The doctor palpates hemorrhoidal formations protruding into the lumen of the PC, checking their consistency. Unfortunately, the specialist cannot examine deep-lying cones, so he resorts to using other methods,
- Anoscopy. This method involves the use of specialized endoscopic equipment to diagnose the patient. The anoscope is inserted into the PC, illuminates it and allows the proctologist to examine the mucous membrane. Although anoscopy allows you to recognize many proctological diseases, it has one significant drawback - it allows you to examine the patient’s PC a maximum of ten centimeters from the anus,
- Sigmoidoscopy. This procedure is carried out if there is a need to examine about 25 centimeters of the patient’s PC. Sigmoidoscopy allows you to recognize and study even deeply located hemorrhoidal formations. Also, the use of this method allows the specialist to take material for a biopsy to exclude the development of cancer in the patient.
- Irrigoscopy. This study of the patient involves the introduction of barium sulfate into the intestines and X-raying it. Thus, the doctor will be able to see not only VH, but also anal fistulas.
Note! The above methods require special preparation from the patient. You can find out all the necessary information on this matter from your attending physician.
Forms of endometriosis
Experts distinguish genital (located within the organs of the reproductive system) and extragenital (outside the genital organs) endometriosis. The genital form, in turn, is divided into external, with damage to the peritoneum and ovaries, and internal - endometriosis of the uterine body (adenomyosis). With adenomyosis, pathological foci appear in the muscular layer of the uterus, which due to this gradually acquires a spherical shape and can significantly increase in size.
Treatment method for VH
Therapy for internal hemorrhoids can be surgical or conservative.
Read also: How internal hemorrhoids are treated: groups of drugs, minimally invasive techniques
Conservative treatment is effective for the patient only in the early stages of the disease. It assumes:
- Carrying out symptomatic therapy (pain relief, stabilization of intestinal function),
- Preventing the development of blood clots,
- Use of venotonics.
If a patient has hemorrhoids diagnosed at the first or second stage of its development, the proctologist can use infrared photo- and electrocoagulation, as well as sclerotherapy of hemorrhoidal cones. Dilated venous areas stick together, become empty and dissolve over time.
At the third stage of hemorrhoids, it is advisable for the patient to carry out more radical surgical measures:
- Cryodestruction (freezing hemorrhoids with liquid nitrogen),
- Ligation with latex rings,
- Surgical ligation of dilated vessels,
- Hemorrhoidectomy using the Milligan-Morgan or Longo method,
- Desarterization (ligation of hemorrhoidal arteries). The procedure is controlled by Doppler ultrasound.
Ligation with latex rings
If a patient has been diagnosed with thrombosis of internal hemorrhoids, he is prescribed anticoagulant therapy. Surgical measures involve cutting, removal of thrombotic mass and evacuation of thrombosed cones.
Reduction of a prolapsed VG can be done manually. If this does not give a positive result, surgical intervention is possible, but only after the exacerbation has resolved.
Traditional medicine recipes
Traditional medicine is often combined with folk medicine to treat CH. As practice shows, a competent combination of these techniques shows very good results. In most cases, alternative medicine is used to relieve itching, burning, pain and inflammation in the anus. Good for this:
- Bone decoction. 35 grams of berries are poured with water and boiled for 20 minutes over medium heat. The decoction should infuse for 10 hours, then take a tablespoon every 3.5 hours, but no more than five times a day. The healing drink eliminates pain, strengthens vascular walls and has an anti-inflammatory effect,
- Bath or microenema with chamomile, oak bark, sage and calendula,
- Homemade rectal suppositories with potato juice, birch tar and aloe juice.
Endometriosis and drug therapy
Taking medications for endometriosis can help suppress the growth of endometrioid tissue and alleviate existing symptoms of the disease. The main emphasis is on hormonal therapy. Use:
- estrogen-progestin agents;
- antigonadotropic drugs;
- gestagens;
- gonadotropin releasing hormone agonists.
Hormonal treatment with small doses of gestagens is effective in the early stages of the development of pathology. The main goal of these drugs is to suppress the production of estrogen, which will inevitably lead to the death of endometrioid cells. There are hormones that are used throughout the entire period of treatment, in long courses, they suppress ovulation and endometrial growth.
Gonadotropin releasing hormone agonists can be used only 1-2 times a month, which is attractive for women. They block the functioning of the ovaries, which makes it possible to relieve pelvic pain and relieve patients from discomfort and anemia. The restoration of menstruation occurs 1-6 months after the end of drug therapy.
Gonadotropin-releasing hormone agonists are available in different forms. When they are used, the production of estrogens (specific female sex hormones) stops. By doing this, specialists achieve a decrease in the activity of endometriotic tissue, which ultimately leads to atrophic phenomena and obtaining favorable treatment results. But women should remember that hormones are prescribed only by specialists, under the control of the functioning of internal organs and general health.
Improvement in the well-being of patients is not observed immediately. The first signs of the effectiveness of therapy appear after 2-3 weeks of taking the drugs. It is impossible to completely stop the synthesis of sex hormones in a short time, even with potent hormonal treatment.
Antigonadotropic medications help relieve pain and prevent relapses of endometriosis and infertility. But antigonadotropins can cause a number of undesirable consequences, causing the appearance of excess weight, acne, swelling, physical looseness and general weakness. Therefore, it must be used strictly according to indications and no longer than the period prescribed by the doctor.
Treatment methods for NG
External hemorrhoids can be treated in two ways:
- Conservative methods
- Surgical intervention.
Conservative therapy involves taking special measures that will help eliminate the symptoms of the disease and improve the patient’s condition. These include: taking medications, observing dietary restrictions and general lifestyle adjustments.
To treat NG, you can use tablets, ointment, gel, cream and rectal suppositories. The main task of these pharmaceuticals is to relieve swelling, itching and inflammation. The constituent component of many of them is an anesthetic that relieves pain. Medicines whose components thin the blood show a good therapeutic effect. Thanks to this, the patient’s blood clots dissolve and the risk of new ones forming is significantly reduced.
For the treatment of external hemorrhoids, it is advisable to prescribe topical medications. Compared to rectal suppositories, they are easier to use and have better results. The most effective medications include:
- "Relief"
- "Proctosedyl"
- "Posterizan"
- "Aurobin"
- "Hepatrombin"
- "Heparin ointment."
The following tablets show good results for the treatment of external hemorrhoids:
- "Detralex"
- "Ginkor Fort"
- "Aklezan A"
- "Pylex."
Read also: Causes of itching in the anus in women, traditional treatment methods and folk remedies
Detralex
Be carefull! Non-steroidal pharmaceuticals with an anti-inflammatory effect are sometimes used to treat NG: indomethacin, diclofenac and ibuprofen. They quickly relieve pain and inflammation, but should only be used as directed by a qualified professional.
The use of minimally invasive therapeutic techniques can be prescribed by a doctor if there are no positive results from conservative treatment. In such cases, it is advisable to:
- Infrared photocoagulation (in the first stages of disease development),
- Ligation of external hemorrhoids with latex rings (at the third and fourth stages).
It is prohibited to perform minimally invasive therapy on patients who suffer from:
- Acute or purulent paraproctitis,
- Thrombosis of hemorrhoidal formations,
- Cracks in PC.
Surgical intervention in the treatment of NG is performed for patients in whom the disease is constantly exacerbating and progressing, and conservative methods do not produce any results.
If the patient’s disease is complicated by the presence of blood clots in the cones, a thrombectomy is performed: the nodes are opened and the blood clots are removed from them. Thrombosis is considered a very serious disease. If left untreated, the patient may develop necrotic tissue damage followed by blood poisoning. If a person does not seek qualified help in time, he may die.
People's Councils
Alternative medicine is good for treating all forms of hemorrhoids. If the patient suffers from external bumps, he can use a sitz bath or steam bath based on herbal infusions. A decoction of string, chamomile and calendula removes inflammation. At home, the patient can prepare an ointment from propolis, honey or mummy. Onion juice, birch tar and celandine juice have a healing effect on NG. Also, to relieve inflammation, the patient can apply raw potatoes, carrots and clay to the external nodes.
A popular treatment for NG patients is sea buckthorn oil. A small amount of the substance is applied to a cotton swab and applied to the problem area.
Sea buckthorn oil
The medicinal herb Knotweed has received good reviews among patients, as it has a strong anti-inflammatory effect. It can be used as an oral decoction or as a poultice for sore bumps. Preparation of the healing drink is very simple: pour 2.5 tablespoons of the substance with boiling water (250 ml) and leave to infuse in a warm place overnight. In the morning the drug is ready for use. For oral administration, it is enough to drink 50 milliliters three times a day.
Highlander
It would not be superfluous for the patient to use cold baths. To make them, the patient needs to pour cold water into a shallow basin, add infusions of chamomile, rose hips and sage and sit in the water for 5-7 minutes. It is better to carry out the procedure 2-3 times a day until the symptoms of the disease disappear.
Rehabilitation
Rehabilitation
Carrying out rehabilitation measures is no less important than the main course of treatment. It involves resting the knee immediately after surgery or conservative therapy, followed by special activities that involve certain movements.
As the tissues recover, the range of motion and load gradually increase. This makes it possible for the cartilage tissue to adapt to loads and subsequently restore the functional state of the knee.