Crohn's disease is a chronic inflammatory disease of the digestive tract. The manifestations of the pathology are varied, often including dyspeptic disorders, stool disorders, abdominal pain, as well as symptoms of intoxication and exhaustion. Treatment includes taking medications to relieve and prevent exacerbations, and, if necessary, surgical intervention.
In adults, the peak incidence of Crohn's disease occurs around age 30. Among women and men, granulomatous inflammation of the intestine occurs with equal frequency. In children, Crohn's disease manifests itself mainly after 10 years.
Causes
The etiology of the disease is currently unknown to science.
Scientists are discussing a hypothesis about its relationship with the impact of the measles virus during pregnancy on the fetus or newborn child. Factors that can trigger the development of Crohn's disease include:
- smoking;
- jar of Hearts;
- hypovitaminosis D;
- a diet enriched in animal protein and poor in dietary fiber;
- intestinal infection;
- appendectomy.
There is a hereditary predisposition to intestinal damage in Crohn's disease in close relatives. It has also been revealed that it develops more often in people living in metropolitan areas and representatives of the Caucasian race.
Etiology
Crohn's disease is a polyetiological disease. Factors that increase the risk of developing this pathology include:
- genetic predisposition: the majority of newly identified patients have a burdened hereditary history along a similar line;
- immune imbalance;
- eating increased amounts of refined foods, as well as simple carbohydrates;
- the presence of other autoimmune problems: rheumatoid arthritis, including juvenile arthritis, systemic lupus erythematosus, etc.;
- smoking.
There is also a theory of the influence of lifestyle on the incidence of CD, according to which in developed countries people are susceptible to pathology more often than in poor countries.
Symptoms
Manifestations of the disease depend on the location of the inflammation.
Extraintestinal symptoms of Crohn's disease include weight loss, episodes of fever up to 38-39 degrees, anemia, joint damage in the form of arthritis, arthralgia and arthropathy, erythematous and pyodermal rashes on the skin, episcleritis, uveitis, stone formation in the biliary organs and urinary system . Signs of granulomatous intestinal inflammation are:
- diarrhea in the form of unformed stools with mucus more than 5 times a day;
- the presence of blood and pus in the stool;
- constant, cramping pain in a certain area of the abdomen;
- with inflammation in the anorectal area - the appearance of pain during bowel movements.
In case of development of ileitis or ileocolitis, the formation of internal and external fistulas is possible.
Intestinal obstruction is accompanied by spontaneous periodic abdominal pain, stool retention and the passage of gas. Often the first manifestations of Crohn's disease are inflammation in the oral cavity - aphthous stomatitis, as well as an increase in the size of the lips, a change in the relief of the mucous membrane like a “cobblestone street”.
Involvement of the esophagus, stomach and duodenum is less common than the ileum, colon or rectum. In this case, bleeding from the upper digestive tract and difficulty swallowing while eating may occur.
Preparing for a visit and a doctor's visit
A gastroenterologist diagnoses and treats gastrointestinal diseases. Before visiting a specialist, prepare for the fact that you may be asked the following questions:
- the onset of symptoms when ailments manifest themselves for the first time;
- symptoms are present all the time or unpleasant phenomena occur periodically;
- Do the symptoms intensify due to some events, provoking factors (after stressful situations, taking certain medications, certain foods, etc.);
- your general condition - how uncomfortable the manifestations of the disease are, how much your well-being has worsened and how this is manifested, whether your quality of life has decreased, whether there are any restrictions on any type of activity or taking certain foods;
- whether you took medications after the first signs of the disease appeared and whether you are currently taking certain medications (list).
Based on the information received and a comprehensive clinical examination (palpation of the abdomen, examination of the oral cavity), the specialist draws up a subsequent examination regimen.
Complications
Due to deep damage to the intestinal wall, complications develop in Crohn's disease, which often significantly aggravate the course of the underlying disease.
These include:
- bleeding from the upper and lower digestive tract;
- perforation of hollow organs with the development of peritonitis;
- internal fistulas with the formation of communication between the inflamed intestine and neighboring organs;
- external fistulas with an outlet on the surface of the abdominal wall;
- anal fissures, paraproctitis, rectal strictures;
- fibrous changes in the wall of the affected organ, stenosis and development of intestinal obstruction;
- interintestinal and interorgan purulent infiltrates and abscesses;
- toxic megalocolon - excessive expansion of the lumen of the colon with absorption of its contents into the blood;
- development of dysplasia and malignant degeneration of affected tissues.
What is Crohn's disease?
Crohn's disease
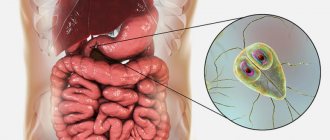
is a chronic inflammatory disease that can cover the entire gastrointestinal tract (GIT): from the oral cavity to the anal area. With this pathology, the resulting inflammation affects the entire thickness of the wall of the affected area of the gastrointestinal tract, which leads to the development of deep ulcers. The cause of this inflammation is a pathological reaction of the immune system: our own “defender” cells attack the cells of the gastrointestinal tract. In approximately 80% of cases, the disease affects the final section of the small intestine - the ileum; damage to both the small and large intestines is slightly less common.
The clinical picture of the disease is often multifaceted and ambiguous, so in some cases years pass before a correct diagnosis is made.
The incidence and prevalence of the pathology is growing all over the world: most often the onset of the disease occurs in people aged 15 to 30 years, the second peak incidence occurs at the age of 50-80 years, however, it is worth noting that this inflammatory bowel pathology can manifest itself at any age. age; with Crohn's disease, there is also a tendency towards a slight predominance of women compared to men among the number of cases.
Crohn's disease cannot be cured, however, with the help of modern drug therapy and surgical treatment, it is possible to achieve stable remission of the disease - a significant reduction in symptoms, taking the disease “under control”.
Diagnostics
With symptoms of the disease, patients more often turn to a general practitioner or therapist, who in turn refers such patients for further examination and treatment to a gastroenterologist, surgeon, or proctologist.
Diagnosis of Crohn's disease includes taking an anamnesis, examination, and the use of laboratory and instrumental research methods.
In a general blood test for granulomatous inflammation of the intestine, the following changes are possible:
- acceleration of ESR;
- an increase in the number of leukocytes with a shift in the leukocyte formula to the left;
- decrease in hematocrit and hemoglobin levels;
- moderate thrombocytosis.
The biochemical blood test also shows markers of inflammation and electrolyte disturbances.
Extraintestinal changes accompanied by damage to the liver and pancreas may be manifested by increased levels of transaminases, GGTP, alkaline phosphatase, amylase and lipase. If differential diagnosis of anemia is necessary, it is advisable to examine the level of folic acid, vitamin B12, serum iron, total iron-binding capacity of serum, and ferritin. In case of severe diarrhea, stool analysis and bacteriological examination are performed to exclude acute intestinal infection. The biomaterial is also analyzed for worm eggs and parasites to exclude helminthiasis, and fecal calprotectin and lactoferrin are detected to determine the degree of inflammation.
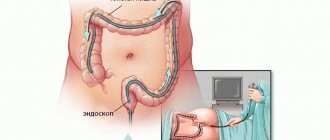
Instrumental research methods primarily include ultrasound of the abdominal organs, retroperitoneum, pelvis and esophagogastroduodenoscopy. If the diagnosis is not established, colonoscopy with ileoscopy and plain radiography of the abdominal cavity are performed. If necessary, MRI, CT with contrast, fistulography in the presence of external fistulas, and biopsy of the intestinal mucosa in the affected area are performed. For perianal lesions, transrectal ultrasound or MR examination of the rectum and anal canal is performed.
Differential diagnosis of Crohn's disease is carried out with nonspecific ulcerative colitis and other pathologies, such as:
- irritable bowel syndrome;
- intestinal infection;
- vascular lesions of the intestine;
- endocrine diseases;
- radiation, chemical, drug enteritis and colitis.
Classification
The current classification of Crohn's disease has been developed based on the location of the lesion, the nature and severity of the course, the prevalence of the process, as well as the phenotypic form and dependence on the response to hormonal therapy.
Classification by location of the lesion (Montreal):
- terminal yelitis;
- colitis;
- ileocolitis.
The first two forms are characterized by damage to the upper gastrointestinal tract, the latter by the development of a pathological process in the anal area.
According to the prevalence of the lesion:
- clearly localized CD: divided into isolated lesions of a small area of the intestine and lesions no more than 30 cm;
- widespread CD: characterized by a lesion area larger than 100 cm (the sum of all areas is taken into account in the calculation).
According to the nature of the flow:
- acute: the period from the onset of the disease does not exceed 6 months;
- chronic continuous: subject to adequate therapy, there are no six-month periods of remission;
- chronic relapsing course: a history of the disease includes six-month or longer periods of remission.
According to severity:
- light;
- medium-heavy;
- heavy.
Severity is assessed based on the degree of attack, that is, the current exacerbation or the Best activity index. The use of a particular rating system is determined on the basis of the practical methods of a particular medical institution.
Depending on the phenotypic form:
- non-stricturing, non-penetrating (similar names in Russian-language scientific manuals - luminal, uncomplicated, as well as infiltrative-inflammatory);
- stricturing form (stenotic);
- penetrating option (fistula).
Perianal lesions can either complement any of the listed phenotypic forms or be an independent clinical manifestation of CD.
Depending on the response to hormonal therapy:
- Hormonal resistance. In the case of a severe form, the absence of positive dynamics after more than 7 days of active therapy is taken into account, and in the case of a moderate course, within two weeks.
- Hormonal dependence. The status is assigned when a relapse develops within 90 days after hormonal therapy, as well as when the activity of the pathology increases when the dose of drugs is reduced (after stable improvement) for 3 months after the course.
Example of DS formulation: Crohn's disease: ileocolitis, stenotic form (stricture without intestinal obstruction), chronic relapsing course, mild attack. Hormonal dependence.
specialist
Our doctors will answer any questions you may have
Tumasova Anna Valerievna Gastroenterologist
Treatment
Treatment of Crohn's disease is aimed at stopping and preventing exacerbations of the disease, eliminating complications. The goal of drug therapy is to put the disease into long-term remission, since it is currently impossible to completely cure it. For this purpose, drugs of the following groups are used:
- aminosalicylates;
- glucocorticosteroids;
- immunosuppressants;
- biological drugs;
- antibacterial agents;
- ursodeoxycholic acid.
Painkillers and antidiarrheals are used to relieve symptoms.
Additionally, iron supplements, agents to control anemia, prevent osteoporosis, and vitamin supplements are prescribed. The diet for Crohn's disease involves avoiding foods that stimulate peristalsis, fermentation and putrefaction in the intestines, in particular those rich in fiber. It is also important to exclude additional sensitization by food allergens, therefore extractive substances, chocolate, cocoa, eggs, coffee, citrus fruits, red apples, strawberries, wild strawberries, baked goods, and industrial canned food are prohibited. Dishes should be mechanically and chemically gentle with a high content of vitamins and protein. With a high degree of inflammation activity, parenteral nutrition is prescribed.
If conservative therapy is ineffective, as evidenced by the presence of hormonal dependence and resistance, delayed physical development, as well as the appearance of complications, surgery is performed. The latter may include:
- resection of a section of the intestine changed due to inflammation, followed by anastomosis;
- formation of ileostomy;
- stricturoplasty;
- drainage of abscesses.
General recommendations for Crohn's disease include quitting smoking, and during an exacerbation, complete physical and mental rest.