Crohn's disease is a chronic inflammatory disease of the digestive tract, characterized by multiple formation of ulcers on the intestinal mucosa, the proliferation of specific granulomas and narrowing of the intestinal lumen. The inflammatory process can spread to the entire gastrointestinal tract from the root of the tongue to the anus or cover individual areas. The small intestine is most often affected. This is a very serious and unpleasant disease that is difficult to treat. It is found in children of all ages.
Symptoms and clinical picture
The disease develops gradually, sometimes over many years. The reason to suspect its presence is a child’s delay in growth and development.
The clinical picture is very diverse; in many ways this disease is similar to others, which makes its diagnosis much more difficult.
Characteristic manifestations of Crohn's disease are frequent diarrhea (large stools up to 10 times a day) and cramping abdominal pain. The fecal matter is whitish, often with bloody streaks. If the stomach is affected, it is manifested by a feeling of heaviness, nausea, and vomiting. Later, bloating may occur. Anal fissures and fistulas may appear.
When the small intestine is damaged, the process of absorption of nutrients from food and their proper distribution in the body is disrupted, which leads to anemia, delayed physical development, and menstrual irregularities in girls.
Extraintestinal manifestations - joint pain, stomatitis, conjunctivitis.
Common symptoms of Crohn's disease:
- fever;
- weakness;
- fast fatiguability;
- lack of appetite;
- weight loss;
- low-grade fever.
Crohn's disease in children. Symptoms. Diagnostics. Treatment.
Crohn's disease is a chronic nonspecific progressive transmural granulomatous inflammation of the gastrointestinal tract.
The terminal part of the small intestine is most often affected, so there are such synonyms for this disease as “terminal ileitis”, “granulomatous ileitis”, etc. Any part of the digestive tract from the root of the tongue to the anus can be involved in the pathological process. The frequency of damage to intestinal sections decreases in the following sequence: terminal ileitis, colitis, ileocolitis, anorectal form, etc. Focal, multifocal and diffuse forms are also distinguished. The course of Crohn's disease is undulating, with exacerbations and remissions.
Crohn's disease is detected in children of all age groups. The peak incidence occurs between 13 and 20 years of age. Among the sick, the ratio of boys to girls is 1:1.1.
Etiology and pathogenesis
The etiology and pathogenesis of the disease are unknown. The role of infection (mycobacteria, viruses), toxins, food, and some medications, considered as a trigger for the development of acute inflammation, is discussed. Immunological, dysbiotic, and genetic factors are of great importance. A connection has been established between the HLA histocompatibility system and Crohn's disease, in which the DR1 and DRw5 loci are often identified.
Clinical picture
The clinical picture of the disease is very diverse. The onset of the disease is usually gradual, with a long-term course with periodic exacerbations. Acute forms are also possible.
- The main clinical symptom in children is persistent diarrhea (up to 10 times a day). The volume and frequency of stool depend on the level of damage to the small intestine - the higher it is, the more frequent the stool and, accordingly, the more severe the disease. Damage to the small intestine is accompanied by malabsorption syndrome. An admixture of blood periodically appears in the stool.
- Abdominal pain is a common symptom in all children. The intensity of pain varies from minor (at the beginning of the disease) to intense cramping associated with eating and defecation. When the stomach is affected, they are accompanied by a feeling of heaviness in the epigastric region, nausea, and vomiting. In the later stages, the pain is very intense and is accompanied by bloating.
- General symptoms of the disease: general weakness, weight loss, fever. With significant damage to the small intestine, the absorption and metabolism of proteins, carbohydrates, fats, vitamin B12, folic acid, electrolytes, iron, magnesium, zinc, etc. are impaired. Hypoproteinemia is clinically manifested by edema. Characterized by delayed growth and sexual development.
- The most common extraintestinal manifestations of Crohn's disease are arthralgia, monoarthritis, sacroiliitis, erythema nodosum, aphthous stomatitis, iridocyclitis, uveitis, episcleritis, pericholangitis, cholestasis, and vascular disorders.
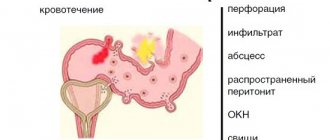
Complications
in Crohn's disease are most often associated with the formation of fistulas and abscesses of various locations, intestinal perforation, and peritonitis. Intestinal obstruction and acute toxic dilatation of the colon are possible.
Laboratory and instrumental studies
A general blood test reveals anemia (decreased red blood cells, hemoglobin, hematocrit), reticulocytosis, leukocytosis, and increased ESR. A biochemical blood test reveals hypoproteinemia, hypoalbuminemia, hypokalemia, a decrease in the content of microelements, an increase in the level of alkaline phosphatase, a2-globulin and C-reactive protein. The severity of biochemical changes correlates with the severity of the disease.
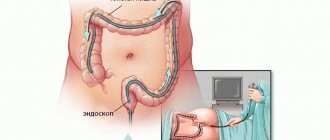
The endoscopic picture of Crohn's disease is characterized by great polymorphism and depends on the stage and extent of the inflammatory process. Endoscopically, three phases of the disease are distinguished: infiltration, ulcers-fissures, scarring.
- In the infiltration phase (the process is localized in the submucosa), the mucous membrane has the appearance of a “quilt” with a matte surface, the vascular pattern is not visible. Subsequently, aphthae-type erosions appear with isolated superficial ulcerations and fibrinous deposits.
- In the phase of fissure ulcers, individual or multiple deep longitudinal ulcerative defects are detected, affecting the muscular layer of the intestinal wall. The intersection of cracks gives the mucous membrane a “cobblestone” appearance. Due to significant swelling under the mucous membrane, as well as damage to the deep layers of the intestinal wall, the intestinal lumen narrows.
- During the scarring phase, areas of irreversible intestinal stenosis are detected. Characteristic radiological signs (the study is usually carried out with double contrast) are segmented lesions, wavy and uneven contours of the intestine. In the large intestine, irregularities and ulcerations are determined along the upper edge of the segment with preservation of haustration along the lower edge. At the stage of ulcers-cracks - the appearance of a “cobblestone pavement”.
Diagnosis and differential diagnosis
The diagnosis is established on the basis of clinical and anamnestic data and the results of laboratory, instrumental, and morphological studies.
Differential diagnosis of Crohn's disease is carried out with acute and protracted intestinal infections of bacterial and viral etiology, diseases caused by protozoa, worms, malabsorption syndrome, tumors, ulcerative colitis, etc.
Differential diagnosis of inflammatory bowel diseases
| Clinical symptom | Disease | |
| Nonspecific ulcerative colitis | Crohn's disease | |
| Stool with blood | Often | Rarely |
| Stomach ache | Rarely | Often |
| Tenesmus | Often | None |
| Stool volume | Moderate | Excess |
| Rectal lesion | Always expressed | Rarely |
| Perianal lesions | Rarely | Often |
| Fistulas | Rarely | Often |
| Relapses after surgery | No | Often |
Treatment
The regimen during the period of exacerbation is bed rest, then gentle. Medical nutrition (table No. 4 according to Pevzner). The nature of the diet largely depends on the location and extent of intestinal damage and the phase of the disease.
The most effective drugs are considered to be 5-aminosalicylic acid (mesalazine) and sulfasalazine. At the same time, it is necessary to take folic acid and multivitamins with microelements in an age-specific dose. In the acute phase of the disease and in case of severe complications (anemia, cachexia, joint damage, erythema, etc.), glucocorticoids (hydrocortisone, prednisolone, dexamethasone) are prescribed, and less often, immunosuppressants (azathioprine, cyclosporine).
In addition, broad-spectrum antibiotics, metronidazole, probiotics, enzymes (pancreatin), enterosorbents [diosmectite (smecta)], antidiarrheal drugs (for example, loperamide), and symptomatic agents are used to treat patients with Crohn's disease. In severe cases of the disease with the development of hypoproteinemia and electrolyte disturbances, intravenous infusions of solutions of amino acids, albumin, plasma, and electrolytes are performed. According to indications, surgical treatment is carried out - removal of the affected parts of the intestine, excision of fistulas, anastomosis to restore patency.
Prevention
Prevention involves rational, complete nutrition, appropriate for age and individual capabilities of the gastrointestinal tract, prevention and consistent treatment of acute intestinal infections, parasitic diseases, as well as other pathologies of all parts of the digestive system.
Forecast
The prognosis for recovery is unfavorable; for life, it depends on the severity of the disease, the nature of its course, and the presence of complications. It is possible to achieve long-term clinical remission.
Source: Children's diseases. Baranov A.A. // 2002.
Diagnostic methods
The process of diagnosing Crohn's disease begins with the study of complaints, history taking, examination and palpation. Soreness of the abdomen, its hardness, palpation on the lower right side of a space-occupying formation, swollen, usually painful polyps in the anal area gives the doctor reason to assume the presence of this disease.
To confirm the primary diagnosis, tests are taken for Crohn's disease - general and biochemical blood and urine tests, feces for occult blood. Based on their results, it is possible to establish the presence of inflammation, the degree of its activity, determine the causes of diarrhea, and differentiate Crohn's disease from nonspecific ulcerative colitis and cancer.
An X-ray examination of the stomach, intestines, and throat is also performed to determine the location of foci of inflammation, detect strictures of the small intestine and fistula tracts.
An important diagnostic test is colonoscopy. Visualizes the intestinal mucosa and reveals specific signs of the disease.
If there is a need to assess the condition of other organs, an ultrasound or computed tomography is prescribed.
Why does Crohn's disease occur?
The exact cause of Crohn's disease is unknown. It was previously believed that a certain diet and high levels of stress were the causes of the disease. But it is now known that these factors may aggravate, but not cause, the disease. Smoking, other gastrointestinal diseases and an imbalance of the intestinal microbiota can also aggravate the disease.
How does microbiota fight stress and depression?
Doctors identify two main risk factors for developing Crohn's disease: hereditary predisposition and a malfunction of the immune system.
- The immune system. Sometimes, when the immune system fights foreign microorganisms, an abnormal immune response can occur. In this case, the immune system can also attack the cells of the gastrointestinal tract.
- Hereditary predisposition . Crohn's disease is more common in people who have family members who also have the disease. However, most people with Crohn's disease do not have a family history of it.
Scientists also suggest that Crohn's disease may be caused by a virus or bacteria, but there is no evidence for this theory yet.
Who is at risk?
- Young people. Although Crohn's disease can begin at any age, most patients are diagnosed before age 30.
- People of Eastern European (Ashkenazi) Jewish descent. The incidence is also increasing among black people living in North America and the UK. It is important to consider that Crohn's disease can affect any ethnic group.
- People with a family history of Crohn's disease. If your parents or siblings (first-degree relatives) have the disease, your risk increases. One in five people with Crohn's disease has a family member with the disease.
- People who smoke. Cigarette smoking leads to more severe disease and a greater risk of surgery.
- People taking non-steroidal anti-inflammatory drugs. Although the drugs themselves do not cause Crohn's disease, they can lead to inflammation in the intestines, which makes the disease worse.
How to assess risks
The development of the disease involves genes that regulate various processes in the intestine. They are involved in inflammatory reactions and autophagy, the process of cell self-destruction. Associated genes also influence the interaction between the body and gut bacteria. You can find out if you have such genes using a genetic test.
What can you learn from a genetic test?
To date, scientists have also been able to describe the microbiota profile observed in Crohn's disease. The less similar your microbiota profile is to that of your disease, the lower your risks. The indicator is assessed on a scale from 1 to 10. A microbiota test will help you find out how far your microbiota is from the profile for Crohn's disease and whether you need to adjust your diet to avoid it.
In Crohn's disease, the ratio of opportunistic bacteria that trigger inflammation and beneficial bacteria changes. Also, the presence of beneficial bacteria - producers of butyric acid, which protects the intestines from inflammation - is often sharply reduced.
Basic treatment methods
How Crohn's disease is treated depends on its stage and the lesions present.
The main methods of treatment are a special diet and drug therapy. A diet with plenty of easily digestible proteins and limited consumption of fatty foods and milk is required.
Among the medications, corticosteroids are usually used to relieve inflammation, broad-spectrum antibiotics, as well as auxiliary agents for the treatment of concomitant conditions (extraintestinal manifestations, fistulas, diarrhea, etc.).
Severe cases require surgery.
Definition
Crohn's disease is a chronic inflammatory disease primarily affecting the gastrointestinal (GI) tract.
Although any part of the gastrointestinal tract from the mouth to the anal canal (back passage) can be involved, the end part of the small intestine (ileum) and/or large intestine (colon and rectum) is most often affected. Crohn's disease is a chronic disease and can flare up many times throughout life. Some patients have long-term remissions, sometimes for several years, without any symptoms of the disease. It is impossible to predict when remission will begin or when symptoms of the disease will return.
Should we try to avoid surgical treatment of CD at all costs?
Although medical (conservative) treatment is preferred as an initial step, it is important to understand that about 3/4 of all patients ultimately require surgical treatment. Many patients mistakenly believe that surgery for Crohn's disease is dangerous or inevitably leads to complications.
Surgery is not a panacea, but after one operation, many patients will not require additional surgery. The most common treatment procedure is conservative therapy with limited bowel resection (removal of only the affected area of the bowel).
Surgery often provides long-lasting relief from Crohn's disease symptoms and reduces or eliminates the need for ongoing medication use. Surgical treatment is best performed by a coloproctologist surgeon working in a clinic that has experience in complex treatment of patients with Crohn's disease.