Burns, especially with extensive lesions, are often accompanied by the development of functional and organic changes in the internal organs of the victims. Severe burn disease, inadequate treatment and a number of other reasons can lead to complications, often fatal. Acute erosive and ulcerative lesions of the gastrointestinal tract (GIT) attract special attention.
Acute gastric ulcers were first described in a patient with burns in 1823 by J. Swan [1]. The causal relationship between burn injury and the development of acute gastric or duodenal ulcers was established in 1842 by Thomas Curling [2], which is why they are often called Curling’s ulcers. Chronic gastroduodenal ulcers, according to the literature, are found in burn victims only in 1.6-21.9% of cases; acute erosions and ulcers of the gastrointestinal tract are detected much more often [3-5].
Such lesions in severely burned patients occur much more often than it is possible to diagnose on the basis of the clinical picture alone, therefore, often the manifestation of both chronic and acute erosions or ulcers of the esophagus, stomach and duodenum in burned patients is gastrointestinal bleeding (GIB). Acute erosive and ulcerative lesions of the gastrointestinal tract, including those complicated by gastroduodenal bleeding, even if not the direct cause of death, significantly aggravate burn disease and worsen its prognosis [6-9].
In most cases, uncomplicated acute erosions and ulcers, without specific clinical manifestations, remained unrecognized and were discovered in the recent past only at autopsy [10]. According to M.I. Kuzina et al. [11], the incidence of ulcers reported by different clinicians based on autopsy data varied markedly, which was due in part to differences in terminology. A mucosal defect that did not penetrate muscle tissue was considered an erosion. However, the division of lesions of the wall of the stomach and duodenum into erosions and ulcers, in our opinion, can be considered artificial, since the process has a single pathogenetic basis.
The pathogenesis of burn disease combines complex metabolic processes, endotoxemia, microcirculation disorders and many other signs that predispose to the development of acute erosive and ulcerative lesions of the gastrointestinal tract [12].
The existing circulatory theory cannot fully reveal the cause of the formation of gastrointestinal ulcers in burn disease. The peptic theory does not fully explain the cause of ulcers. In this theory, a significant place is occupied by the assumption of the role of increased secretion and acidity in the occurrence of both acute gastric ulcers and erosions and ulcers of the esophagus due to reflux of gastric contents. The main pathogenetic mechanism of developing gastrointestinal tract infections is also a combination of increasing the influence of an aggressive factor (increased production of hydrochloric acid) and weakening the protective factors of the gastric mucosa (ischemia). However, not all authors found a high level of gastric acidity in burn injury. According to D.O. Wagner et al. (2016), the frequency of hyperacidity in patients in a state of burn shock was no more than 14%, 69% of victims were in a hypo- or anacid state, but in 25% of cases, erosions and ulcers of the gastrointestinal tract were detected in patients [13]. The role of endogenous intoxication in the genesis of morphological changes during the development of acute ulcerations of the gastrointestinal tract in severely burned patients is also confirmed [14]. Therefore, the pathogenesis of acute erosive and ulcerative lesions of the gastrointestinal tract requires further study.
More often, erosive and ulcerative changes in the gastrointestinal tract are detected in the early stages after injury, during the period of burn shock [3, 15, 16], but they can also develop during periods of acute burn or septicotoxemia against the background of a stressful toxic or bacterial load on the victim’s body.
Acute gastroduodenal ulcers in burned patients are often asymptomatic. Complications from the gastrointestinal tract may be masked by the clinical manifestations of burn disease or its complications such as sepsis. Diagnosis of these complications is difficult due to the blurred clinical picture against the background of burns. Diagnosis of ulcerative lesions in these patients is especially difficult due to the forced position in bed and the impossibility of physical examination of the abdomen through the area of the burn injury.
Often the first sign of erosive and ulcerative lesions of the gastrointestinal tract in burned patients is bleeding. Despite the fact that the frequency of damage to the mucous membrane of the stomach and duodenum in burned patients is quite high, only 10-30% of patients have characteristic clinical manifestations of bleeding from the gastrointestinal tract [17-21]. Initial symptoms of bleeding in the form of nausea, vomiting, dizziness, weakness and tachycardia are sometimes regarded as manifestations of the underlying disease. Often the first sign of the onset of bleeding is collapse, which in some cases is mistakenly associated with the manifestation of cardiovascular failure, myocardial infarction, etc.
The diagnosis becomes clear only when blood appears in the vomit and stool (admixture of “coffee grounds”, or melena). Even in patients with a perforated ulcer, clinical symptoms of complications may be absent - and perforated ulcers are diagnosed only during surgery or autopsy.
The main method for diagnosing erosive and ulcerative lesions of the gastrointestinal tract in burned patients is, of course, esophagogastroduodenoscopy (EGD). Only thanks to the widespread introduction of modern endoscopy methods into the practice of burn centers, it was possible to establish the true number of gastrointestinal lesions. In an endoscopic study of 37 patients with a burn area of more than 25% of the body surface, A. Gzaja et al. [22] found acute gastric and duodenal ulcers in 49% of cases. When conducting a systematic endoscopic study, it was found that acute ulcerations of the mucous membrane of the stomach and duodenum usually develop within the next 3-7 days after injury [19]. Often at the same time, the course of the disease is complicated by gastrointestinal tract complications. Moreover, according to the literature, potential predictors of gastrointestinal bleeding are the area and depth of the burn lesion, inhalation injury, duration of the prehospital period, and indices of the severity of the general condition [17, 21, 23, 24].
Prevention of the development of erosive and ulcerative lesions in burn victims should be comprehensive and include drug therapy, nutritional support and active tactics of local treatment of burn wounds. The main direction of prevention and treatment of erosions and ulcers is to maintain the pH of gastric juice at a level of more than 3.5 (antisecretory therapy). According to previous studies [21], based on a comparison of the frequency of gastroduodenal bleeding in burn patients, the advantage of using proton pump inhibitors (PPIs) for prophylaxis (4.4% of cases) compared with the group of patients without antisecretory therapy (13.3% of cases) was shown. ) and H2 blockers (16.8%). At the same time, this study included all patients with burns, regardless of the results of diagnosing erosions and/or gastrointestinal ulcers.
Thus, even against the background of complex treatment, it is not always possible to prevent the development of Curling ulcers and bleeding from them in burned people, so the issues of timely diagnosis, prevention and effective treatment of erosive and ulcerative lesions of the gastrointestinal tract remain relevant.
The purpose of the study was to assess the frequency of erosive and ulcerative lesions of the gastrointestinal tract in patients with burns, including those complicated by gastrointestinal tract, depending on the severity of the injury, complications of the burn disease and treatment characteristics.
Material and methods
The work is based on an audit of the medical records of 1833 patients (564 women and 1269 men) with burns aged from 15 to 93 years (on average 43±0.4 years), who were treated at the burn center of the National Medical Research Center for Surgery named after. A.V. Vishnevsky in 2001-2018. In 71.1% of cases, the cause of injury was flame (Table 1) .
Table 1. Etiological factor of burn injury
| Cause of injury | Number of patients | |
| abs. | % | |
| Flame burn | 1303 | 71,1 |
| Burn with boiling water, steam | 256 | 14,0 |
| Contact burn | 124 | 6,8 |
| Electrical injury | 106 | 5,8 |
| Chemical burn | 44 | 2,4 |
| Total | 1833 | 100 |
The total affected area in patients ranged from 1 to 98% of the body surface (on average 25±0.5%). Only 285 (15.5%) victims had I-II degree burns (ICD-10); the rest had superficial and borderline burns combined with deep III degree burns, the area of which occupied from 0.1 to 80% of the body surface (on average 12.4±0.4%).
Changes in the gastrointestinal tract were diagnosed based on clinical and instrumental data, mainly based on endoscopy. In patients with already identified erosive and ulcerative lesions of the gastrointestinal tract, a retrospective analysis of the clinical picture of the disease, as well as the incidence of gastroduodenal bleeding depending on the treatment, was carried out.
Statistical processing of the data obtained during the study was carried out. The arithmetic mean and standard error of the mean (M±m) were used as statistical parameters; statistical probability of an event (event frequency, %; P(A)=n(A)/n×100%, where n(A) is the number of observations with a distinctive feature A, n is the total number of observations). The reliability of differences was assessed by the significance coefficient (t-test) using the Student formula. With a sufficient number of observations, t≤2 indicated the significance of the differences between the two values with a probability of 95% or higher (p<0.05), and with t<2, the differences were considered random, unproven.
Results and discussion
As a result of the study, it was found that erosive and ulcerative lesions of the gastrointestinal tract complicated the course of the disease in 268 (14.6%) of 1833 patients with burns: erosion of the esophagus and stomach - in 84 (31.3%) patients, erosion and ulcers of the stomach and duodenum intestines - in 184 (68.7%) patients.
The localization of acute gastroduodenal erosions and ulcers according to endoscopy was different. Erosions, as a rule, were multiple, with a slight perifocal reaction, localized in the esophagus, body and fundus of the stomach. Acute ulcers were often combined with erosions and were single, localized in the antrum of the stomach and duodenum, involving the submucosal and muscular layers, and had a round or oval shape. Their bottom is smooth, without granulations, the edges are sharp. A red thrombus was often visible at the bottom; after bleeding stopped, the bottom was pale in color with a protruding brown pinpoint vessel.
In 76 (28.3%) of 268 patients with erosions and ulcers of the gastrointestinal tract, the course of the burn disease was complicated by gastrointestinal tract. At the same time, bleeding in the presence of erosions and ulcers of the gastrointestinal tract was observed much more often - in 64 (34.8%) patients, and in the presence of erosions - only in 12 (14.3%) patients.
When analyzing the clinical picture of 102 burned patients with gastrointestinal erosions and ulcers already diagnosed endoscopically, most of them showed an asymptomatic course of the disease (Table 2) .
Table 2. Structure and frequency of clinical symptoms in burn patients with endoscopically diagnosed erosions and ulcers of the gastrointestinal tract ( n=102, 100%)
| Clinical signs | Frequency of occurrence | |
| abs. | % | |
| Epigastric pain | 3 | 2,9 |
| Hiccups | 15 | 14,7 |
| Vomiting like "coffee grounds" | 12 | 12,7 |
| Hemorrhagic staining or “coffee grounds” in the gastric contents when the tube is inserted | 17 | 16,7 |
| Melena | 10 | 9,8 |
| Asymptomatic | 59 | 57,8 |
The frequency of erosions and ulcers of the gastrointestinal tract in burned patients, depending on gender, was comparable and amounted to 14.9% in men and 14% in women. However, in men more often than in women, the course of the disease was complicated by the development of gastrointestinal tract (31.2% and 21.5% of cases, respectively).
Erosive and ulcerative lesions of the gastrointestinal tract were most often observed in patients aged 20-39 years (Table 3) . At the same time, gastrointestinal tract lesions from erosions and ulcers of the gastrointestinal tract were more often observed in patients aged 40-59 years than in younger patients.
Table 3. Frequency of erosive and ulcerative lesions of the gastrointestinal tract and gastrointestinal bleeding in burn patients depending on age ( n=1833, 100%)
| Age, years | Total | With erosions and ulcers gastrointestinal tract | With gastrointestinal bleeding |
| <20 | 87 (4,75%) | 9 (10,3%) | 1 (11,1%) |
| 20—39 | 712 (38,8%) | 121 (17%) | 34 (28,1%) |
| 40—59 | 731 (39,9%) | 107 (14,6%) | 33 (30,8%) |
| >60 | 303 (16,5%) | 31 (10,6%) | 8 (25,8%) |
The incidence of erosive and ulcerative lesions of the gastrointestinal tract directly depended on both the total area of burns and the area of deep lesions. At the same time, erosions and ulcers of the gastrointestinal tract, depending on the total area of burns, occurred 5.9 times more often in groups of victims with burns of more than 30% of the body surface - 28.3% of cases, than with limited lesions - 4.8% of cases (p<0 .05) (Fig. 1) .
Rice. 1. The frequency of erosive and ulcerative lesions of the gastrointestinal tract in patients, depending on the total area of burns.
The frequency of erosions and ulcers of the gastrointestinal tract, depending on the area of deep burns, was 4.1 times higher in groups of victims with deep lesions of more than 20% of the body surface - 38.8% of cases, than with smaller areas of damage - 9.5% of cases (p< 0.05) (Fig. 2) .
Rice. 2. The frequency of erosive and ulcerative lesions of the gastrointestinal tract in patients, depending on the area of deep burns.
At the same time, the frequency of gastrointestinal tract lesions from erosions and ulcers of the gastrointestinal tract in patients depended more on the area of deep lesions than on the total area of burns. If with deep burns of up to 20% of the body surface and a total area of up to 30% of the body surface, gastrointestinal tract complications complicated the course of the disease in patients with almost the same frequency (22.1% and 23.1% of cases, respectively), then with deep burns of more than 20% of the body surface GIBs occurred significantly more often than in patients with a total affected area of more than 30% of the body surface (35.5% and 29.6% of cases, respectively).
The frequency of erosive and ulcerative lesions of the gastrointestinal tract in patients with burns when combined with inhalation injury was significantly higher than without it - 32.9% and 9.8% (p<0.05). Moreover, in patients with erosions and ulcers of the gastrointestinal tract, in 31.4% and 25.7% of cases, respectively, the course of the disease was complicated by gastrointestinal tract.
Of particular interest is the analysis of the frequency of diagnosis of erosive and ulcerative lesions of the gastrointestinal tract and gastrointestinal tract in victims with burns, depending on the time period after injury (Table 4) . The increase in the frequency of gastrointestinal tract bleeding was probably one of the manifestations of multiple organ failure against the background of severe burn disease with the development of complications.
Table 4. Frequency of erosive and ulcerative lesions of the gastrointestinal tract and gastrointestinal bleeding in patients with burns depending on the period after injury ( n=1833)
| Days after injury | Total | With erosions and ulcers gastrointestinal tract | With gastrointestinal bleeding |
| <3 | 344 (18,8%) | 63 (18,3%) | 12 (19%) |
| 4—9 | 647 (35,3%) | 121 (18,7%) | 36 (29,7%) |
| 10—19 | 398 (21,7%) | 63 (15,8%) | 20 (31,7%) |
| 20—29 | 168 (9,2%) | 16 (9,5%) | 5 (31,2%) |
| >30 | 276 (15,1%) | 5 (1,8%) | 3 (60%) |
The addition of pneumonia and sepsis in patients led to a more frequent development of erosions and ulcers of the gastrointestinal tract than each of these complications separately, and occurred much more often than in patients without infectious complications. At the same time, the frequency of erosions and ulcers of the gastrointestinal tract due to the presence of infectious complications also increased depending on the total area of burns (Fig. 3) and the area of deep lesions (Fig. 4) .
Rice. 3. The frequency of erosions and ulcers of the gastrointestinal tract in patients with burns, depending on the total area of damage and the presence of infectious complications.
Rice. 4. The frequency of erosions and ulcers of the gastrointestinal tract in patients with burns, depending on the area of deep damage and the presence of infectious complications.
At the same time, gastrointestinal tract complications in patients with burns complicated the course of the disease most often in patients diagnosed with pneumonia (25.5% of cases) and sepsis (20% of cases), especially when they were combined (45.5% of cases), compared with patients without infectious diseases. complications - 11.5% of cases (p<0.05).
In addition, a study was conducted of the frequency of gastrointestinal tract in patients with burns diagnosed with acute erosions and ulcers of the gastrointestinal tract, depending on the use of antisecretory drugs. At the same time, the patients were divided into two groups: in patients of the 1st group (n = 79), who were treated in 2001-2007, only H2-histamine receptor blockers (ranitidine, histodil, quamatel) were used in complex therapy; 2nd group (n=189) in 2008—2018. began to use PPIs (omeprazole, Losek). The patients of the compared groups were comparable in age and total burn area. A feature of patients in group 1 was a significantly (p<0.05) large area of deep burns and the frequency of detection of thermal inhalation injury (Table 5) , which in itself was a predictor of an increased risk of gastrointestinal tract.
Table 5. Characteristics of comparison groups of patients with burns
| Index | 1st group | 2nd group |
| Total patients with erosions and ulcers of the gastrointestinal tract | 79 | 189 |
| Patient age, years | 38,9±1,6 | 42,1±1,1 |
| Total area of burns, % body surface | 44,3±2,3 | 42,4±1,5 |
| Area of deep burns, % body surface | 27,9±1,9* | 22,1±1,3 |
| Frequency of thermal inhalation injury, % | 65,8%* | 38,1% |
Note. * — p<0.05 compared to 2008–2018.
It was revealed that, despite the specific antiulcer therapy, erosions and ulcers of the gastrointestinal tract in patients in group 1 were complicated by gastrointestinal tract in 41.8% of cases. In group 2, when using PPIs, these lesions were complicated by bleeding 1.8 times less often (p<0.05) (22.7% of cases), which confirms the data from the above studies [21].
Further analysis showed that, despite the presence of erosive lesions of the gastrointestinal tract, during the use of PPI drugs in patients of group 2, changes in the form of acute gastrointestinal ulcers were detected in 63% of cases, which is less than in group 1, where these changes were detected in 82.3% of cases (p<0.05).
At the same time, gastrointestinal bleeding from acute erosions of the esophagus and stomach, diagnosed in the first days after injury, was detected with the same frequency in the compared groups (14.3% of cases each). In the later stages after the injury, gastrointestinal ulcers from gastrointestinal ulcers were noted in the 2nd group only in 27.7% of cases - against 47.7% of cases in the 1st group.
A comparative analysis of the frequency of gastroduodenal bleeding in patients with erosions and ulcers of the gastrointestinal tract, depending on the area and depth of the burn lesion, showed that with the use of PPI, gastroduodenal bleeding was observed much less frequently with a total area of burns up to 50% of the body surface (Fig. 5) and an area of deep lesions up to 40 % body surface (Fig. 6) . At the same time, in victims with critical burns of more than 50% of the body surface, the risk of gastrointestinal tract infection remained high regardless of the use of antisecretory drugs.
Rice. 5. The frequency of bleeding from erosions and ulcers of the gastrointestinal tract in patients, depending on the total area of burns and the characteristics of treatment.
Rice. 6. The frequency of bleeding from erosions and ulcers of the gastrointestinal tract in patients, depending on the area of deep burns and the characteristics of treatment.
Analysis of deaths in 2001–2018. showed that out of 1833 patients with burns, 155 died, of which 90 (58.1%) had erosive and ulcerative lesions of the gastrointestinal tract diagnosed as a manifestation of multiple organ failure. Moreover, among all deaths with erosive and ulcerative lesions of the gastrointestinal tract, regardless of treatment, gastrointestinal tract diseases were detected in groups 1 and 2 with a similar frequency - 46.1% and 39.2% of cases, respectively. Among surviving patients with erosions and ulcers of the gastrointestinal tract, the frequency of gastrointestinal tract infections was lower and, with the use of PPI drugs, decreased by 2.2 times (from 37.5 to 16.7%) compared with the group of patients who used H2-histamine receptor blockers ( p<0.05).
Acute erosive-ulcerative gastroduodenal lesions in patients with cardiovascular diseases
Purpose of the review: To highlight the issues of pathogenesis, diagnosis, treatment of acute erosive-ulcerative gastroduodenal lesions in patients with cardiovascular diseases, as well as their role in thanatogenesis.
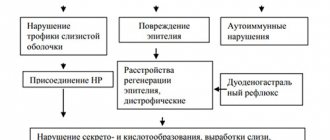
Main points of the review: There is an increase in the frequency of acute erosive and ulcerative gastroduodenal lesions in patients with cardiovascular diseases and other somatic pathologies. The role of bleeding caused by them in the thanatogenesis of these diseases is underestimated. In the pathogenesis of acute erosive gastropathy in patients with cardiovascular and other somatic pathologies, many factors are summed up, primarily acute or chronic ischemia of the gastroduodenal mucosa, as well as its age-related involution, helicobacteriosis, reflux gastritis, multiple organ failure, drug damage, etc. d.
Conclusions: Despite the increase in the frequency of OEGP and the unresolved issues of their prevention, diagnosis and treatment, in recent years there has been a tendency towards a decrease in fatal gastrointestinal tract complications associated with OEGP. Antisecretory therapy, increasingly administered to patients with ischemic heart disease and CVD during the period of active influence of risk factors, reduces the likelihood of gastroduodenal bleeding in therapeutic patients by at least 50%.
Multiple hemorrhages and acute erosions of the gastric mucosa are usually combined under the term acute erosive gastropathy. This group concept cannot, however, be considered successful, since it unites a large number of nosological forms that are diverse in etiology and pathogenesis and their complications - infectious, ischemic, medicinal, oncological lesions of the stomach, requiring the use of various methods of diagnosis and treatment. In addition, a combination of erosive lesions and acute ulcers of the mucous membrane, not only of the stomach, but also of the duodenum, is often found [1 – 15].
The etiology of acute erosive and ulcerative gastroduodenal lesions (AUGD) is extremely diverse. The most important etiological factors include taking certain medications - non-steroidal anti-inflammatory drugs (NSAIDs), cytostatics, corticosteroids, etc.; alcohol intoxication; chemical and physical gastroduodenal injuries; stress, shock, disseminated intravascular coagulation syndrome of various etiologies, severe injuries, burns (Curling ulcers), frostbite; chronic atrophic gastritis, Helicobacter pylori and heilmannii infection; renal (uremic gastropathy), liver failure (hepatogenic ulcers); oncological diseases, incl. stomach tumors; blood diseases (anemia, leukemia); infectious diseases, chronic lung diseases, diseases of the neuro-endocrine system, such as neurotrauma and other lesions of the brain (especially the posterior cranial fossa), the hypothalamic-pituitary system (Cushing's ulcer); gastrin-producing tumors (Zollinger-Ellison syndrome), hyperparathyroidism, diabetes mellitus (coma, ulcerogenic effect of insulin), etc. However, in recent years, attention has been drawn to the increase in the frequency of AEHP and the resulting gastrointestinal bleeding (GIB) in patients with cardiovascular diseases, primarily coronary heart disease (CHD) and cerebrovascular diseases (CVD) [1-7 , 16 – 30].
The increase in the frequency of OEGP in patients with cardiovascular diseases and other somatic pathologies allows us to speak, in fact, about their epidemic. According to various authors, the frequency of OEGP in such patients reaches 80-90%, and the gastrointestinal tract complications caused by them – 45-55%. The wide distribution of OEGP is associated with the aging population, the influence of unfavorable ecology, exogenous (alcohol, etc.) and endogenous intoxications, iatrogenic factors (increasing the number and volume of surgical interventions, taking various medications) [2-11, 19-24, 31 ].
Thus, a comparison of the results of studies of the frequency of OEGP based on materials from 6900 autopsies of people who died from various diseases from the groups of IHD and CVD in multidisciplinary emergency hospitals with a percentage of autopsies of at least 80% in 2000-2002. (2400 autopsies) and 2003-2008. (4500 autopsies) demonstrated that over the last decade it has increased by about a third, despite the introduction into clinical practice of measures for their prevention, diagnosis and treatment [2-8, 10, 11, 20-24]. It is important to note that these studies excluded observations with diseases that could be independent causes of the development of OEGP, in addition to cardiovascular diseases: surgical pathology of the digestive organs, chronic alcohol intoxication, chronic gastritis, oncological, endocrine (except for diabetes mellitus in 2003 -2008), and infectious and allergic diseases, as well as with renal and liver failure, cachexia, with a known history of taking medications that cause OEGP. The IHD group was represented by myocardial infarction (32%), large- and small-focal cardiosclerosis (20%); CVB group - ischemic cerebral infarctions and intracerebral non-traumatic hematomas (42%), long-term consequences of cerebrovascular accidents (3%). Background diseases were arterial hypertension (71.6% for ischemic heart disease and 86.6% for CVD), type 2 diabetes mellitus (4.3 and 1.2%, respectively), or a combination of both (18.6 and 9. 6%). Combined underlying diseases were represented by a combination of diseases from the groups of IHD and CVD (21%). The ratio of men to women was 1: 1.3 for IHD, 1: 1.1 for CVD, the average age of the deceased was 67.5 ± 3.2 years [2-8, 10, 11, 20-24].
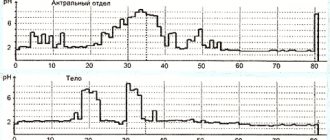
The results of the above studies showed that the frequency of OEGP was in myocardial infarction in 2000-2002. 10%, and in 2003-2008. – 18%, in chronic forms of IHD with chronic heart failure syndrome, 6 and 10%, respectively, in strokes – 8 and 14%, and in chronic forms of CVD – 4 and 9% (Fig. 1). In observations with a combination of diseases from the IHD and CVD groups, OHEP were detected much more often, in 21% of observations. Increase in the frequency of OEGP in 2003-2008. to a certain extent, can be explained by the inclusion in the analyzed group (compared to 2000-2002) of patients with diabetes mellitus, who amounted to 22.7% for coronary artery disease and 10.8% for CVD [2-8, 10, 11].
Fig. 1 Frequency (in %) of acute erosive and ulcerative gastroduodenal lesions in those who died from diseases from the ischemic heart disease and CVD groups in 2000-2002 (2400 autopsies, background disease - diabetes mellitus was excluded) and in 2003-2008. (4500 autopsies, background disease included - diabetes mellitus).
In patients with ischemic heart disease and CVD, acute erosions and ulcers were localized predominantly in the stomach (88 and 74%), in the duodenum (mainly in its bulb) - in 8 and 12% of patients, respectively, and combined damage to the stomach and duodenum was detected in 4 and 14% of observations, respectively. (Fig. 2). In the stomach, changes were more pronounced in the area of the body and lesser curvature (with ischemic heart disease - in 52±1.3%, with CVD - in 41.0±0.3%), less often - in the fundus (respectively, in 21±0. 7 and 27±0.5%) and antrum (in 27±1.5 and 25±0.2%) sections. In both IHD and CVD, superficial lesions predominated (acute erosions accounted for 47.3–87.9% of cases), rather than deep ones, such as acute ulcers [10, 11].
Fig. 2 Frequency (in%) of localization of acute erosions and ulcers in the stomach or duodenum in ischemic heart disease and CVD.
Timely diagnosis of OEGP is a problem that has not been solved to date, which is due to the peculiarities of their clinical manifestations. 30-90% of patients are characterized by an asymptomatic course, 46-58% - the absence of a typical and pronounced clinical picture, and in 25-42% of patients the symptoms of the underlying disease predominate. As a result, AEHP often goes undiagnosed until it suddenly presents with bleeding, often life-threatening. At the same time, the frequency of hemorrhagic complications of OEGP, including fatal ones, is 39-47% [3, 9, 11]. In patients with ischemic heart disease and CVD, the first manifestation of damage to the gastroduodenal mucosa is gastrointestinal tract in 25-55% of cases, and in most cases the diagnosis is first established at autopsy. It should be noted that the widespread decrease in the number of pathoanatomical autopsies, characteristic of many medical institutions, leads to an underestimation of the frequency and role of OEGP in thanatogenesis in patients with cardiovascular diseases. Most researchers agree that bleeding caused by OEGP develops much more often than is detected [2-11, 19-24].
The problem of treating gastrointestinal tract in patients with OEGP also remains unresolved. The results of conservative treatment of acute ulcers and erosions complicated by bleeding remain unsatisfactory, mortality ranges from 36.4 to 64-80% [1,3]. The outcomes of surgical treatment are also often unfavorable. Mortality after using various methods of surgical intervention is in the range of 24-44% [32-34]. Since gastrointestinal tract disorders during OEGP often occur subclinically and do not lead to significant hemodynamic disturbances, some authors believe that their clinical significance should not be exaggerated [35-37]. This opinion is opposed by data from other researchers, according to which bleeding prolongs the treatment period by an average of 4-8 days, increases the risk of repeated massive bleeding by 4 times and the risk of death by 2-4 times [2-8,36,38 ].
According to the above-mentioned pathological studies conducted in 2002-2008. in multidisciplinary emergency hospitals, gastrointestinal tract diseases of varying severity associated with OEGP developed in 67% of those who died with ischemic heart disease and 55% in CVD, but their role in thanatogenesis was different. The frequency of fatal gastrointestinal tract complications (direct causes of death) was for myocardial infarction in 2000-02. 4%, in 2003-08 – 3%, for chronic forms of IHD with chronic heart failure syndrome, 2 and 2%, respectively, for strokes – 2 and 1%, chronic forms of CVD in 2000-02. - 1%, and in 2003-08. no such deaths were identified (Fig. 3).
Fig. 3 Frequency (in%) of fatal bleeding in acute erosive-ulcerative gastroduodenal lesions in those who died from diseases from the ischemic heart disease and CVD groups in 2000-2002 (2400 autopsies, background disease - diabetes mellitus was excluded) and in 2003-2008. (4500 autopsies, background disease included - diabetes mellitus).
Thus, despite the increase in the frequency of AEGP, there is a trend towards a decrease in the fatal gastrointestinal tract complications associated with them [10,11,20,21]. It is known that antisecretory therapy, increasingly carried out in patients with coronary artery disease and CVD, increases the pH of the stomach contents to 5.0 - 7.0 units. during the period of active influence of risk factors, reduces the likelihood of gastroduodenal bleeding in therapeutic patients by at least 50% [2,3,35]. Although the share of gastrointestinal tract among the causes of death of patients with coronary artery disease and CVD did not exceed in 2000-08. 4%, the absolute number of such deaths is quite large, since nosological forms from these groups of diseases are the leading causes of death in the population. Taking into account the mortality rates for these diseases, 1 in 200 patients with myocardial infarction and 1 in 1000 with ischemic infarction or cerebral hematoma die from gastrointestinal tract. In 2009 in Moscow, among all causes of death, diseases from the IHD group amounted to 31.6, neoplasms – 19.8, and CVD – 18.3%. Among the nosological units, the leaders remain chronic forms of IHD (atherosclerotic and post-infarction cardiosclerosis - 24.1%, strokes - 6.6% and myocardial infarction - 5.5%) (Fig. 4). As a result, in Moscow, mortality from gastrointestinal tract diseases caused by OEGP is at least 1000 patients per year [10,11,20,21].
Fig.4 The most common (in %) diseases and their groups (CHD, CVD, cancer) - causes of death in Moscow in 2009.
The pathogenesis of OEGP in patients with cardiovascular diseases is not clear enough. A number of authors believe that the mechanisms of development of OEGP in patients with various somatic pathologies generally reflect the known pathogenesis of “stress” damage to the gastroduodenal mucosa, which is practically independent of the characteristics of the underlying disease. Consequently, OEGP develops as a result of peptic (acid) damage to the mucous membrane against the background of its deep ischemia with inhibition of all mechanisms of gastroprotection: secretion of bicarbonate, mucin, proliferation and regeneration of the epithelium [10,11,39-41]. It is known that with chronic circulatory failure, degenerative processes develop in many organs, including the digestive organs, especially in the gastric mucosa, which loses its resistance [15,28,29]. Other factors, such as helicobacteriosis, drugs, duodenogastric bile reflux, gastroparesis, etc., can also contribute to the development of OEGP. [1-3.37]. However, many researchers insist on the need to consider OEGP as an acute injury to the gastroduodenal mucosa associated with hyperacidity, in which the primary etiological factor is not Helicobacter pylori gastritis, as in peptic ulcers, and not long-term use of anti-inflammatory drugs, as in NSAID gastropathy, but severe somatic disease [29]. A morphological study conducted in deceased patients with ischemic heart disease and CVD, taking into account the known role of chronic atrophic gastritis and helicobacteriosis in the pathogenesis of erosive and ulcerative lesions of the stomach, did not reveal a significant difference in their frequency in two groups of observations - complicated and uncomplicated OEGP, which indicates the presence in cardiovascular diseases there are other important pathogenetic factors in the development of these complications [10,11].
Thus, the leading role in the pathogenesis of OEGP appears to be played by ischemia and microcirculatory disorders of the gastroduodenal mucosa, which cause reverse diffusion of H+, acidosis, depletion of buffer systems, death and impaired regeneration of epithelial cells [2,3,10,11, 20,21].
Morphological studies have shown that in chronic heart failure syndrome in patients with ischemic heart disease and, often, with CVD, chronic venous plethora, atrophy and sclerosis of all layers, sclerosis and hyalinosis of the walls of arterioles and small arteries develop in the gastroduodenal mucosa, cavernous structures are formed from sharply dilated veins and venules in the submucosal layer, reduction of the capillary bed, multiple superficial small foci of hemorrhage, ischemic and hemorrhagic necrosis, leading to the formation of acute erosions, more rarely, acute ulcers. An immunohistochemical study of the gastroduodenal mucosa in patients with ischemic heart disease and CVD revealed a decrease in proliferative activity and expression of growth factors and angiogenesis (TGF-β1 and VEGF), indicating inhibition of regenerative abilities and a decrease in protective functions. Such changes, typical of chronic ischemia, developed in the presence of severe stenosing atherosclerosis of the arteries of the stomach and duodenum [10,11,20,21]. In patients with coronary artery disease and acute heart failure syndrome, against the background of chronic changes in the gastroduodenal mucosa, its acute venous plethora, pronounced swelling of the submucosal and muscular layers, the appearance of extensive hemorrhages, large foci of ischemic and hemorrhagic necrosis, up to the submucosal layer, are noted. Cardiogenic shock, often against the background of chronic ischemic changes in the mucous membrane, is characterized by alternating foci of acute venous congestion and anemia, widespread thrombosis of the microvasculature, extensive multiple hemorrhages and confluent superficial foci of necrosis of the mucous membrane [10,11,20,21]. Such morphological changes in the stomach and duodenum in patients with cardiovascular diseases make it possible to substantiate the concept of ischemic disease of the stomach and duodenum, by analogy, for example, with ischemic intestinal disease. A feature of ischemic disease of the stomach and duodenum is the extremely rare development of necrosis (infarction) of the entire thickness of their walls, which is due to the extremely developed system of vascular anastomoses of these organs and multiple sources of blood supply. At the same time, the aggressive environment of the stomach, even with minor circulatory impairment and ischemia of the gastroduodenal mucosa, contributes to its damage.
The question remains open about the pathogenetic role of acute posthemorrhagic anemia in the development of exacerbations of coronary artery disease and CVD in gastrointestinal tract diseases caused by OEGP. A specially conducted retrospective analysis of medical records of inpatients and outpatients in multidisciplinary hospitals showed, even taking into account the incompleteness of information, that gastrointestinal tract complications preceded the development of myocardial infarction in 1.3%, and strokes in 0.22% of patients, which is of undoubted interest in terms of the relationship OEGP and ischemic lesions of the heart and brain [10,11,20,21].
Thus, there is an increase in the frequency of OEGP in patients with cardiovascular diseases and other somatic pathologies. The role of gastrointestinal tract diseases caused by OEGP in the thanatogenesis of these diseases is underestimated; the problems of their prevention, diagnosis and treatment remain unresolved. OEGP in patients with cardiovascular diseases is a morphological substrate of ischemic disease of the stomach and duodenum. With atherosclerosis, arterial hypertension and diabetes mellitus, the stomach and duodenum become one of the target organs, and damage to the heart and brain with ischemic heart disease and CVD aggravate the severity of pathological changes in the gastroduodenal mucosa. It should be taken into account, however, that in the pathogenesis of OEGP in patients with cardiovascular diseases and other somatic pathologies, many factors are summed up: acute or chronic ischemia of the gastroduodenal mucosa, its age-related involution and atrophy due to helicobacteriosis, reflux gastritis, drug damage, etc. .
Literature 1. Gelfand B.V., Guryanov V.A., Martynov A.N. and others. Prevention of stress-damage to the gastrointestinal tract in patients in critical conditions. Consilium Medicum 2005; 7 (6):464-71. 2. Vertkin A.L., Zairatyants O.V., Vovk E.I. Damage to the stomach and duodenum in patients with acute coronary syndrome. Attending Physician 2005; 1:66-70. 3. Vertkin A.L., Zairatyants O.V., Vovk E.I. Final diagnosis. – M.: GEOTAR-Media, 2008. 4. Kolobov S.V., Zayratiants O.V., Poputchikova E.A.. Morphological features of acute erosions and gastric ulcers in patients with myocardial infarction during treatment with the drug “Losek”. Morphological statements - 2002; 3(4):80-2. 5. Kolobov S.V., Zayratiants O.V., Khokhlova E.E., Frolova Yu.V. Acute erosive and ulcerative lesions of the stomach in emergency conditions in therapeutic patients. Abstract. report VI Congress of the Scientific Society of Gastroenterologists of Russia. – M., 2006. – P.24-25. 6. Kolobov S.V., Vertkin A.L., Zayratiants O.V., Poputchikova E.A., Mishutchenko O.P., Khokhlova E.E. Acute erosive and ulcerative lesions of the upper gastrointestinal tract in patients with myocardial infarction. Sat. proceedings of the II Congress of the Russian Society of Pathologists. – M., 2006. – T.1. — P.70-71. 7. Kolobov S.V., Zairatyants O.V., Vovk E.I., Poputchikova E.A., Mishutchenko O.P., Khokhlova E.E. Acute erosive and ulcerative lesions of the upper gastrointestinal tract. Sat. works “Current issues of morphogenesis in normal and pathological conditions.” – M.: Research Institute of Human Morphology of the Russian Academy of Medical Sciences, 2006. – P.17-18. 8. Kolobov S.V., Zairatyants O.V., Khokhlova E.E. Erosive and ulcerative lesions of the stomach and duodenum and gastrointestinal bleeding in patients with myocardial infarction. Sat. abstract report VII Moscow Assembly “Health of the Capital”. – M., 2008. – P.305-306. 9. Maev I.V. Erosive gastritis: a separate nosological form or a universal reaction of the mucous membrane to damage? Ross Journal of Gastroenterology, Hepatology, Coloproctology 2005; 15 (6):53-9. 10. Khokhlova E.E., Kolobov S.V., Zairatyants O.V., Zairatyants G.O. Acute erosive-ulcerative gastroduodenal lesions and bleeding in therapeutic and neurological patients. Sat. Proceedings of the III Congress of the Russian Society of Pathologists. – Samara: SamSMU, 2009. – P.325. 11. Yarema I.V., Kolobov S.V., Zayratiants O.V., Khokhlova E.E., Poputchikova E.A. Acute erosive-ulcerative gastroduodenal lesions in patients with coronary heart disease, cerebrovascular diseases and chronic obstructive pulmonary diseases. Surgeon 2009; 12:5-13. 14. Borchard F., Malferthemer P., von Herbay A. et al. Classification of erosions of the stomach results of a meeting of the study group of Gastroenterologic Pathology of the German Society of Pathology. Pathology - 1992; 13(5):249-51. 15. Steinberg KP Stress-related mucosal disease in the critically ill patient: risk factors and strategies to prevent stress-related bleeding in the intensive care unit. Crit Care Med 2002; 30(6): Suppl. 362-4. 16. Aruin L.I., Kapuller L.L., Isakov V.A. Morphological diagnosis of diseases of the stomach and intestines - M.: Medicine, 1998. 17. Grinevich V.B., Uspensky Yu.P., Grigoriev V.P., Kalinin A.V. Erosive changes in the gastroduodenal mucosa - a pre-ulcerative condition? Klin Med 1991; 69(11):57–9. 18. Grinevich V.B., Tkachenko E.I., Uspensky Yu.P. Classification of erosions of the mucous membrane of the stomach and duodenum. Klin Med 1996; 74(1):75–6. 19. Ivashkin V.T., Sheptulin A.A. Erosive and ulcerative lesions of the stomach and duodenum caused by non-steroidal anti-inflammatory drugs. Doctor 2001; 3:22-3. 20. Zairatyants O.V., Kolobov S.V., Khokhlova E.E., Poputchikova E.A. Acute erosive-ulcerative gastroduodenal lesions in therapeutic and neurological patients. Sat. scientific works of the conference in memory of Yu.L. Perov / Ed. Academician RAS and RAMS V.A. Tkachuk. – M.: Moscow State University Publishing House, 2009. – P.35-43. 21. Zairatyants O.V., Kolobov S.V., N.I. Polyanko, Khokhlova E.E. Acute erosive and ulcerative bleeding in therapeutic and neurological patients. Sat. abstract report VIII Moscow Assembly “Health of the Capital”. – M., 2009. – P.256-257. 22. Kolobov S.V., Zayratiants O.V., Loranskaya I.D., Simonova N.I., Poputchikova E.A. Erosive and ulcerative lesions of the upper gastrointestinal tract in patients with acute myocardial infarction. Emergency Therapy 2002; 3 (4): 63-7. 23. Kolobov S.V., Zayratiants O.V., Loranskaya I.D., Simonova N.I., Poputchikova E.A. Erosive and ulcerative lesions of the stomach and duodenum in acute myocardial infarction. Experimental and Clinical Gastroenterology 2003; 1:95-7. 24. Kolobov S.V., Vertkin A.L., Zayratiants O.V., Vovk E.I., Shamuilova M.M., Melnikova T.A., Frolova Yu.V. Treatment and prevention of gastrointestinal bleeding in patients with exacerbation of coronary artery disease. Therapist 2006; 6:15-28. 25. Bawk S. Stress ulcers — prevention of gastrointestinal bleeding in critical care units. Med J Austral - 1985; 142: (Special. Suppl):17-21. 26. Imhof M., Ohman G., Hartwig A. et al. Which peptic ulcers bleed? Results of a case-control study. DUSUK Study Group. Scand J Gastroenterol – 1997; 32 (2):131-8. 27. Jick SS The risk of gastrointestinal bleed miocardiae infarction and newly diagnosed. Pharmacotherapy – 2000; 4 (4):741-7. 28. Kantorova I., Svoboda P., Scheer P. et al. Stress ulcer prophylaxis in critically ill patients: a randomized controlled trial. Hepatogastroenterology 2004; 51(57):757-61. 29. Peterson WL The role of acid in upper gastrointestinal haemorrhage due to ulcer and stress-related mucosal damage. Aliment Pharmacol Ther 1995; 13(Suppl 1):43-6. 30. Robert G. Amer J Health-System Pharmacy 2002; 62 (10): (Suppl.2): 11-7. 31. Mikhailov A.P., Danilov A.M., Napalkov A.N., Shulgin V.L. Acute ulcers and erosions of the digestive tract: Textbook. – St. Petersburg: St. Petersburg Publishing House. Univ., 2004. 32. Stotsko Yu.M., Kurygin A.A., Musinov I.M. Vagotomy in the treatment of acute gastric ulcerations complicated by severe bleeding. Vestn hir 2001; 3:25-9. 33. Chernov V.N., Miziev I.A., Belik B.M. Prediction and prevention of acute ulcers and erosions of the stomach and duodenum in surgical patients. Vestn hir 1999; 6:12-5. 34. Sheptulin A.A. Gastropathy associated with the use of non-steroidal anti-inflammatory drugs: risk factors, treatment, prevention. Clin Perspectives in Gastroenterology and Hepatology 2001; 1:27-31. 35. Pimentel M, Roberts DE, Bernstein CN et al. Clinically significant gastrointestinal bleeding in critically ill patients in an era of prophylaxis. Am J Gastroenterol 2000; .95(10):2801-6. 36. Cook DJ, Griffith LE, Walter SD et al. The attributable mortality and length of intensive care unit stay of clinically important gastrointestinal bleeding in critically ill patients. J Crit Care 2001; 5(6):368-75. 37. Yang YX, Lewis JD Prevention and treatment of stress ulcers in critically ill patients. Semin Gastrointest Dis 2003; 14 (5):11-9. 38. Stollman N., Metz DC Pathophysiology and prophylaxis of stress ulcer in intensive care unit patients. J Crit Care 2005; 20 (1):35-45. 39. Loginov AS, Zvenigorodskaia LA, Potapova VB et al. The characteristics of peptic ulcer in subjects with concomitant ischemic heart disease. Ter Arkh 1998; 70 (3):9-13. 40. Spirt MJ Stress – related mukosal disease: risk factors and prophylactic therapy. Clin Ther 2004; 26 (6):197-213. 41. Raynard B., Nitenberg G. Is prevention of upper digestive system hemorrhage in intensive care necessary? Schweiz Med Wochenschr 1999; 129 (8): S.1605-1612.