Non-parasitic liver cyst (NPLC) refers to benign focal formations of the liver and is a cavity in the liver filled with fluid.
Currently, non-parasitic liver cysts are detected in 5–10% of the population. Moreover, in women they occur 3–5 times more often. The disease usually develops between 30 and 50 years of life.
True and false cysts are distinguished. True cysts differ from false ones by the presence of an epithelial cover of columnar or cubic epithelium on the inner surface. False cysts usually develop after injury.
Causes of the disease
The reasons for the occurrence of NCP have not yet been fully elucidated. Currently, the prevailing opinion is that liver cysts arise from aberrant bile ducts, i.e., during embryonic development, individual intralobular and interlobular bile ducts are not connected to the biliary tract system. Liver cysts may occur when taking certain medications (estrogens, oral contraceptives).
Sign up for a consultation First consultation is free!
Varieties and classification
A cyst is a general term for several different forms of neoplasm. First of all, cysts are divided into congenital and acquired. Congenital formations are also called “true”; their walls are lined with epithelial cells. They come in different sizes, sometimes multi-chambered. They may not manifest themselves in any way; they are often diagnosed accidentally during examination. Acquired cysts are called “false” cysts.
Cysts can be multiple or single. They are distinguished not by the number of single formations, but by the number of cavities limited by the wall. A condition in which there are many single cysts in one segment of the liver is called polycystic disease.
Due to the fact that cysts form during parasitic infestations, it is important to differentiate the pathology caused by echinococcus or protozoa. Differentiation is carried out only by the presence or absence of signs of echinococcosis. Treatment of a parasitic disease is specific and is aimed primarily at eliminating the infection and preventing the parasite from reproducing.
Symptoms of the disease
The clinical picture of NPC is usually poor and nonspecific. Most often, liver cysts are accidentally detected during ultrasound of the abdominal organs. Manifestations of the disease depend on the size of the cyst, its location, as well as the effect of the cyst on neighboring organs. Enlargement of the cyst also leads to atrophic changes in the liver tissue.
The most common complaint with solitary liver cysts is pain in the upper right quadrant or epigastric region. In many cases the pain is constant. Patients also note a quick feeling of fullness and abdominal discomfort after eating.
Benign focal formations of the liver: age-related psychosomatic aspects
Non-parasitic liver cysts (NLCs) are benign focal formations of the liver and are a cavity (or cavities) in the liver filled with fluid.
There is an increase in the incidence of NPC everywhere, which is mainly due to the widespread use of modern diagnostic methods that allow visualization of the liver intrastructure: ultrasound, computed tomography (CT), magnetic resonance imaging (MRI), angiography, etc. According to H. Sancher et al. (1991), NPC is detected in 5–10% of the population. Moreover, in women they occur 3–5 times more often. The disease usually develops between 30 and 50 years of life.
The reasons for the occurrence of NCP have not yet been fully elucidated. Thus, according to E. Moschowitz, R. Virchow, the formation of cysts is associated with inflammatory hyperplasia of the bile ducts at the time of embryogenesis with their subsequent obstruction. S. Henson and co-authors believe that this process serves as the basis for neoplasm.
Currently, the prevailing opinion is that liver cysts arise from aberrant bile ducts, i.e., during embryonic development, individual intralobular and interlobular bile ducts are not connected to the biliary tract system. The lack of involution of these passages is the reason for the development of liver cysts; as a result of the secretion of their epithelium, fluid gradually accumulates in them, and they turn into a cyst. This origin of liver cysts is confirmed by the fact that there is no bile in the secretion; in addition, liver cysts almost never communicate with normal bile ducts. Many scientists proceed from the fact that liver cyst damage is either an independent genetic unit with autosomal dominant heredity, or cystic changes in various organs are caused by a single genetic defect with varying prevalence.
The possibility of liver cysts occurring when taking certain medications (estrogens, oral contraceptives) is also discussed.
True and false cysts are distinguished. True cysts differ from false ones by the presence of an epithelial cover of columnar or cubic epithelium on the inner surface. False cysts usually develop after injury.
There is no generally accepted classification of liver cysts. In practice, the most convenient classification of NCPs is proposed by A. A. Shalimov and co-authors (1993), according to which NCPs are distinguished as follows:
- According to the structure of the cyst wall:
- true,
- false.
- By number of cysts:
- single,
- multiple,
- polycystic liver disease.
- According to the clinical course:
- uncomplicated,
- complicated.
Complications include: suppuration, bleeding into the cyst cavity, wall rupture, portal hypertension, mechanical jaundice, liver failure. When a cyst ruptures, secondary infection, formation of external and internal fistulas, and torsion of the cyst pedicle are possible. These complications occur in 5% of cases. Malignant degeneration is rare.
It is believed that the clinical picture of NPC is poor and nonspecific. Most often, liver cysts are accidentally detected during ultrasound of the abdominal organs. Manifestations of the disease depend on the size of the cyst, its location, as well as the effect of the cyst on neighboring organs. Enlargement of the cyst also leads to atrophic changes in the liver tissue.
The most common complaint with solitary liver cysts is pain in the upper right quadrant or epigastric region. In many cases the pain is constant. Patients also note a quick feeling of fullness and abdominal discomfort after eating.
Previously, an important symptom was considered to be the detection on palpation of a moderately intense massive tumor-like formation that moves with breathing along with the liver. It has been reported that palpable liver cysts are usually felt as tight-elastic and easily fluctuating painless tumors. It should be noted that even large liver cysts are inaccessible to palpation due to their location deep in the liver parenchyma or localization on the diaphragmatic surface of the organ.
The appearance of other, also nonspecific symptoms: weakness, excessive sweating, loss of appetite, nausea, shortness of breath - is usually associated with an increase in the size of the cysts, but most likely this is a consequence of the reaction of other organs - the gallbladder, duodenum, etc.
The variety and nonspecificity of clinical symptoms dictate the need to examine the patient in order to determine or exclude concomitant somatic and mental pathology.
NPCs should first of all be differentiated from parasitic cysts. For this purpose, specific serological blood tests are performed (indirect hemagglutination reaction and enzyme immunoassay for echinococcosis). In some cases, there is a need for differential diagnosis with hemangioma, cystadenoma, retroperitoneal tumors, tumors of the intestine, mesentery, pancreas, hydrocele of the gallbladder and metastatic tumor lesions of the liver.
Polycystic liver disease is often combined with polycystic kidney disease, pancreatic disease, and ovarian disease. Polycystic liver disease, like a solitary cyst, is often asymptomatic and detected by chance during examination for another pathology. In most cases, the course of the disease is favorable. Clinical symptoms are observed as the disease progresses, which usually occurs after 40–50 years. With an increase in the volume of polycystic formations, patients complain of discomfort in the right hypochondrium and epigastrium, heartburn, and belching, which is associated with pressure from the enlarged liver on neighboring organs. During the study, hepatomegaly is determined. Palpation: the liver is dense, lumpy. Liver function tests are usually unchanged. Violation of the synthetic function of the liver is detected in the later stages with pronounced degeneration of the liver parenchyma. With massive spread of the process, when most of the liver parenchyma is replaced, terminal liver failure develops. The situation is aggravated by chronic renal failure - the outcome of polycystic kidney disease.
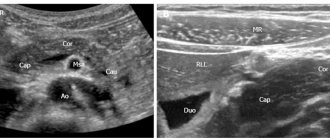
Echography occupies a leading place in the diagnosis of NPC, due to the high information content, harmlessness and general availability of this method. Echographically, liver cysts are cavities delimited by a thin wall (1–2 mm) with an anechoic internal space, which is explained by the difference in the density of the fluid and liver parenchyma. Their shape can be round or oval. The diagnosis is based on the following signs detected by ultrasound: 1) the presence of clear, even contours with a clearly visible posterior wall; 2) absence of internal reflections; 3) identifying the increase in echo signals behind the formation.
In the presence of an intraluminal septum, the ultrasound image of a liver cyst may have a spotty pattern. In case of complicated cysts (hemorrhage or infection), when intraluminal “echo” signals are detected, it is difficult to exclude a malignant tumor. In doubtful cases, CT, MRI, angiographic and radiological research methods are used. In certain situations, it is considered advisable to perform percutaneous puncture of the cyst under ultrasound control, followed by bacteriological and cytological examination of the material.
Traditionally, the problem of NCP was dealt with by surgeons who developed diagnostic methods and surgical treatment tactics. Patients with NPC came to the surgeon's field of view when a focal liver formation was detected, while patients with complications and uncomplicated cysts exceeding 5 cm in diameter received surgical treatment.
Therapeutic tactics for NCP have not yet been developed. The purpose of our work was to study the therapeutic, age-related and psychosomatic aspects of NCP.
The presented material is based on the results of a survey of 93 patients (72 women and 21 men) aged from 20 to 82 years, average age - 56.9 + 11.3 years. The patients were divided into two groups based on age.
Solitary NPC was identified in 37 people, 56 patients with NPC had two or more cysts. The average age of patients with solitary liver cysts (27 women and 10 men) was 53.5+11.6 years. The average age of patients with multiple liver cysts was 59.3 + 10.6 years (p < 0.05).
An analysis of complaints showed that pain in the right hypochondrium was significantly more common in patients with liver cysts larger than 5 cm in diameter. Pain and discomfort in the epigastrium were almost 2 times more common in the group of patients with small liver cysts than with large ones. Large cysts in surgery are considered to be those larger than 5 cm in diameter. Symptoms of intestinal and gastric dyspepsia occurred in patients of both groups with the same frequency. From this we can conclude that pain in the right hypochondrium is a true clinical manifestation of NCP.
It is interesting to note that such a symptom as general weakness was significantly more common in the group of patients with cysts less than 5 cm in diameter than among patients with large liver cysts. Since in most patients we did not find serious organic reasons that explain general weakness, then, most likely, the appearance of this complaint is due to various personal characteristics, including the patient’s attitude towards his illness.
Pain in the right hypochondrium bothered more than half (52%) of patients with NPC, which first of all required clarification of the condition of the gallbladder. According to the results of ultrasound, the gallbladder remained intact in 20% of patients in the group under 57 years of age and in only 8% in the group over 57 years of age. Dysformia (impaired shape) of the gallbladder was more common in younger patients (39%), possibly due to the “transition” of existing dysformia to the cholelithiasis section with age. Bile dyscrasia was determined in both age groups with the same percentage (2 and 3%). Gallstone disease (GSD) was diagnosed (at various times) in 34% of patients with NPC. Cholelithiasis and cholecystectomies were more often observed in the older age group, which seems quite natural. However, stones in the gallbladder in one form or another (gallstone disease or cholecystectomy) were diagnosed much more often in patients with NPC than in the general population. The presented data suggest a possible connection between the presence of a liver cyst and increased stone formation in the gallbladder, which can be explained by a violation of the formation of the biliary system in ontogenesis.
Heartburn bothered 15% of patients with NCP, which was qualified as a manifestation of gastroesophageal reflux disease, confirmed by 24-hour intragastric pH-metry of the esophagus and stomach. However, EGD revealed esophageal lesions in only 3% of patients. Also, according to endoscopy, cardia insufficiency and hiatal hernia were somewhat more common in the older age group, which is likely due to a general decrease in muscle tone with age.
About 20% of patients with NCP noted various symptoms of intestinal dyspepsia (flatulence, rumbling and transfusion along the intestines, stool disorders), which in most cases were a consequence of impaired bile excretion.
Analysis of laboratory data showed that the average level of GGTP and total bilirubin in the group of patients with liver cysts larger than 5 cm was statistically significantly higher than in patients in the group with liver cysts less than 5 cm in diameter (Table 1).
The data obtained suggest the possibility of a direct relationship between the size of the cyst and the presence of signs of cholestasis.
As is known, the attitude towards the disease can be adequate and pathological, which depends primarily on the patient’s personality: the presence or absence of accentuation of character, the formation of personality disorders, a tendency to neurotic forms of reaction or the presence of any mental disorder. Of course, the formation of the “internal picture of the disease” is also influenced by the course and prognosis of somatic disease, social factors and a number of other reasons.
The results of determining the level of anxiety as a current state and as a stable personality characteristic turned out to be interesting. In our study, low and moderate reactive anxiety (RT) were significantly more common than high ones. Personal anxiety (PT), on the contrary, was high or moderate in a greater number of patients. The lower level of RT compared to the level of RT is due to the fact that by the time of admission to the hospital, patients had calmed down to a large extent: already before the start of treatment, they “left the threshold” or transferred to doctors most of the anxieties and experiences that tormented them in the “usual » life. However, it should be remembered that an increase in RT in patients with non-parasitic liver cysts should not be ignored, since such a characteristic of the patient’s personality is certainly important and is reflected in the course of the disease.
Using the Mini-Mult questionnaire, the psychological characteristics of patients with non-parasitic liver cysts were studied. The assessment of the reliability of the sincerity of the answers was positive in most cases, only in two cases there were increased scores on the lie scale and in four cases on the reliability scale. The value of the correction index for all tested was within the normal range. As a result of deciphering the questionnaire, the entire spectrum of characterological types was represented in patients with NCP, however, in more than half of the tested patients (60%), the scores on all scales were within normal limits. In 10 out of 19 patients, there was a combination of several characterological types, each of them was taken into account separately.
The hysterical type was most often identified (27%). Almost a third of patients were prone to neurological defensive reactions of the conversion type. They “used” the symptoms of physical illness as a means of defense, often thereby avoiding responsibility. All problems were resolved by “going into illness.” The main feature of such people is the desire to appear larger, more significant than they really are, to attract attention, to arouse admiration at all costs, a “thirst for recognition” (according to K. Schneider). The feelings of such people are superficial and their interests are unstable.
The hypochondriacal type (astheno-neurotic) was determined in 15% of the examined patients. These are slow, passive patients who take everything on faith, with unsatisfactory ability to adapt, as a result of which they easily lose their balance in conditions of social conflicts.
Anxious-hypochondriac character type (psychasthenia scale) was diagnosed in 13% of patients. Such people are characterized by anxiety and suspiciousness, fearfulness, indecisiveness and a tendency to doubt.
The depression scale was elevated in 8% of patients. These patients may be characterized as sensitive, timid and self-conscious, and prone to anxious reactions. In business they are diligent, conscientious, highly moral and obligatory, but at the same time they are not able to make a decision on their own, they do not have self-confidence, and at the slightest failure, such people show mood disorders with a pessimistic assessment of the situation.
The schizoid type of behavior (schizoidity scale) was also determined in 8% of patients; a common feature of this type is a combination of increased sensitivity with emotional coldness and alienation in interpersonal relationships.
Another 8% of patients were of the paranoid type. The main feature of such people is a tendency to form highly valuable ideas; they are characterized by mental rigidity, aggressiveness, and resentment. Because of this, paranoid individuals are extremely sthenic and stubborn in achieving what they want. These individuals are extremely egocentric, subjective, cannot be persuaded, and have inflated self-esteem.
The psychopathic type was identified in 4% of patients, who were distinguished by more pronounced disharmony of personality and potentially the possibility of disruption of social adaptation. Such people are aggressive, conflict-ridden, and disregard social norms and values. Their mood is unstable, they are touchy, excitable and sensitive.
Personality traits are an important, but far from the only factor that determines the attitude towards one’s own illness. The attitude towards the disease and everything that is connected with it and what it influences is determined by three most important factors (A. E. Lichko, N. Ya. Ivanov, 1980):
- the nature of the somatic disease itself;
- a personality type, in which the most important component is determined by the type of character accentuation;
- attitude towards this disease in the environment that is significant for the patient, in the microsocial environment to which he belongs.
Under the influence of these three factors, an attitude towards illness, treatment, doctors, one’s future, work, family and friends, others, etc. is developed.
In our work, we used the Personality Questionnaire of the Bekhterev Institute (LOBI) to determine the types of attitudes towards the disease and other personal relationships associated with it in patients with chronic somatic diseases.
We were unable to identify a type of attitude toward the disease specific to NCP. But the most common types of attitude towards the disease (depending on the age of the patients) have been established (Fig. 1).
As can be seen from the presented graph, with age the number of patients with harmonious and neurasthenic types of attitudes towards the disease decreases and the number with anxious, obsessive-phobic, sensitive and paranoid types of attitudes increases.
Among the diagnostic types of attitude towards the disease in our patients, the paranoid type predominated and the melancholic type was completely absent, but no statistically reliable data were found.
The results obtained indicate that NCP as a somatic disease is a diagnosis whose significance reaches the level of mental trauma. The identification of a paranoid attitude towards the disease in 22% indicates not only the severity of psychogenicity, due to an understanding of the seriousness of the disease, but also characterizes the personality traits of the patients. Paranoid reactions are psychopathologically completed psychogenic states and indicate the depth of the existing personal pathology (often the presence of a mental illness).
Psychiatric diagnosis involved qualification of the condition in accordance with the criteria of ICD-10 (1992).
When comparing the identified pathology, no statistically significant differences were obtained, but it should be noted that in the group of patients under 57 years of age, traits of emotional instability and asthenic states were almost 2 times more likely to be noted, and depression, adaptation disorders, neurasthenic and somatoform disorders clearly predominated among more older patients, while anxiety and schizotypal disorders were diagnosed in both groups with the same frequency.
Consequently, patients with NCP experience various psychopathological symptoms—syndromes that often have independent dynamics and form the so-called “second disease,” which significantly aggravates the course of existing somatic diseases.
Thus, the therapist’s tactics in relation to patients with NPC (sizes up to 5 cm in diameter) are determined by: the function of the gallbladder; symptom of intestinal dyspepsia; intrahepatic cholestasis syndrome (minor); mental deviations.
Our experience of working with patients with NCP has shown that most complaints in such patients are due to the presence of concomitant somatic and mental disorders. Drug therapy for the identified pathology has a positive effect on the “clinical manifestations” of NPC.
According to indications in the treatment of our patients, we used drugs that affect the gallbladder. For hyperkinetic dyskinesia of the gallbladder, treatment was aimed at overcoming spasm of smooth muscles - antispasmodics were prescribed (duspatalin, dicetel, odeston, no-spa); in case of hypokinetic - to activate its motor activity (choleretics: bile acid preparations - allochol, cholenzym, enzistal, panzinorm, festal; synthetic choleretics - nicodine, oxafenamide, nicotinamide, odeston, febihol; herbal remedies - corn silk, sandy immortelle, rose hips, tansy ; hydrocholeretics - mineral waters; true cholekinetics - cholecystokinin, pituitrin, magnesium sulfate, barberry preparations, Berberis-homaccord, holagol). Choleretic therapy led to the normalization of the biliary, motor-evacuation, and anti-inflammatory (drainage) functions of the gallbladder.
Treatment of erosive and ulcerative lesions of the upper gastrointestinal tract in patients with NPC was carried out according to generally accepted standards of treatment (omeprazole, Pariet, Nexium, sucralfate or de-nol; when indicated, eradication therapy was carried out with Klacid and amoxicillin while taking proton pump inhibitors). For the treatment of gastroesophageal reflux disease, prokinetics (Motilium) and antacid drugs (Almagel, Maalox) were added to antisecretory drugs as needed.
To eliminate the symptoms of intestinal dyspepsia, probiotics (Hilak Forte, Enterol, Intetrix), enzyme preparations (Mezim Forte, Creon, Pancreatin), and, if necessary, hepatoprotectors (Essential-N, Heptral, Corsil) were prescribed.
When selecting drug therapy, the characteristics of psychosomatic relationships in each individual patient were also taken into account. In the presence of neurotic disorders, psychopharmacotherapy was of an additional, auxiliary nature. Somatic treatment included tranquilizers (Relanium, fenozepam, clonazepam, less often Grandaxin), small doses of small neuroleptics (sonapax, eglonil, etapyrazine). When diagnosing depression, on the contrary, antidepressants (amitriptyline, Coaxil, Profluzac, Zoloft), tranquilizers and minor antipsychotics were the main drugs, and gastroenterological therapy was only symptomatic, of course, if a somatic examination excluded severe pathology of the gastrointestinal tract.
The results of combination therapy - hofitol (1 tablet 3 times a day before meals for at least 3 weeks) and Eglonyl (100-200 mg/day in 2 doses for at least 3 weeks) in patients with NPC were interesting (Table 2).
| Table 2. Clinical results of using Chofitol and Eglonil |
Blood tests during two-week therapy showed a decrease in the level of liver enzymes - AST and ALT, and significantly (p < 0.05) lower levels of GGTP and total bilirubin. The positive result of this therapy is due to the widespread prevalence of diffuse diseases of the liver, gall bladder and mental deviations in our patients.
It is important to emphasize that the drug therapy we conducted did not affect the size of the cysts, their localization and the short-term prognosis of the disease.
Moving on to the issues of treating NCP directly, it should be noted that today doctors only have surgical methods, but the issue of tactics for managing such patients currently remains controversial: there is no consensus among surgeons regarding the methods of surgical treatment of NCP, which generally depend on their size and location. The most radical method of surgical treatment is liver resection. However, to perform this intervention, a comprehensive and scrupulous comprehensive study of patients is necessary in order to determine the localization and extent of the lesion in lobes and segments, its relationship with vascular-secretory elements, the functional state of the liver, etc.
Recently, minimally invasive interventions for NPC have become widespread, such as percutaneous punctures followed by sclerosis of the cyst and laparoscopic operations.
Also widely discussed is the tactic according to which, for asymptomatic small liver cysts of stable size, one should refrain from surgery and observe them over time. Most researchers suggest that cysts up to 5 cm in diameter should be considered “small”. It is believed that a cyst of this size does not have negative effects: compression of surrounding tissues, stretching of the Glyson capsule, or increase in liver mass. G. G. Akhaladze and co-authors (1999) believe that patients with cysts up to 7 cm in diameter do not need surgical treatment. Nevertheless, it is generally accepted that NPCs less than 5 cm in diameter are not subject to immediate surgical treatment, but require dynamic monitoring.
In conclusion, it should be noted that all patients with NPC, regardless of the size of the focal formation, need a thorough somatic and psychological examination. The identified concomitant pathology allows us to clarify the genesis of complaints and determine the correct tactics for further management of the patient. When complete psychogenic reactions develop in the examined patients, complex treatment with the necessary psychotropic drugs is recommended.
V. M. Makhov , Doctor of Medical Sciences, Professor L. V. Romasenko , Doctor of Medical Sciences, Professor T. V. Turko , Candidate of Medical Sciences MMA named after. I. M. Sechenova, Moscow
For questions regarding literature, please contact the editor.
Operations
In recent years, transparietal punctures of cysts under ultrasound or CT control have become widespread. After aspiration of the contents, a 96% solution of ethyl alcohol is injected into the lumen of the cyst to harden the inner lining of the cyst. This operation is effective for cysts up to 5 cm in size. If there is no effect from these treatment methods or the cyst is larger, an operation is indicated - laparoscopic excision of the cyst area, followed by de-epithelialization of the inner lining of the cyst with argon-enhanced plasma or a defocused laser beam. Similar tactics are used for polycystic liver disease. In case of complicated polycystic liver disease (suppuration, bleeding, malignancy, compression of the bile ducts, portal or vena cava by large cysts), surgical treatment is indicated. Typically, fenestration is performed (opening cysts protruding above the surface of the liver), followed by deepithelialization of the inner lining of the cyst.
Have questions?
Leave your phone number and we will call you back
Pathogenesis
The formation of a parasitic cyst from the moment of infection includes 3 stages:
- Penetration of the parasite first into the blood and then into the hepatic system, forming a cyst capsule with small contents. At this stage, the liver is able to fully perform its functions, the immune system works as usual. The stage is completely asymptomatic.
- An increase in the size of the tumor, the formation of a specific stalk, which falls into the abdominal cavity. The tumor reaches such a size that it begins to compress the liver and nearby organs, causing severe pain to the patient.
- Rapid progression of the process, which is accompanied by a pronounced inflammatory process around the cyst and subsequent suppuration. In rare cases, it is at this stage that the cyst ruptures with damage to the liver structures.
Our leading specialists
All specialists
Evseev Maxim Alexandrovich
- Deputy Chief Physician for Surgery
- Surgeon
- Bariatric surgeon
- Oncologist
- Doctor of Medical Sciences
- Professor
- Doctor of the highest category
Mirgatia Irakliy Olegovich
- Head of the surgical department
- Surgeon
- Oncologist
Vladykin Alexey Leonidovich
- Surgeon
- Bariatric surgeon
- Oncologist
- Candidate of Medical Sciences
- Doctor of the highest category
Alekseev Mikhail Sergeevich
- Surgeon
- Leading doctor price list
- Doctor of Medical Sciences
Fedotov Stanislav Viktorovich
- Head of the operating unit
- Surgeon
- Bariatric surgeon
- Leading doctor price list
- Doctor of the highest category
Balarev Anton Sergeevich
- Surgeon
- Oncologist
- Candidate of Medical Sciences
- Doctor of the highest category
Efimkina Jennet Orazmammetovna
- Surgeon
Rozumny Ilya Arkadievich
- Surgeon
Kharitonov Andrey Ivanovich
- Surgeon
- Doctor of the highest category
Titkov Boris Evgenievich
- Chief Physician of the Hospital Center
- Surgeon
- Oncologist
- Doctor of Medical Sciences
- Professor
- Academician AMTN
- Surgeon of the highest qualification category
Diet for liver cysts
Diet for liver cysts
- Efficacy: no data
- Terms: 1-6 months/lifetime
- Cost of products: 1500-1600 rubles. in Week
Diet for liver inflammation
- Efficacy: therapeutic effect after 10 days
- Timing: constantly
- Cost of products: 1300-1400 rubles per week
Dietary nutrition for cystic neoplasms in the liver involves avoiding some foods and including others in the diet.
It is prohibited to use:
- sweets;
- carbonated drinks;
- spices, seasonings;
- coffee;
- fried, salted, smoked and spicy dishes.
Permitted for use:
- greenery;
- fish;
- vegetables and fruits;
- cellulose;
- fermented milk products;
- sea buckthorn and rose hips.
The diet involves eating foods that have undergone deep heat treatment. The diet must contain easily digestible protein (at least 120 g per day) and a minimum amount of fat (no more than 80 g). Daily calorie content should not exceed 3000 Kcal. The meal plan must be fractional.
Advantages of the Hospital Center
Individual treatment regimen for each patient
For each patient, it is mandatory, even at the pre-hospital stage, that an individual treatment regimen is developed, taking into account all the characteristics of the body: age, health status, medical history, etc. – this approach allows you to minimize risks both during surgery and in the postoperative period, and as a result, ensure the fastest possible rehabilitation with a minimum period of hospital stay.
Multidisciplinary approach
The medical staff of the Hospital Center is a single team made up of expert doctors of different specializations, which allows for a multidisciplinary approach. We treat the patient, seeing in front of us not a list of diseases he has, but a person whose problems are interconnected and interdependent. The therapeutic measures taken are always aimed at overall improvement of the patient’s health, well-being and quality of life, and are not limited to eliminating the symptoms of a specific disease.
Surgical treatment of any level of complexity
The operating doctors of the Hospital Center are proficient in advanced and high-tech methods of performing operations. The combination of highly qualified doctors and innovative equipment allows for surgical treatment of the highest level of complexity.
High-tech, minimally invasive treatment methods
The basis of the treatment methodology carried out at the Hospital Center is the principles of minimizing risks for the patient and the fastest possible rehabilitation.
The implementation of such an approach is possible only by using the most high-tech techniques, modern equipment and the application of the latest achievements of medical science.
The qualifications of doctors combined with modern equipment allow us to successfully implement this approach to treatment.
Fast-track surgery
Fast-track is a comprehensive technique that allows you to minimize the length of a patient’s stay in the hospital without compromising the quality of treatment.
The approach is based on minimizing surgical trauma, reducing the risk of postoperative complications and accelerating recovery after surgery, which provides our patients with a minimum hospital stay.
Thanks to this approach, even complex operations such as cholecystectomy require a hospital stay of no more than 3 days.
Personal medical supervision in the postoperative period
To completely exclude the development of possible complications, the early postoperative period is spent in all patients, regardless of the complexity of the operation, in the intensive care unit under the individual supervision of a resuscitator.
The transfer of the patient to the ward is carried out only in the complete absence of even the minimal possible risks.
Informing relatives 24/7
We are as open as possible and show care not only for the patient, but also for his loved ones. Information about patients' health status is provided to relatives seven days a week, 24 hours a day.
Visiting patients is also possible at any convenient time.
Highly comfortable single and double rooms
Patients are offered spacious, comfortable rooms for single and double occupancy, equipped with everything necessary for rest and recovery.
In the children's department, our young patients are accommodated together with their parents.
Tax deduction
According to the tax legislation of the Russian Federation, each patient has the right to compensation of up to 13% of the amount spent on his treatment, as well as the treatment of close relatives.
Our specialists will prepare for you a package of documents for the tax office for a refund of 13% of the amount of treatment expenses, and will also give recommendations on various ways to interact with the tax office.
Treatment of liver cysts with folk remedies
Herbal infusions and decoctions can provide powerful support to a weakened body affected by neoplasms. However, uncontrolled use of herbal infusions can have a negative effect on the entire body. Before starting treatment with folk remedies, it is recommended to consult your doctor about compatibility with the main drug therapy. Plants used in recipes:
- celandine (juice);
- burdock (root and juice);
- elecampane;
- tenacious bedstraw;
- yarrow;
- milk thistle;
- pine nut (shell).
In addition to medicinal herbs, traditional medicine recommends consuming quail eggs and kombucha infusion.