- home
- general surgery
- Cholelithiasis
- Gallstones - causes, symptoms, treatment, surgery
Gallstones are one of the most commonly diagnosed diseases of the digestive system. The size of the stones can vary; there are small stones - less than 3 cm, and large stones. Depending on the number of stones, we can talk about single or multiple formations. Stones can have different shapes: round or multi-faceted. But even one stone can be dangerous.
Today, this disease is diagnosed in more than 10% of the adult population, and after 45 years it is found in every third person. Statistics show that every decade the number of cases doubles. Unfortunately, one can only guess about the true number of people with cholelithiasis, since at the initial stage there are no clear signs of the presence of stones, or the person ignores the existing symptoms without consulting a doctor.
Causes
Currently, there are several most likely causes of the formation of gallstones. It is expected that this could be:
- stagnation of bile of a mechanical or functional nature; with mechanical - the outflow of bile is obstructed due to obstacles (adhesions, kinks, tumors, etc.), with functional - disturbances arise due to impaired motility of the gallbladder.
- disturbance of bilirubin or lipid metabolism, which affects the circulation and synthesis of bile; cholesterol, bile pigments, salts are precipitated, the quantitative ratio of bile components is also disrupted, and solid formations appear.
The presence of unfavorable factors may be decisive in the development of the disease. The largest number of patients are in developed countries, with older people predominating; perhaps the reason lies in lack of exercise, poor diet, and stress. Also, the risk of this disease is higher in women. In addition, the likelihood of stone formation increases:
- obesity: in people with a body mass index of more than 35, cholelithiasis is diagnosed 20 times more often;
- dietary features: predominance in the diet of foods containing large amounts of cholesterol, abuse of low-calorie foods, sudden weight loss (more than 1.5 kg per week);
- various diseases: metabolic disorders, Crohn's disease, diverticula, infections, etc.;
- burdened heredity: among relatives there are already patients with the same diagnosis;
- long-term use of drugs that affect metabolic processes.
CHOLELITHIASIS
Gallstone disease (GSD) is a multifactorial and multistage disease characterized by impaired metabolism of cholesterol and/or bilirubin with the formation of stones in the gall bladder and/or bile ducts.
GSD is one of the most common human diseases. It ranks third after cardiovascular diseases and diabetes [8].
In developed countries, cholelithiasis is detected on average in 10–15% of the adult population. In Russia, among various populations of those examined, the prevalence of cholelithiasis ranges from 3–12%.
In women, cholelithiasis occurs 3-4 times more often than in men. The incidence among both men and women gradually increases with age, reaching a maximum at 60 years of age. Among children, the incidence of cholelithiasis is about 5%. Depending on the chemical composition, they are distinguished
There are 3 types of gallstones - cholesterol (cholesterol content 70% or higher), black pigmented and brown pigmented. Cholesterol and black pigment stones are formed mainly in the gallbladder, and brown ones - in the bile ducts. The prevalence of these types of stones varies greatly by country. In Europe and Russia, 80-90% of patients have cholesterol stones.
Etiology
GSD is a multifactorial disease. For the formation of gallstones and the progression of the disease, a necessary condition is the simultaneous existence and long-term action of 3 factors: supersaturation of bile with cholesterol, an imbalance between pronucleating and antinucleating factors, and a decrease in the evacuation function of the gallbladder.
Oversaturation of bile with cholesterol. This factor is caused by its excess production or deficiency of bile acids. Hereditary predisposition also matters. The risk of gallstone formation is 2–4 times higher in individuals whose relatives suffer from cholelithiasis. An important risk factor for the development of cholelithiasis is excess body weight. Obesity is accompanied by increased synthesis and excretion of cholesterol into bile. Eating foods high in cholesterol increases its level in bile. Low fiber foods slow down intestinal transit, which in turn promotes increased absorption of secondary bile acids, resulting in increased lithogenic properties of bile.
The use of oral contraceptives leads to increased lithogenic properties of bile. In women who use contraceptives, gallstones occur 2 times more often. Taking estrogen-containing drugs during menopause increases the risk of gallstone formation by 2.5 times. The lithogenic properties of bile are also affected by the intake of other drugs. Thus, clofibrate increases the excretion of cholesterol and increases the lithogenic properties of bile. Treatment with octreotide (Sandostatin) in patients with acromegaly leads to oversaturation of bile with cholesterol, decreased motor activity of the gallbladder and the formation of gallstones in 13–60% of patients [1, 2].
The course of a number of diseases is accompanied by cholelithiasis. With cirrhosis of the liver, gallstones are detected in 30% of patients. In PBC, bile duct stones (usually pigmented) occur in 39% of patients. It has been suggested that individuals with HbsAg have an increased risk of developing gallstones. Diseases of the small intestine with localization of the pathological process in the terminal section lead to disruption of the enterohepatic circulation of bile acids and, as a consequence, to dyscholia. Thus, in Crohn's disease with predominant localization in the terminal part of the small intestine, the frequency of stone formation reaches 26.4%. At the same time, there is no difference in the frequency of formation of gallstones between men and women, as well as the age dependence characteristic of cholelithiasis [14]. The degree of risk of stone formation is influenced by the location and extent of resection of the small intestine for various diseases. Subtotal and total hemicolectomy also increases the risk of gallstone formation. In severe malabsorption syndrome (celiac enteropathy, small intestinal resection, Crohn's disease, etc.), all main types of metabolism change, including the absorption of bile acids, which contributes to stone formation.
Factors contributing to the precipitation of cholesterol and the formation of a crystallization nucleus. The matrix for stone formation is bile proteins, cholesterol or bilirubin crystals. One of the most significant and identified pronucleators is mucin-glycoprotein gel. It should be noted that normally mucin is constantly secreted by the mucous membrane of the gallbladder, but its secretion increases in the presence of lithogenic bile. Proteins that accelerate the precipitation of cholesterol, in addition to mucin, include N-aminopeptidase, acidic α1-glycoprotein, immunoglobulins, phospholipase C; to antinucleators - aspirin and other NSAIDs. Apolipoproteins A1 and A2 slow down the deposition of cholesterol. In this case, weight loss is accompanied by an increase in the content of mucin and calcium in the gallbladder bile and thereby contributes to the formation of gallstones.
Factors leading to disruption of the basic functions of the gallbladder (contraction, absorption, secretion, etc.). In the gallbladder, bile is concentrated due to the absorption of Na+, Cl-, HCO- by the mucous membrane. At the same time, the wall of the gallbladder is virtually impermeable to bilirubin, cholesterol and bile acids, as a result of which bile thickens and the concentration of its main components increases by 5–10 times. When the contractile function of the gallbladder is preserved, its contents are constantly emptied, including from biliary sludge (BS), which can provoke the formation of gallstones. Stagnation of bile in the gallbladder, while its concentration function is preserved, significantly increases the risk of stone formation. Emptying the gallbladder is difficult due to flatulence, pregnancy, as well as a decrease in the sensitivity and number of receptors to cholecystokinin, motilin and other stimulants of motor activity, which is noted in chronic and xanthogranulomatous cholecystitis, cholesterosis of the gallbladder. With age, the sensitivity of the gallbladder receptor apparatus to various stimulants, including cholecystokinin, decreases.
Pathogenesis of the formation of cholesterol stones
Oversaturation of bile with cholesterol is the result of a violation of complex biochemical processes, the main of which is an increase in the activity of hydroxymethylglutaryl-coenzyme A reductase (HMG-CoA reductase), leading to an increase in cholesterol synthesis, or a decrease in the activity of cholesterol 7α-hydroxylase, leading to a decrease in the synthesis of bile acids These 2 enzymes are considered key in biliary lithogenesis. Cholesterol is insoluble in an aqueous environment and is excreted from the liver in the form of mixed micelles (in combination with bile acids and phospholipids), which are water-soluble. Mixed micelles are able to keep cholesterol in a stable state. When bile is oversaturated with cholesterol, all cholesterol cannot be transported in the form of mixed micelles. Its excess is transported in phospholipid vesicles, which are unstable and easily aggregate, and such bile is called lithogenic. In this case, large multilayer bubbles are formed, from which cholesterol monohydrate crystals are deposited [11], creating the basis for the formation of various variants of BS. In addition to cholesterol monohydrate crystals, BS may contain calcium salts - calcium bilirubinate, calcium carbonate and phosphate, mucin-glycoprotein gel and other components. If the conditions for cholelithiasis persist, gallstones form over time. The growth rate of stones is 3–5 mm per year, and in some cases more.
Classification of cholelithiasis
The widespread use of ultrasound research (ultrasound) has contributed to the detection of cholelithiasis at an early, pre-stone stage. However, these achievements of clinical gastroenterology, unfortunately, have not found practical application. One of the reasons is the lack of a clinical classification that would distinguish the initial stages of the disease.
The first, most significant attempt to identify the initial stages of the disease was made in the classification of cholelithiasis, proposed back in 1974 by DM Small, in which 3 out of 5 stages could be designated as pre-stone [5]. However, the classification, due to its complexity, was not used in the clinic and had more theoretical than practical significance.
A classification of cholelithiasis, more convenient for clinical use, was proposed by Kh. Kh. Mansurov in 1982 [4]. In the clinical period of cholelithiasis, in which the author identified 3 stages, its initial stage is designated by the author as physicochemical. However, to identify this stage, it is necessary to conduct a biochemical and microscopic examination of bile.
Other, noteworthy classifications of cholelithiasis reflected only the features of the clinical course of the disease [2, 3].
In 2002, the Congress of the Scientific Society of Gastroenterologists of Russia adopted a new classification of cholelithiasis, which distinguished 4 stages of the disease [5].
Stage I - initial, or pre-stone:
- thick heterogeneous bile;
- formation of biliary sludge: with the presence of microlites; with the presence of putty-like bile (PG); with a combination of putty-like bile with microliths.
Stage II - formation of gallstones:
- by localization: in the gallbladder; in the common bile duct; hepatic ducts;
- by the number of stones: single; multiple;
- composition: cholesterol; pigmented; mixed;
- according to the clinical course: latent course; with the presence of clinical symptoms - a painful form with typical biliary colic; dyspeptic form; under the guise of other diseases.
Stage III is the stage of chronic recurrent calculous cholecystitis.
Stage IV - stage of complication.
Detection of cholelithiasis at its initial stage - the formation of BS - provides ample opportunities for the primary prevention of cholelithiasis. Stage II allows you to more clearly determine the indications for various types of conservative therapy or surgical treatment. At stage III in the form of chronic recurrent calculous cholecystitis, the main method of treatment is surgery (in the absence of contraindications).
According to the proposed classification, the following diagnosis options can be formulated: cholelithiasis, biliary sludge (putty-like bile in the gallbladder), dysfunction of the gallbladder and sphincter of Oddi; cholelithiasis, cholecystolithiasis (single stone in the gallbladder), latent course; cholelithiasis, chronic recurrent calculous cholecystitis (multiple gall bladder stones) with attacks of biliary colic; cholelithiasis, chronic recurrent calculous cholecystitis (multiple gallbladder stones), disabled gallbladder, biliary pancreatitis.
Clinic
About 80% of patients with cholelithiasis do not complain. In some cases, the disease is accompanied by various dyspeptic disorders. The classic symptom of cholelithiasis is biliary colic. Attacks of biliary colic are usually associated with errors in diet and develop after heavy intake of fatty, fried or spicy foods.
The following characteristics of biliary colic are currently accepted [8]:
- severe pain lasting from 15 minutes to 5 hours;
- localization of pain in the epigastrium, right hypochondrium, sometimes radiating to the back, under the right shoulder blade;
- the patient needs bed rest and the use of medications;
- pain occurs most often in the evening or at night;
- pain recurs at various intervals.
The disease can be slow or characterized by a rapidly progressive course with various complications.
Diagnostics
To diagnose cholelithiasis, laboratory and instrumental research methods are used.
Laboratory parameters in uncomplicated cholelithiasis, as a rule, are not changed. After an attack of biliary colic, in 40% of cases an increase in the activity of serum transaminases is detected, in 23–25% - alkaline phosphatase, GGTP, in 45–50% an increase in the level of bilirubin. A week after the attack, the indicators usually return to normal. If the course of the disease is complicated by the development of acute cholecystitis, then leukocytosis and acceleration of ESR are noted.
Instrumental research methods play a leading role in the diagnosis of cholelithiasis. The main one is ultrasound, which makes it possible to detect the disease at the stage of formation of BS [7]. Transabdominal ultrasound scanning (TUS) detects gallstones in 90–98% and choledocholithiasis in 40–70% of cases. Using ultrasound, the size of stones, their number, location, mobility, and, to a certain extent, structure are determined. Ultrasound also allows us to judge the motor activity of the gallbladder. To do this, study the volume of the bladder on an empty stomach and after a choleretic breakfast. Ultrasonography makes it possible to assess the condition of the gallbladder wall, for example, to determine the presence or absence of an inflammatory process, cholesterol, or intrawall abscesses. In case of complicated cholelithiasis, ultrasound is used to assess the degree of destruction of the gallbladder wall and the condition of the circumvesical space.
The ultrasound criterion for diagnosing gallstones is a triad of signs: the presence of dense echo structures, an ultrasound shadow behind the stone (with soft cholesterol stones the shadow may be weak or absent), stone mobility.
X-ray methods have faded into the background, but have not lost their importance. The diagnostic value of oral cholegraphy in detecting cholelithiasis does not exceed 80-85%, and intravenous - 50-60%.
Computed tomography (CT) is used as an additional method to assess the condition of the tissues surrounding the gallbladder and bile ducts, as well as to detect calcification in gallstones when deciding on litholytic therapy.
Endoscopic retrograde cholangiopancreatography (ERCP) is the “gold” standard in the diagnosis of choledocholithiasis in many countries. However, this method plays a rather modest role in identifying cholecystolithiasis (CL). It is important to note that ERCP can be used not only for diagnostic purposes, but also for therapeutic purposes (papillosphincterotomy, extraction and crushing of stones, nasobiliary drainage for biliary hypertension, etc.). ERCP is indicated, first of all, in situations where there is a suspicion of choledocholithiasis, and other diagnostic methods, including TUS, do not allow it to be excluded.
The diagnostic value of ERCP in detecting choledocholithiasis is 79–98%. False-negative results are due to small-sized stones, as well as X-ray negative stones.
With ERCP, in some cases, complications develop, such as acute pancreatitis, acute cholecystitis, purulent cholangitis, suppuration of a pancreatic cyst, bleeding, injuries of the common bile duct, and penetration of a contrast agent into the retroduodenal tissue. ERCP in 15% of cases does not detect small (<3 mm) stones in the common bile duct, therefore, according to some authors, it cannot currently be considered the “gold” standard for diagnosing choledocholithiasis [15]. In this regard, endoscopic ultrasonography is becoming increasingly important in identifying stones in the bile ducts.
Endoscopic ultrasonography (EUS)
In obese patients with severe flatulence, TUS in most cases does not allow sufficiently good visualization of the gallbladder and especially the bile ducts and exclude cholecysto- or choledocholithiasis. At the same time, ERCP cannot always be performed due to technical difficulties in its implementation, organic changes in the sphincter of Oddi, surgical interventions in the gastroduodenal area, increased sensitivity to contrast agents, etc.
In these situations, EUS is indicated. Ultrasound scanning of the gallbladder and bile ducts is performed using an echoendoscope from the stomach or duodenum. Of the existing methods for detecting stones in the bile ducts, EUS is the most accurate [1].
Complications
Acute cholecystitis. Among the total number of patients with acute cholecystitis, the vast majority (up to 90%) are patients with cholelithiasis. The development of acute cholecystitis is promoted by mechanical damage to the mucous membrane from stones, as well as disruption of the outflow of bile (partial or complete obstruction of the cystic duct with mucus, small stones, putty-like bile).
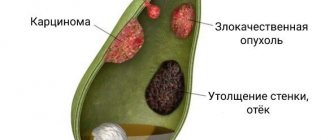
Chronic cholecystitis can occur as an outcome of acute cholecystitis or develop gradually, in the form of a primary chronic form. Laboratory parameters are usually within normal limits. On ultrasound, the gallbladder is deformed, reduced in size, the walls are compacted and unevenly thickened. In the lumen of the bladder there are clots of heterogeneous bile with an admixture of bile.
Hydrocele of the gallbladder develops when the cystic duct is obstructed by a stone or a clot of the gallbladder and is accompanied by the accumulation of transparent contents mixed with mucus in the cavity of the bladder. Diagnosis is made using ultrasound, sometimes supplemented by CT. The addition of infection threatens the development of empyema of the gallbladder.
Empyema of the gallbladder develops against the background of a disabled gallbladder as a result of infection. Clinical symptoms correspond to the picture of an intra-abdominal abscess. On palpation of the abdomen, the gallbladder is enlarged, tense, sharply painful, positive symptoms of peritoneal irritation. Treatment is surgical, in combination with antibiotic therapy.
Cellulitis of the gallbladder wall and an abscess in the area of the gallbladder bed can be the result of acute cholecystitis, formed as a result of a bedsore from a large stone with the subsequent addition of an inflammatory process. Diagnosis is based on clinical data, laboratory and instrumental studies (ultrasound, CT). Often accompanied by the formation of various fistulas. Treatment is surgical, in combination with antibiotic therapy.
Perforation of the gallbladder occurs when there is transmural necrosis of the gallbladder wall. It most often occurs as a result of a bedsore that develops from the pressure of a large stone on the wall of the gallbladder. Less commonly, as a result of rupture of the Rakitansky-Aschoff sinuses. A breakthrough of the contents of the gallbladder into the free abdominal cavity is observed relatively rarely, since the adhesive process around the bladder and the surrounding organs limit its spread. A breakthrough into the hollow organs adjacent to the bladder leads to the formation of internal fistulas. With CT and ultrasound, in addition to gallstones, it is possible to additionally identify abscesses and effusion in the abdominal cavity. The prognosis is poor, with a mortality rate of approximately 30%.
Biliary pancreatitis. Both mild forms of pancreatitis and severe ones, up to pancreatic necrosis, can develop. Treatment primarily consists of eliminating the cause of biliary pancreatitis.
Mirizzi syndrome. Wedging of a stone into the neck of the gallbladder with the subsequent development of the inflammatory process can lead to compression of the common bile duct (Mirizzi syndrome type I). Subsequently, a cholecystocholedochal fistula (Mirizzi syndrome type II) may form. Currently, there are 4 types of this syndrome [12]. Treatment is surgical.
Biliary fistulas. With necrosis of the bladder wall, internal bile fistulas are formed. Diagnosing them is difficult, since the clinical picture is masked by the symptoms of the underlying disease. Most internal fistulas are discovered incidentally during cholangiography or surgery.
Intestinal obstruction caused by gallstones is rare, usually occurs in patients over 70 years of age, and is associated with high mortality. Occurs after perforation of the gallbladder and entry into the intestine of a gallstone of at least 2.5 cm in diameter. Intestinal obstruction occurs in the most narrowed areas of the intestine, usually 30–50 cm proximal to the ileocecal valve. Treatment is surgical.
Gallbladder cancer. Gallstones and a wrinkled gallbladder, as a rule, do not lead to the development of gallbladder cancer; the incidence of its occurrence in patients with cholelithiasis usually does not exceed 3–5%. However, 90% of cases of gallbladder cancer are accompanied by cholecystolithiasis.
Treatment
Conservative methods. Conservative therapy is indicated at the pre-stone stage of the disease; in some patients it can be used at the stage of formed gallstones.
Treatment at the pre-stone stage. The appearance of clinical symptoms in BS, the development of complications and the formation of gallstones in some patients are the basis for adequate therapy and dynamic monitoring of such patients.
Depending on the form of BS and the state of the contractile function of the gallbladder, bile acid preparations or hepabene are used.
Ursodeoxycholic acid (UDCA) drugs for BS are prescribed in a standard daily dose of 10 mg/kg body weight once, at night. The course of treatment depends on the form of BS. For BS in the form of a suspension of hyperechoic particles (HHP), a month's course of treatment is usually sufficient. With other forms, the course of treatment is longer, but, as a rule, does not exceed 3 months.
In patients with a low cholate-cholesterol ratio, it is advisable to add chenodeoxycholic acid (CDCA) preparations to UDCA treatment, replacing 1/3 of the daily dose with them. This is due to the different mechanisms of action of bile acids, so their combined use is more effective than monotherapy with each drug separately. According to our data, after a 3-month course of ursotherapy in patients with BS in the form of HHV, the effectiveness was 60%; clots of echoheterogeneous bile (HBC) - 85.7%; putty-like bile - 87.5%.
Gepabene is prescribed 1 capsule 3 times a day; for severe pain, add 1 capsule at night. The course of treatment is 1–3 months. The drug contains extract of fumaria officinalis, which has a choleretic and antispasmodic effect, and milk thistle fruit extract, which improves hepatocyte function.
According to our data, the effectiveness of hepabene for BS in the form of HHV was maximum and amounted to 100%; with BS in the form of SEF - 70%; in patients with BS in the form of gastrointestinal tract, therapy did not have a noticeable effect.
Treatment at the stage of formed gallstones. According to our information, about 30% of patients with cholecystolithiasis can be subjected to litholytic therapy (LT). For treatment, CDCA and/or UDCA drugs are used.
RT is prescribed in cases where patients are contraindicated for other types of treatment, as well as in the absence of the patient’s consent to surgery.
The effectiveness of RT depends on the correct selection of patients. Successful treatment is more often with early detection of cholelithiasis and much less often with a long history of the disease due to calcification of stones. Single stones dissolve worse than multiple ones (the latter have a more optimal ratio of the surface of the stones to the volume of the gallbladder). If the contractile function of the gallbladder is preserved, the prognosis for the success of therapy is much more optimistic.
The patient selection criteria are based on ultrasound and oral cholecystography data. One of the main conditions determining the effectiveness of RT is determining the composition of gallstones. Stones with a high cholesterol content dissolve best. According to ultrasound, these are stones with a homogeneous and low-echoic structure, a soft acoustic shadow behind (or without); according to cholecystography - “floating” stones. To clarify the composition of stones, it is advisable to conduct a CT scan. Stones with an attenuation coefficient below 70–100 Hounsfield units are more likely to dissolve [8, 11]. A prerequisite for RT is the absence of obstruction of the bile ducts.
Numerous studies have shown that large stones require long-term (at least 2 years) therapy with a fairly low effectiveness. Currently, it is not recommended to carry out treatment for stone diameters greater than 10 mm.
Contraindications to RT are pigment stones, cholesterol stones with a high content of calcium salts, stones more than 10 mm in diameter, stones whose total volume is more than 1/4-1/3 of the volume of the gallbladder, as well as reduced contractile function of the gallbladder (ejection fraction < thirty%). RT is not indicated for patients with frequent colic. However, in a number of cases, according to our data, during therapy their frequency noticeably decreased or they disappeared altogether.
Severe obesity is considered a relative contraindication. For successful therapy, such patients need to increase the daily dose of bile acids. Ursotherapy is not a contraindication for the treatment of cholelithiasis in pregnant women.
The results of RT depend on the careful selection of patients, the duration of therapy and vary widely: from 0 [4] to 80–90% [11] and even 100% [6].
Stone recurrence after successful oral radiotherapy is approximately 10% per year for 5 years, most often in the first 2 years, then its frequency decreases. To prevent recurrence of stones, it is necessary to continue therapy for another 3 months. It is advisable to reduce body weight, avoid taking drugs that increase cholesterol synthesis, and long periods of fasting.
Extracorporeal shock wave lithotripsy (ESWL)
The method is based on the generation of a shock wave. Within 30 ns, a pressure 1000 times higher than atmospheric pressure is reached at the focus. Due to the fact that soft tissues absorb little energy, most of it falls on the stone, resulting in its destruction. The method is currently used as a preparatory step for subsequent oral litholytic therapy.
Indications for ESWL:
- single cholesterol stones with a diameter of no more than 3 cm;
- multiple stones (no more than 3) with a diameter of 1–1.5 cm;
- functioning gallbladder;
- no obstruction of the bile ducts.
Contraindications to ESWL:
- presence of coagulopathy or anticoagulant therapy;
- the presence of cavity formation along the shock wave.
We found that approximately 20% of patients with cholelithiasis meet the criteria necessary to undergo ESWL.
With proper selection of patients for ESWL, stone fragmentation can be achieved in 90–95% of cases. Lithotripsy is considered successful if it is possible to achieve fragmentation of stones with a diameter of less than 5 mm. After ESWL, bile acid preparations are prescribed in the same doses as for oral RT. Side effects with ESWL are relatively rare. The most significant are biliary colic, in some cases mild signs of cholecystitis, hyperaminotransferasemia.
Stone recurrence is less after ESWL than after oral RT. This circumstance is due to the fact that patients with ESWL are selected mainly with single stones, in whom relapses are observed less frequently, compared to patients with multiple stones.
Contact dissolution of gallstones
In contact litholysis, a solvent is injected directly into the gallbladder or bile ducts. The method is an alternative for patients with high surgical risk and has become increasingly widespread abroad in recent years. In Russia, there are isolated reports of successful dissolution of gallstones using contact litholysis [9, 10]. Only cholesterol stones are dissolved, and the size and number of stones are not of fundamental importance. Methyl tert-butyl (ether) (MTBE) is used to dissolve stones in the gall bladder, and propionate (ether) in the bile ducts [16]. Dissolution occurs in 4–16 hours.
A multicenter study conducted in 21 medical centers in Europe, which involved 803 patients, showed the high effectiveness of contact litholysis [13]. The puncture was successful in 761 patients (94.8%), and the stones were dissolved in 95.1% of cases. In 43.1% of patients, after lysis of stones, stones remained in the bladder. The method can be successfully used to dissolve fragments remaining after ESWL.
Surgery
Surgical treatment for cholecystolithiasis consists of removing the gallbladder along with stones or only stones from the bladder. In this regard, the following types of operations are distinguished:
- traditional (standard, open) cholecystectomy from the upper middle or right oblique laparotomy access;
- laparoscopic (videolaparoscopic) cholecystectomy;
- cholecystolithotomy.
Options for surgical interventions for cholelithiasis are described in sufficient detail in the specialized literature. Based on our own experience, we offer a list of the following main indications for surgical treatment:
- HL with the presence of large and small gallbladder stones, occupying more than 1/3 of the gallbladder volume;
- HL, regardless of the size of the stones, occurs with frequent attacks of biliary colic;
- CL, disabled gallbladder;
- HL complicated by cholecystitis and/or cholangitis;
- HL in combination with choledocholithiasis;
- HL complicated by the development of Mirizzi syndrome;
- HL complicated by dropsy, empyema of the gallbladder;
- HL complicated by penetration, perforation, fistulas;
- HL, accompanied by a decrease in the contractile function of the gallbladder (ejection fraction after a choleretic breakfast less than 30%);
- HL complicated by biliary pancreatitis;
- HL in combination with obstruction of the common bile duct.
For questions regarding literature, please contact the editor.
A. A. Ilchenko, Doctor of Medical Sciences, Research Institute of Gastroenterology, Moscow
Symptoms
Manifestations depend on the location and size of gallstones; symptoms characteristic of this pathology:
- The pain is dull, constant, localized on the right hypochondrium, and can radiate to the shoulder, arm, neck, shoulder blade, and lower back. In some cases, the pain radiates beyond the sternum, resembling the pain of angina pectoris. Pain can occur after errors in diet or excessive exercise. But its intensity is not an indicator of the severity of the disease; some patients experience only mild pain and the presence of several stones of impressive size.
- Biliary colic, in which intense pain forces the patient to unsuccessfully search for a position that can relieve suffering. As the disease progresses, pain occurs more often, its intensity and duration increase.
- Temperature - periodic increases to 37-38°C, accompanied by pain; also during an attack, an increase to 38-40°C is possible, and the patient often experiences chills.
- Yellowness of the skin is characteristic of obstruction of the sphincter of Oddi or obstruction of the ducts.
Signs such as nausea, vomiting, and bloating, although they may occur in the presence of stones, are not specific; these symptoms often appear with other diseases of the digestive system.
Possible complications
Among the common ones are the development of the inflammatory process and obstruction (block) of the biliary tract, which can lead to obstructive jaundice and acute pancreatitis. Also, in the absence of timely treatment, the appearance of fistulas, bladder rupture, the development of peritonitis and other complications dangerous to humans is possible.
To identify cholelithiasis, determine the degree of inflammation in the wall of the gallbladder, as well as select the correct individual tactics of surgical treatment, you must send me a complete description of an ultrasound of the abdominal organs, preferably a gastroscopy, to my personal email address, you must indicate your age and main complaints. In rare cases, if stones in the ducts are suspected, it is necessary to perform an endoscopic ultrasound examination of the ducts and pancreas. Then I will be able to give a more accurate answer to your situation.
Treatment
The goal of treatment for gallstones is to relieve the condition and prevent complications. With the help of conservative treatment, you can only reduce the clinical manifestations; we are talking about taking drugs that improve the motility of the gallbladder, the outflow of bile, and anti-inflammatory therapy. It is important to prevent attacks by following a diet, combating inactivity and excess weight.
However, gallstones can only be removed through surgery. Indications for intervention are:
- recurrent attacks;
- development of the inflammatory process;
- constant pain;
- the presence of pathological changes in neighboring organs (pancreatitis, duodenitis, hepatitis);
- the appearance of complications.
Selection of methodology
The doctor chooses the method of crushing formations individually. In the first surgical department of the hospital, it is possible to carry out both modern methods of treating this pathological process. The doctor prescribes ultrasound destruction only in the presence of insoluble stones of a certain chemical structure that are sensitive to the effects of ultrasound. Laser crushing of stones is effective regardless of their chemical structure. The choice of technique, in addition to the chemical structure of the formations, is also determined by the general condition of the patient and the presence of possible contraindications to each specific treatment method.
Operation
Today there are two methods of surgical treatment, but in any case, during the operation the gallbladder is removed, since while methods for removing stones without removing the organ itself are not effective, after 6 months they form again
- Open cholecystectomy is an operation during which the stones along with the gallbladder are removed through one 15-20 cm incision in the abdominal wall. This technique is recommended only for complicated processes.
- Laparoscopic cholecystectomy is a low-traumatic operation for gallstones, performed through small punctures in the peritoneal wall, the size of which is no more than 10 mm. This technique is recognized as the “gold” standard in the treatment of gallstone disease. There are several types of laparoscopy; surgery for gallstones can be performed transvaginally (NOTES technology), through a single puncture in the paraumbilical area (single-port SILS technology), and mini-laparoscopy is also performed in our clinic using miniature instruments.
Prevalence of cholelithiasis
According to static data, 25% of the world's population suffers from signs of gallstone disease: in Russia, the disease is diagnosed in 15% of the adult population.
Stones can form at any age, but more often after 30-35 years. Unfortunately, recently the disease has become “younger” and young patients are faced with the symptoms of gallstone disease. Women are at risk: they are diagnosed 3-4 times more often. But after 60-70 years, this difference disappears, and the frequency of cases becomes approximately the same. Historical reference
This disease has been known since ancient times. The first mentions date back to the Renaissance; scientific treatises described attacks of pain in the right side and other symptoms characteristic of the disease. For the first time, cholelithiasis was described by a German doctor who established a connection with jaundice and a disorder of bilirubin metabolism. The first operation to remove the gallbladder was performed in 1735. In Russia, the first such operation was performed in 1890 by N.V. Sklifosofsky. The first laparoscopic operation was performed in France in 1987, and later the technique became widespread and recognized throughout the world. In Russia, the first such operation was carried out only in 1991. Now this technique has been put into production and is widely used in our country.
Forecast
With stones in the gall bladder, there are no obvious clinical manifestations at first. But sooner or later a person is forced to see a doctor. Repeated attacks indicate the need for surgery, otherwise there is a high risk of complications. With a timely cholecystectomy, a complete cure is possible, and in the future the person, subject to simple recommendations, can lead a life without any special restrictions.
Every patient who contacts me can count on complete and high-quality treatment. I always strive to perform a low-traumatic operation. But to choose the optimal treatment tactics, an examination is necessary; in our clinic, all effective diagnostic methods are available to patients. We have developed a special program, registered in the Russian Federation, which allows us to improve diagnostics and select the most appropriate treatment method, avoiding unnecessary trauma and the risk of intraoperative complications.
Having personally performed more than 6,000 laparoscopic cholecystectomies, the experience gained over more than 30 years of work allows me to find the solution that is most suitable for the patient, taking into account his medical condition. The results of the operations performed are summarized in 30 scientific papers published in academic Russian and foreign publications. I described in detail the indications and technique of all types of operations for cholelithiasis in a monograph published in 2022 - SURGERY FOR GALLSTONIS: laparoscopy, minilaparoscopy, single port, transvaginal access, simultaneous operations. -M.: Publishing House "MEDPRACTIKA-M", 2022, 312 p.
I also regularly conduct seminars where issues of treatment of the abdominal organs, including cholelithiasis, are discussed. They are attended by both postgraduate cadets and leading specialists from large scientific centers.