- What types of cancer can occur in the head of the pancreas?
- Stages of pancreatic head cancer
- Risk factors
- Symptoms of pancreatic head cancer
- Diagnostic methods. Screening
- Treatment of pancreatic head cancer
- Prognosis and survival
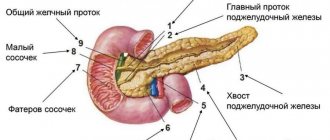
The pancreas is approximately 15 cm long and anatomically consists of three parts: head, body and tail. The head is located in the upper right part of the abdomen, at the level of the first two lumbar vertebrae. It is covered by the duodenum.
The main function of the pancreas is to produce digestive enzymes. The duct of the gland emerges from its head, then connects with duct - the main bile duct - and together they flow into the duodenum.
In addition, the pancreas contains endocrine cells that produce hormones. The most famous of them is insulin.
What types of cancer can occur in the head of the pancreas?
In 60–70% of cases, pancreatic cancer occurs in the head of the pancreas. More than 80% of tumors are adenocarcinomas . They develop from cells that line the ducts of the gland.
Less common are cystic tumors . In most cases, pancreatic cysts are benign, but in some cases they contain cancer cells. A biopsy helps establish an accurate diagnosis.
If the tumor originates from cells that produce the enzyme, it is called acinar cell carcinoma . It is usually diagnosed at a younger age, grows slowly and has a better prognosis.
Tumors of endocrine cells are rare: insulinomas, glucagonomas, gastrinomas, somatostatinomas.
Etiology
Pancreatic cancer is more common among urban residents who consume large amounts of meat and fat. Smoking contributes to carcinogenesis in general and prostate cancer in particular (pancreatic cancer is registered 2-2.5 times more often in smokers than in non-smokers). It is assumed that carcinogens contained in tobacco can, under certain conditions, enter the pancreatic duct with bile, first provoking inflammation and then the formation of a tumor. Drinking large amounts of coffee (more than 3 cups per day) increases the risk of the disease, but the true cause-and-effect relationship remains unclear.
Stages of pancreatic head cancer
At stage I, the tumor measures no more than 4 cm and is located within the organ and does not spread to adjacent structures and lymph nodes. There are substages IA (tumor less than 2 cm) and IB (tumor 2–4 cm).
At stage II, the tumor is more than 4 cm in diameter (substage IIA), or it has any size, but spreads to neighboring organs (bile duct, duodenum), lymph nodes (substage IIB). In this case, the process does not affect large blood vessels.
If the tumor affects a larger number of lymph nodes, grows into neighboring organs and large blood vessels, but there are no distant metastases, stage III cancer of the head of the pancreas is diagnosed.
At stage IV there are distant metastases.
Kinds
Congenital (dysontogenetic) pancreatic cysts are formed as a result of malformations of the tissue of the organ and its ductal system. Acquired pancreatic cysts are as follows:
- Retention - develop as a result of narrowing of the excretory ducts of the gland, persistent blockage of their lumen by neoplasms and stones;
- Degenerative – formed as a result of damage to gland tissue during pancreatic necrosis, tumor process, hemorrhage;
- Proliferative – cavitary neoplasms, which include cystadenomas and cystadenocarcinomas;
- Parasitic - echinococcal, cysticercosis.
Depending on the cause of the disease, pancreatic cysts of an alcoholic nature and those developing as a result of cholelithiasis are distinguished. With the increasing number of terrorist acts, road traffic accidents, natural and man-made disasters, the formation of false pancreatic cysts in severe abdominal injuries is becoming important. Depending on the location of the cystic formation, a cyst of the head, body or tail of the pancreas is distinguished.
True cysts make up 20% of cystic formations of the pancreas. True cysts include:
- Congenital dysontogenetic cysts of the gland;
- Acquired retention cysts;
- Cystadenomas and cystadenocarcinomas.
A distinctive feature of a true cyst is the presence of an epithelial lining on its inner surface. True cysts, unlike false formations, usually do not reach large sizes and are often accidental findings during surgery.
A false cyst is observed in 80% of all pancreatic cysts. It forms after trauma to the pancreas or acute destructive pancreatitis, which was accompanied by focal tissue necrosis, destruction of the walls of the ducts, hemorrhages and release of pancreatic juice outside the gland. The walls of the false cyst are compacted peritoneum and fibrous tissue; from the inside they do not have an epithelial lining, but are represented by granulation tissue. The cavity of a false cyst is usually filled with necrotic tissue and fluid. Its contents are serous or purulent exudate, which contains a large admixture of clots of altered blood and spilled pancreatic juice. A false cyst can be located in the head, body and tail of the pancreas and reach large sizes. It contains 1-2 liters of content.
Among cystic formations of the pancreas, surgeons distinguish the following main types, which differ in the mechanisms and causes of formation, features of the clinical picture and morphology required in the application of surgical tactics:
- Extrapancreatic false cysts occur due to pancreatic necrosis or trauma to the pancreas. They can occupy the entire omental bursa, the left and right hypochondrium, and are sometimes located in other parts of the chest and abdominal cavities, the retroperitoneal space;
- Intrapancreatic false cysts are usually a complication of recurrent focal pancreatic necrosis. They are smaller in size, often located in the head of the pancreas and often communicate with its ductal system;
- Cystic dilatation of the pancreatic ducts as their dropsy is most often found in alcoholic calculous pancreatitis;
- Retention cysts most often originate from the distal parts of the pancreas, have thin walls and are not fused with the surrounding tissues;
- Multiple thin-walled cysts unchanged in the remaining parts of the pancreas.
Make an appointment
Risk factors
A normal cell becomes cancerous when certain mutations occur in it. It is often impossible to say exactly what caused the changes in DNA, so the causes of cancer of the head of the pancreas are unknown. Scientists only know about risk factors - various external influences and conditions of the body that increase the likelihood of disease:
- Bad habits: smoking (increases the risk by about 20%), alcohol.
- Low physical activity and excess body weight.
- A diet high in red and processed meats, low in fruits and vegetables.
- Family history (close relatives who have been diagnosed with cancer of the head of the pancreas), certain genetic defects and hereditary syndromes.
- Chronic pancreatitis.
- Stomach diseases: Helicobacter pylori infection, peptic ulcer.
- Viral hepatitis.
- There is evidence that the risks are increased by diseases of the teeth and gums.
Causes
The causes of the development of diseases in this group are very diverse. Among the main ones are the following:
- Smoking.
- Alcohol abuse.
- Metabolic diseases (obesity, type 2 diabetes).
- Poor nutrition (consumption of fast food, fatty and fried foods, lack of plant fiber in the diet).
- History of chronic inflammatory diseases of the pancreas (pancreatitis).
- Living in an unfavorable environmental environment, in conditions of high levels of asbestos, cadmium, benzene, petroleum products, soot, phenolic resins in the atmosphere; harmful working conditions (heavy dust, high temperature).
Symptoms of pancreatic head cancer
In the early stages, the tumor usually does not manifest itself. Then some symptoms appear, but they are non-specific, most often they indicate some other disease.
The most characteristic manifestation of pancreatic head cancer is jaundice. It is often the first symptom with which a patient consults a doctor. Next to the head of the gland is the bile duct. As the tumor grows, it compresses it, disrupting the flow of bile. As a result, the toxic breakdown product of hemoglobin - bilirubin - is not excreted into the intestines, but enters the blood. This leads to the skin and whites of the eyes becoming yellowish and causing itching.
Since bilirubin in bile is not excreted into the intestines, the stool becomes light-colored. Urine, on the contrary, darkens.
Other possible symptoms: abdominal pain, nausea and vomiting, weight loss, indigestion, deep vein thrombosis of the leg, fever. In rare cases, the tumor destroys the endocrine cells that produce insulin. Blood sugar levels rise and diabetes develops.
MRI of the pancreas, how to prepare?
Ask your doctor if you have any questions about MRI scans.
Magnetic resonance imaging is often performed routinely; in urgent situations with an acute abdomen, it is preferable to do a CT scan. Preparation for an MRI of the pancreas implies:
- Obtaining a referral for research. The document must indicate the intended diagnosis, area/s of interest, type - with or without contrast;
- Dieting. A few days before the procedure, products containing starch, yeast, sugar - baked goods, confectionery - are excluded from the diet. Excessive flatulence and fermentation processes in the intestines are caused by fresh vegetables (cabbage, peas, beans), fruits, herbs, mushrooms, milk, brown bread, etc. Alcohol, kvass and drinks with gas can cause the movement of small stones and accompanying inflammation, which will provoke swelling of the gland and gallstone colic. You should avoid fatty meats, fish, smoked meats, marinades, and spices. A 6-hour fast is required before the test. The paramagnetic gadolinium and prolonged lying on the back can cause autonomic reactions in the form of dizziness, nausea, and drooling. You can prevent such phenomena by having a light snack 30 minutes before leaving the house.
- Taking medications. Medicines for routine therapy are taken as usual. Antispasmodics, enzymes, adsorbents, laxatives are used exclusively on the recommendation of a doctor. An enema is needed for chronic constipation (if it is planned to examine all organs of the gastrointestinal tract).
Don’t forget to take with you the results of ultrasound, FGDS, images and descriptions of previously performed MRI/CT, epicrisis from the hospital, conclusion of the oncoconsilium. If the study is paid for by an insurance company, a compulsory medical insurance or voluntary health insurance policy will be required.
Diagnostic methods. Screening
Usually, if symptoms appear, this indicates that the tumor has already grown beyond the pancreas. It is often at this stage that the patient is diagnosed. Currently, there are no recommended screening tests that would help diagnose the disease in its early asymptomatic stages.
Usually, first of all, the doctor prescribes an ultrasound of the abdominal organs to the patient, as the fastest, most accessible, safe and non-invasive diagnostic method. More informative studies are CT and MRI, they help to identify a pancreatic tumor and find out whether the cancer has spread to neighboring organs and regional lymph nodes.
Cholangiopancreatography is used to assess the condition of the bile ducts. To do this, a radiopaque substance is injected into the ducts endoscopically, through the duodenum, or with a needle through the skin, after which radiographs are taken.
PET scanning helps detect metastases. During the procedure, a safe radioactive substance is injected into the body, which accumulates in cancer cells and makes them visible in special photographs.
The most accurate method for diagnosing pancreatic head cancer is a biopsy. Tumor tissue for cytological and histological examination can be obtained in different ways:
- Using a needle through the skin, under CT or ultrasound guidance.
- During laparoscopy.
- During endoscopic ultrasound: a test in which an ultrasound probe is placed at the end of an endoscope inserted into the duodenum.
- During cholangiopancreatography.
Is MRI performed for diseases of the pancreas?
The reason to sign up for a magnetic resonance examination of the abdominal cavity and retroperitoneal space is the detection in laboratory parameters of changes characteristic of damage to the organs of the biliary system
MRI for diseases of the pancreas is done to identify pathology, determine the stage of the disease and detect complications. The images provide the doctor with valuable information for making a diagnosis. The doctor analyzes:
- location, size and internal structure of the gland;
- zonation of the organ - features of visualization of the body, head and tail;
- involvement of parapancreatic tissue in the pathological process, spread of the tumor to nearby tissues, connection of the neoplasm with the pancreas, damage to the lymph nodes;
- configuration, tumor density, blood supply characteristics, presence of areas of necrosis, calcification (allows to differentiate benign and malignant processes);
- consistency of anastomoses after liver transplantation;
- changes in the parenchyma, the severity of inflammation;
- parasitic lesions;
- developmental anomalies;
- modification of the ducts of the pancreatic and biliary tract as a whole, the presence of strictures, localization, stone formation;
- changes in the retroperitoneal space etc.
Taking into account the absence of long-term consequences after the diagnostic procedure, the study is suitable for dynamic monitoring of cystic neoplasms and monitoring the effectiveness of therapy.
Treatment of pancreatic head cancer
The main treatment method for pancreatic head cancer is surgery. In some cases, the surgeon may remove only the head of the pancreas, along with part of the small intestine and/or stomach, gallbladder, and common bile duct. Then the body and tail of the gland are sutured to the small intestine, after which they can continue to perform their functions.
In some cases, the entire gland has to be removed. After such an operation, you will have to take enzymes and administer insulin for the rest of your life.
Pancreatic cancer responds to chemotherapy and radiation therapy. They are prescribed as adjuvant (to prevent relapse after surgery) or neoadjuvant (to reduce tumor size before surgery, convert inoperable cancer to operable) treatment. If the tumor is inoperable, radiation therapy and chemotherapy become the main treatments.
erlotinib ( Tarceva may be used in some patients . It blocks EGFR, a receptor protein that causes cancer cells to multiply.
For inoperable cancer of the head of the pancreas, palliative surgery helps relieve symptoms and improve the patient’s condition:
- If the outflow of bile is impaired, the bile duct is stented or cut off above the block and connected to the duodenum (this operation is called choledochojejunostomy ).
- If the patency of the duodenum is impaired, a stent can also be installed. If this is not possible, a jejunostomy - the jejunum is sutured to the skin and an opening is brought out ( jejunostomy ). Through it, the patient receives nutrition using a catheter.
What can you eat before an MRI of the pancreas?
It is preferable to prepare dishes using gentle heat treatment - boiling, baking, stewing
To ensure that food is fully digested, the following are allowed on the eve of the procedure:
- lean meat, dietary fish, skinned chicken breast;
- baked vegetables and fruits;
- porridge with water;
- omelettes;
- unrich broths;
- crackers, dry cookies;
- vegetable oil in small quantities;
- unsweetened compotes, still water, herbal teas, diluted juices without pulp.
Normal size of the pancreas on MRI
Organ parameters are variable:
| Department | Dimensions (mm) |
| Head | 11- 35 |
| Body | 4- 30 |
| Tail | 7- 30 |
The concept of normal on magnetic resonance images is relative. Sizes depend on gender, height, age, food load. A slight deviation from generally accepted indicators, provided the structure of the organ parenchyma is normal and functions are intact, is not considered a pathology. The length of the pancreas is 15-23 cm, width 4.5-6 cm, weight about 70-80 grams.
Normally, the organ is not enlarged, the contours are clear, even, and the dimensions correspond to the person’s build. The pancreatic duct is not dilated, the surrounding tissue is without any features. No changes in the MR signal were detected.
CT and MRI in the diagnosis of pancreatic cancer
HOW TO DIAGNOSE PANCREAS CANCER
The pancreas is a very important organ that produces pancreatic juice necessary for digestion, and also takes part in the production of hormones, including insulin. Tumor diseases of the gland are common. Their peculiarities include the fact that there are no early symptoms of pancreatic cancer as such. At an early stage, neoplasms of the pancreatoduodenal zone do not manifest any symptoms, which is why they are diagnosed late. Thus, the patient may not be aware of cancer for a long time. Symptoms appear only when the tumor grows into neighboring organs, when its size increases (for example, when it compresses the papilla of Vater, into which the bile ducts open). With this variant of the course of the disease, obstructive jaundice appears. This forces the patient to undergo diagnostic testing (CT, MRI, ultrasound), which reveals the oncological process. In other cases, the tumor may be an incidental finding during studies performed for some other reason. More often, a tumor is discovered by chance during a preventive ultrasound.
HOW TO TEST YOUR PANCREAS FOR CANCER
Today, there are several methods for accurately diagnosing this oncology, both X-ray and non-X-ray. In this article we will take a detailed look at what pancreatic cancer looks like on various images and how to find it using each of these methods. We will also provide diagnostic signs of pancreatic cancer, as well as consider clinical examples illustrating this dangerous disease.
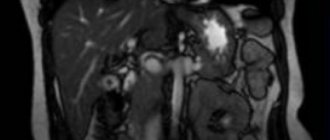
Today, scientists have proven that the most informative way to check the pancreas for cancer and to identify oncopathology as early as possible is magnetic resonance imaging (MRI). This study makes it possible to clearly visualize the tumor, determine its structure and structure, distinguish between the soft tissue and cystic components, identify growth into the parapancreatic tissue (that is, the tissue surrounding the gland, from the Latin word “pancreas”), into neighboring organs (into the spleen, into the renal fascia , into the duodenum, into other parts of the intestine, into the omentum). In this case, it is necessary to take into account the fact that MRI must be performed on a high-field device (with a field strength of not <1.5 Tesla), because only such a device provides the required quality of diagnostic images. If necessary, the study is supplemented with the introduction of a contrast agent. In addition, it should be borne in mind that image analysis should be carried out by an experienced radiologist with good experience in diagnosing pathology of the pancreaticoduodenal zone. To avoid a diagnostic error, you can re-analyze the MRI images and get a Second Opinion from an experienced specialist (more on this at the bottom of the article).
Get an MRI of the pancreas in St. Petersburg
Also, a formation in the pancreas can be detected by ultrasound. This is a simple and accessible method that evaluates changes in the structure of the organ, changes in size (thickening), the presence of a cystic (liquid) component, the degree of expansion of the pancreatic duct, and signs of cancer germination (invasion) into neighboring tissues. The disadvantage of ultrasound is its low tissue resolution, and in doubtful cases, tomographic methods are prescribed - computed tomography and MRI.
A space-occupying pancreas formation can also be suspected during FGDS (fibrogastroduodenoscopy), a study of the organs of the digestive system using a flexible fiber-optic probe. In this case, the endoscopist may note a deformation (persistent, permanent) of the duodenum and suspect some kind of volumetric process in the pancreaticoduodenal zone. If there is such a suspicion, a computer or magnetic resonance imaging scan is required.
CT DIAGNOSIS OF PANCREAS CANCER
The most widely used X-ray method for visualizing pancreatic volumetric processes is computed tomography. The study can be either native (without contrast) or with contrast. Contrast CT helps to better differentiate normal and tumor tissue, as well as clearly identify the pathology of the vessels surrounding the gland. In addition, contrast enhancement on CT scans is mandatory if the doctor wants to exclude the spread of the process to the liver (liver metastases) or surrounding lymph nodes.
SIGNS OF A NEOPOLOGY (CANCER) OF THE PANCREAS DETECTED BY CT
1) Local thickening (tail, body and head are thickened evenly). Thickening can also be diffuse (affecting all departments) - in this case it is customary to talk about “pseudotumorous pancreatitis” and not about cancer. Sometimes it is difficult to distinguish between these two conditions on CT or MRI, and consultation with an experienced radiologist is necessary. With local thickening, the size of the affected area is usually measured on axial sections and assessed according to the TNM system (T - lat., "tumor" - tumor, N - "nodus" - lymph node, M - "metastasis" - the presence of metastases in distant organs, more often total liver).
On the images: local thickening of the pancreas head due to a soft-tissue (solid) neoplasm that practically does not accumulate contrast (red arrow). The dilated duct of Wirsung is highlighted with a yellow arrow.
The tail of the pancreas is sharply thickened (yellow arrow), its structure is disturbed: multiple poorly contrasted areas (necrosis and decay) are visible. In addition, there is ascites (fluid in the abdominal cavity). Metastasis to the perinephric tissue (retroperitoneal) is highlighted with a red asterisk.
The same patient. When analyzing the remaining scans, it becomes clear that the volumetric process is not limited only to the tail, but also extends to the body and head. The prognosis here is unfavorable; life expectancy with such a prevalence of oncological process is usually short. The photo in the top row shows a soft tissue formation with a focus of decay in the center, the images in the bottom row (left) show pathologically altered regional lymph nodes - in the gates of the liver, as well as in the tissue near the aorta and retroperitoneally, in the tissue near the gates of the left kidney. The red arrow also highlights a large solid-cystic area in the liver (metastatic in nature). Green arrows indicate fluid in the abdominal cavity.
2) The presence of a formation that has a heterogeneous structure, with uneven edges (lumpy). With computed tomography, you can evaluate its structure, determine the predominant component (solid, soft tissue; or liquid, cystic), the presence of areas of necrosis, purulent melting, calcifications, hemorrhages, etc.
What does pancreatic cancer look like? Photo (CT). The yellow circle reveals pathological tissue in the head region (with uneven edges, located near the wall of the duodenum).
3) Increased density of parapancreatic fiber. The “turbidity” of the fiber may indicate its tumor infiltration and/or an associated infection, or autolysis (self-digestion) by released enzymes (as a result of the destruction of pancreatic tissue) and the development of pancreatitis.
Please note: near the pancreatic head, the fiber loses its usual structure, its density is higher, the edges of the head are blurred and indistinct. All these are signs of infiltration of fiber by cancer cells (contact metastasis) or signs of pancreatitis (secondary).
Get a CT scan of the pancreas in St. Petersburg
4) Dilation of the pancreatic (Wirsung) duct above the site of the lesion. Cancer of the head causes expansion of the pancreatic duct in the area of the body and tail (normally it has a width of 1-2 mm, with tumor lesions it can expand to 0.5 cm or more).
On the images: a tumor of the head of the gland (in the yellow circle), yellow arrows indicate the dilated pancreatic (Wirsung) duct as a result of a violation of the outflow of secretions. Native (without contrast) computed tomography.
5) Uneven accumulation of contrasted blood by the tumor (it has a lower density compared to unchanged tissue). The solid (soft tissue) component accumulates contrast; areas of necrosis and cystic restructuring do not accumulate it, because they do not have blood vessels in their structure and remain hypodense (low density).
6) Germination of the tumor into the nearest organs (into the spleen, into the duodenum, into the superior vena cava, into the portal vein, into the splenic vein, into the hepar, into the omentum, into Gerota’s fascia, separating the retroperitoneal space from the abdominal cavity) are extremely unfavorable signs - markers of neoplasm inoperability (T4 according to TNM).
In this case, with a tumor of the head of the pancreas, surgery is not indicated, because germination of a blood vessel occurs and hemorrhage occurs in the hepatic parenchyma (hematoma is indicated by a red arrow), a space-occupying lesion is indicated by a yellow circle. According to the TNM classification, pancreatic cancer corresponds to T4 (tumor of any size with invasion into surrounding tissues, including blood vessels).
A mass formation of the tail of the gland growing into the spleen (inoperable, TNM T4), on the left - before contrast, on the right - after contrast administration. A large cystic lesion (O) was detected in the tail area (and also partially in the body area), with a predominant fluid component, with multiple zones of necrosis, close to the spleen (C), also adjacent to the anterior renal fascia on the left. Metastases (distant) are marked with red asterisks.
The same patient. CT images reformatted in the coronal plane allow assessment of the extent of the lesion. A volumetric process with germination into the spleen is clearly visible, and fluid along the edge of the spleen is also visible. Hypodense secondary lesions in liver tissue.
7) The presence of altered and enlarged lymph nodes in the parapankeratic tissue, in the para-aortic tissue, in the hilum of the liver and (or) spleen indicates lymphogenous metastasis of the neoplasm and makes it possible to set N1 according to the TNM system (N - Latin “nodus”, lymph node). TNM N1 means damage to regional (located near the organ) lymph nodes and is an unfavorable sign, but does not exclude surgical intervention.
Tumor of the head (in the yellow circle) with metastases to the lymph nodes near the porta hepatis, as well as to the para-aortic lymph nodes (green arrows). Contrast-enhanced CT images (arterioparenchymal phase contrast enhancement) are shown. According to the TNM classification, the neoplasm belongs to stage N1M1 - the presence of enlarged regional nodes with a pathologically altered structure and distant secondary foci.
Presence of liver metastases. The neoplasm can metastasize not only through the lymphogenous route, but also through the hematogenous route. The organ that is affected first is the liver, while the elimination of tumor cells occurs through the portal vein system. Detection of metastases to distant organs in pancreatic cancer is an unfavorable symptom (according to the TNM system, M1 is set - “distant metastases detected”). If distant metastases are found with a pancreatic tumor, surgery is not indicated. There are, however, modern methods of treating liver metastases (chemoembolization, ultrasound ablation, etc.), carried out in advanced oncology hospitals.
Computed tomography with contrast. Stage of the process is M1 according to the TNM classification (with the presence of symptoms of jaundice - due to compression of the common bile duct - and distant metastases). On the left, red arrows highlight multiple hypodense (low density), weakly accumulating contrast agent areas (1-3 cm in diameter), round in shape, diffusely distributed over the entire section area. On the right, under the blue arrow, is the part of the volumetric process that does not accumulate contrast (which contains a small number of arterial vessels), under the green arrow is the soft tissue part of the formation, and under the red arrow is the unchanged part of the organ (body and tail).
Pancreatic tail cancer. CT symptoms. Yellow arrows indicate a formation that has a heterogeneous structure, with multiple hypodense areas of necrosis and decay. There is a complication - massive ascites, i.e. accumulation of fluid in the abdominal cavity (fluid is marked with yellow stars). Distant metastasis is highlighted with a green arrow.
SECOND OPINION IN CANCER
Without a doubt, a pancreatic tumor is a dangerous diagnosis, which in some cases has an unfavorable prognosis. Patient survival, life expectancy, success of a particular treatment method, and choice of surgical tactics strictly depend on the stage of the tumor process. Therefore, the most important condition for successful treatment is not only the timely detection of oncopathology, but also its accurate staging using the TNM scale. In particular, it is very important for oncologists to know whether the tumor is spreading into surrounding organs and tissue, vascular damage, metastasis to the lymph nodes and liver. Therefore, it is necessary not only to undergo a modern diagnostic examination, such as CT or MRI, but also to correctly analyze the images in order to identify or exclude all of the above signs.
To be confident in the accuracy of the diagnosis, today you can order a review of CT and MRI results from specialists in the radiological diagnosis of oncological diseases. Such expert analysis is carried out in institutions that specialize in oncological and surgical pathology. This allows us to increase the accuracy of diagnosis and describe the disease according to modern standards. The resulting expert opinion is an accurate guideline for the attending physicians - oncologist surgeons.
You can get a Second Opinion on a CT scan of the pancreas in the National Teleradiological Network (NTRS) system. This service receives complex and controversial diagnostic cases from all Russian regions. Specialists from the Moscow Institute of Surgery named after. Vishnevsky and other specialized centers will conduct a remote review of your CT or MRI. It is enough to download CT or MRI images from a disk on the NTRS website and receive a qualified report signed by a doctor within 24 hours.
Vasily Vishnyakov, radiologist
Read more about Second Opinion
Read more about telemedicine
Pavel Popov
Candidate of Medical Sciences, Member of the European Society of Radiologists