INTRODUCTION
Transabdominal ultrasound continues to be the most commonly used first-line imaging modality in the diagnosis of abdominal disease.
Ultrasound of the pancreas is challenging given its retroperitoneal location with overlying structures and relatively small size.
Currently, the sensitivity and specificity of transabdominal ultrasonography in diagnosing pancreatic diseases and the ability to differentiate acute and chronic inflammation from precancerous or malignant lesions have not yet been determined. Today we have high-resolution real-time images where the spatial resolution matches the best CT or MRI with the best image quality. In addition, image quality and especially the amount of information are evolving with technological progress and the introduction of new techniques such as CEUS and elastography.
Figure 1 shows a standard B-mode image of the pancreas, liver, and surrounding vessels with a 1-5 and 12-15 MHz probe.
Figure 1:
Pancreas and surrounding anatomical landmarks. A : B-mode image with 1-5 MHz sensor; B : B-mode image with 12-15 MHz sensor.
Ultrasound of the pancreas can be difficult given its retroperitoneal location, variation in appearance among individuals, and body habitus. Obstructive bowel gas and obesity are the most common limitations on abdominal pancreatic scanning.
Due to food-related production of intestinal gas that reflects ultrasound beams, each examination should be performed on an empty stomach. Ultrasound of the pancreas includes transverse, longitudinal and oblique angled scans. Successful imaging can often be achieved by manipulating the probe and is directly related to the skill and persistence of the clinician. By applying graded pressure with a transducer, intestinal gas can be removed and all parts of the pancreas: head, neck, body and tail can be visualized. Further improvement in visualization can also be obtained by drinking two glasses of water/juice, thereby using the fluid-filled stomach as an acoustic window.
The tail of the pancreas may be difficult to access on transverse scans. Figure 2 shows the trans-splenic approach, where the tail of the pancreas (cauda pancreatis) is scanned from the left lateral side using the spleen as an acoustic window.
Figure 2
When examining the pancreas, the echotexture, size of the gland, including the main pancreatic duct, and anatomical landmarks of the pancreas should be assessed. The echotexture in a normal pancreas is isoechoic or hyperechoic compared to a healthy liver. Often the echogenicity of the pancreas increases with age. The approximate anteroposterior dimensions of the pancreas are: head (2.5 cm), body (1.5 cm), tail (3.5 cm), and pancreatic duct (<2.5 mm). Fatty replacement (lipomatosis) of the pancreas and a decrease in its size are common in older people, but can also be found in patients with cystic fibrosis, CP, some types of diabetes and other diseases.
Landmarks of the surrounding vessels, ducts and abdominal organs are the portal vein, splenic vein, confluence with the mesenteric vein, vena cava, aorta, superior mesenteric artery, common hepatic artery, splenic artery, common bile duct, duodenum, stomach and liver.
Ultrasound of the pancreas
The pancreas is very important in the digestive system. Many diseases negatively affect the functioning of this organ, which negatively affects the body as a whole. One of the effective ways to check the pancreas is ultrasound diagnostics (ultrasound). This technique is completely safe and can be performed on both adults and children.
Location of the pancreas in the human body
The pancreas is located behind the stomach on the left side, fits very tightly to the duodenum, and is also under the reliable protection of the ribs. Why is the role of the pancreas so important in digestion? The fact is that it secretes about two liters of pancreatic juice per day, thanks to which the process of digesting food is carried out.
The thickest part of the organ is the head, then it passes into the body and tail, the end of which is located near the spleen. The pancreas is covered by a special membrane. It is worth noting that the health of the organ is directly related to the urinary tract.
When is an ultrasound scan of the pancreas prescribed?
The pancreas must be checked by ultrasound diagnostics if the patient:
- Complains of pain in the area of the left ribs, but the doctor cannot determine the cause by palpation;
- He is losing weight sharply.
If there is pathology in laboratory tests, ultrasound diagnostics of the pancreas is mandatory. In addition, diagnosis of the gland is prescribed after suffering from diseases such as hepatitis A, C, B.
Other situations in which an ultrasound scan of the pancreas is required:
- Feeling of bloating;
- Bitter taste in the mouth;
- Yellow skin tone;
- Problems with stool;
- Abdominal trauma;
- Detection of tumors.
As part of the pancreatic examination, a complete diagnosis of the abdominal cavity is carried out. The study allows us to identify pathologies at the very initial stage. This will help to prescribe treatment as soon as possible and avoid the development of the disease. After all, gland diseases directly affect the health of other organs.
An ultrasound examination of the pancreas is recommended once a year for all people over 25 years of age.
What is included in preparation for an ultrasound.
To obtain a reliable result during diagnosis, you must follow all the rules for preparing for it. If the rules are ignored, the results of the study may be distorted or difficulties may arise during the ultrasound. First of all, you should completely cleanse the intestines through an enema or taking laxatives. Two days before the test, it is allowed to take sorbents that help reduce the formation of gases.
Two days before the ultrasound, you should completely remove from the diet:
- alcoholic drinks and soda;
- fresh fruits/vegetables;
- dairy products;
- meat;
- eggs;
- black bread.
You can eat cereals, fruits that have undergone heat treatment, and honey.
Eating later than 12 hours before the test is unacceptable.
It is better to plan the examination for the first half of the day, because eating and drinking before the examination on this day is not allowed. Chewing gum and smoking are also prohibited. If you take medications, be sure to ask your doctor how to take them before your ultrasound.
What you need to keep in mind if you need to check your pancreas:
In some cases, a special diet is prescribed only by a doctor; it depends on the individual characteristics of the body;
If you are overweight, the enema should be done 2 times: on the eve of the procedure and on the day of the study.
If all recommendations are not followed, the ultrasound result will lose its information content by 50%.
How is an ultrasound of the pancreas performed?
The pancreas is diagnosed using ultrasound within 30-60 minutes. The procedure is performed lying on your back. A special gel is applied to the stomach. Then the ultrasound doctor begins to conduct the examination using a special sensor. If necessary, the doctor may ask the patient to retract or inflate the abdomen.
During the ultrasound, the patient will need to lie first on the right side and then on the left side; in some cases, the doctor asks the patient to stand on his feet. This is required in order to examine the pancreas as thoroughly as possible.
Immediately after performing the ultrasound, the doctor gives the patient a transcript and, if necessary, comments on certain points in order to focus the patient’s attention on them.
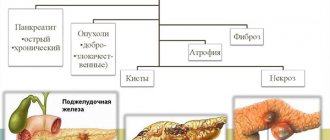
Diseases that can be detected through pancreatic ultrasound diagnostics.
The appearance of pancreatitis in the acute stage is indicated by a decrease in the echo signal. In this case, the gland becomes completely white. If the picture becomes less intense, this may indicate the presence of pancreatic edema.
The presence of tumors in the pancreas can be indicated by deviation of its tail. If the echo signal becomes stronger, this may indicate a chronic stage of pancreatitis or the presence of oncology. In places where it appears, the color of the pancreas will differ from the main one.
If the size of the liver or gallbladder increases, this may also indicate the presence of neoplasms. To identify its etiology, a piece of tissue is sent for histological examination.
Abscesses that contribute to the appearance of cavities with cloudy exudate indicate pancreatic necrosis. If the Wirsung duct is dilated, this may indicate an inflammatory process in the gland.
It is worth noting that many dangerous diseases may not manifest themselves at all in the early stages, but can be diagnosed through ultrasound. Therefore, in no case should you ignore the study if it was prescribed by the doctor.
What indicators are considered normal?
Ultrasound of the pancreas allows you to assess the health of the organ. The following are normal pancreatic values in adult patients:
- The echo signal is average, but becomes higher as the patient ages;
- The structure is holistic, homogeneous, reminiscent of the liver. The appearance of small inclusions is allowed;
- All parts of the pancreas should be clearly visible;
- The diameter of the Wirsung duct should be 1.5-2.5 mm, it should not be dilated;
- There is no deformation in the vascular pattern;
- Normal size indicators: body from 8 to 18 mm, head 18-28 mm, tail from 22 to 29 mm.
Normal indicators for an adult differ from those typical for a child.
Once again, we would like to note that the diagnosis of the pancreas is carried out as part of a comprehensive ultrasound diagnostic of the abdominal cavity. This is due to the fact that it is quite difficult to identify diseases of the pancreas using ultrasound, but it is possible to diagnose diseases of the organs bordering it, which makes it possible to assess the general condition of the abdominal cavity. If abnormalities are detected during an ultrasound, the doctor prescribes additional tests.
Ultrasound diagnostics of the pancreas makes it possible to safely and in a short period of time detect the disease at an early stage and prevent it in a timely manner.
Ultrasound of the pancreas in N. Novgorod
Diagnosis of the pancreas in our city is carried out at the VIP Academy clinic. The study is performed by doctors with more than 15 years of experience. All of them are certified specialists. The clinic has two high-tech ultrasound machines on which examinations are performed. The equipment makes it possible to most accurately assess the condition of the pancreas and nearby organs. The cost of diagnostics is the city average.
You can find out more detailed information about the study, as well as sign up for an ultrasound scan, from the administrators of the VIP Academy clinic. Phone number: +7 (831) 200-47-38.
Tissue Harmonic Mode
Tissue harmonic imaging (THI) overcomes several limitations of B-mode. By obtaining harmonic overtones instead of radiated frequencies, reverberation artifacts are reduced. Image quality is improved by better delineating between fluid and solid structures, increasing spatial and contrast resolution, making millimeter-sized structures detectable. Thus, THI ultrasound may have better resolution than CT and MRI in the absence of excessive obesity or large amounts of intestinal gas, which may temporarily mask the pancreas. There are only a few downsides to THI: reduced frame rate, reduced penetration, and only marginally improved near-sound field image quality. This modality is commonly used with CEUS.
DO YOU CARE CORRECTLY FOR YOUR ULTRASOUND DEVICE?
Download your care guide now
Download PDF
Dopplerography
The combination of gray scale B-mode and color Doppler ultrasound significantly improves overall accuracy. According to international convention, Doppler color is coded such that red expresses the flow towards the ultrasound transducer, while blue expresses the flow away from it. Recent technological advances, particularly increased sensitivity to color Doppler, are facilitating the diagnosis and staging of pancreatic diseases. Doppler imaging of the pancreas can more accurately show the outline of the organ because the pancreas is surrounded by blood vessels. Normal intrapancreatic vessels are small and difficult to demonstrate with conventional Doppler ultrasound. Color Doppler shows flow in normal surrounding vessels and abnormal vascularity, such as in tumors with high vascular infiltration or tumor infiltration in vessels. This method can also differentiate between cystic vascular processes without flow and aneurysm. Very small pancreatic calcifications, which are difficult to distinguish in the irregular tissue of the pancreatic parenchyma in CP, can be identified by the presence of flickering artifacts. Modern high-quality scanners can differentiate between inflammation (high flow) and non-flow infarction.
Contrast-enhanced ultrasound
With this technique, lesions can be studied in real time in a manner similar to contrast-enhanced CT or contrast-enhanced MRI under full operator control.
The advantage of CEUS is the ability to study the dynamics of lesions in real time. Excellent tolerance and safety profiles allow repeat dosing in the same session if necessary.
New technologies can distinguish between normal pancreatic perfusion and pathology in parenchymal pancreatic diseases or different perfusion patterns of tumors that can be visualized using small microbubbles of ultrasound contrast agents. Figure 3 shows an example of a CEUS study of the pancreas with a motion-tracked region of interest.
Figure 3:
Perfusion analysis of the pancreas. Dual image contrast-enhanced ultrasound of the pancreas in a healthy volunteer. 1.5 mL of Sonovue was injected as a bolus and detected in the region of interest approximately 45 s later.
Symptoms of pancreatitis
Manifestations of pathology vary depending on the form - acute or chronic pancreatitis. In acute pancreatitis the following are observed:
- The pain is intense, constant, the nature of the pain is described by patients as cutting, dull.
- High body temperature, high or low blood pressure - the patient’s well-being quickly deteriorates due to the rapid development of the inflammatory process.
- Pale or yellowish complexion.
- Nausea and vomiting - dry mouth and a white coating appear, attacks of vomiting do not bring relief. The most correct step at this moment is to fast; any food intake can only worsen the situation.
- Diarrhea or constipation - stool in acute pancreatitis is most often foamy, often with a foul odor, with particles of undigested food. On the contrary, there are constipation, bloating, and hardening of the abdominal muscles, which may be the very first signal of an acute attack of pancreatitis.
- Bloating – the stomach and intestines do not contract during an attack.
- Shortness of breath - appears due to loss of electrolytes during vomiting.
Chronic pancreatitis is characterized by the following symptoms:
- Abdominal pain - may be girdling or have a clear localization radiating to the back. Appears after eating.
- Intoxication of the body - general weakness, loss of appetite, tachycardia, increased body temperature, and decreased blood pressure appear.
- Endocrine disorders - ketoacidosis, diabetes mellitus, tendency to hypoglycemia. Bright red spots may also appear in the abdomen, back, and chest, which do not disappear with pressure.
With a long course of the disease, the patient gradually develops anemia, weight loss, dry skin, brittle hair and nails, symptoms of vitamin deficiency, and increased fatigue.
Elastography
RV elastography provides a high-quality map of deformation, often as a color pattern superimposed on a B-mode echo, visualizing local deformation as a result of endogenous movement or acoustic impulse. An alternative is the shear wave method, which provides quantitative elasticity information based on the shear wave velocity. Figure 4 shows an elastography image of the pancreas.
Figure 4:
Endoscopic ultrasound with elastography of chronic pancreatitis. Endoscopic ultrasound in B-mode (right) and elastogram with ultrasound overlay (left). This image shows the head of the pancreas, hyperechoic foci and filaments in the parenchyma, as well as heterogeneous echogenicity, which are signs of chronic pancreatitis. The elastogram shows predominantly blue, representing harder tissue, and green, representing intermediate honeycomb hardness compared to pancreatic tissue.
Forms of pancreatitis
Acute – characterized by acute girdling pain in the upper abdomen. Pain often appears after eating fatty foods or alcohol. Unpleasant sensations can be either barely noticeable or unbearable, radiating to the scapula or sternum. Nausea, vomiting, and stool disturbances are observed. Due to the obstructed flow of bile, the skin takes on a yellowish color.
Chronic - the main localization of pain is on the upper part of the abdominal wall with irradiation to the back, chest (left side), lower abdomen. Unpleasant sensations occur after eating heavy fatty foods, alcoholic drinks, and constant stress.
The development of chronic pancreatitis is characterized by nausea, loss of appetite, bloating, bowel dysfunction, and sometimes vomiting.
The chronic form of the pathology differs from the acute form by periods of remission and exacerbation. As the disease progresses, periods of exacerbation become more frequent; intestinal disorders, disturbances in normal digestion, and weight loss are possible.
Chronic pancreatitis often causes complications (stomach bleeding, cancer, cysts and abscesses, liver damage, diabetes mellitus, enterocolitis). That is why you need to take the disease seriously and, at the slightest suspicion of the development of inflammation, consult a doctor.