The text is presented for informational purposes only. We strongly urge you not to self-medicate. When the first symptoms appear, consult a doctor. We recommend reading: “Why you can’t self-medicate?”
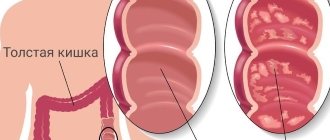
Typhlitis is an inflammation of the mucous membrane of the cecum. The cecum is a small part of the colon (only 3-10 cm). However, inflammation of its mucous membrane leads to serious digestive disorders. If the cause of the pathology is not identified and eliminated, over time the inflammation will spread to the rest of the intestine and serious complications will arise.
Medical products (drugs, medicines, vitamins, dietary supplements) are mentioned for informational purposes only. We strongly do not recommend using them without a doctor's prescription. We recommend reading: “Why can’t you take medications without a doctor’s prescription?”
Classification of typhlitis
According to morphological changes
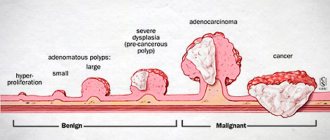
Based on how pathologically the mucous membrane is changed, typhlitis is distinguished:
- catarrhal;
- ulcerative
Due to the occurrence
Depending on the factor that caused typhlitis, it can be:
- Infectious. Inflammation of the cecum is caused by Shigella, dysenteric amoeba, and less commonly tuberculous typhlitis occurs. It is extremely rare that the cecum is affected by sexually transmitted infections (these diseases are characterized by total damage to the colon - colitis). Mycosis of the cecum (infection with pathogenic fungi) is difficult to treat.
- Toxic. Occurs due to damage to the mucous membrane by chemicals. These can be either waste products of pathogenic and opportunistic microorganisms, or low-quality food.
- Allergic. In case of individual intolerance to foods or medications, certain components cause irritation of the mucous membrane. This is how inflammation occurs.
- Ray. Radiation therapy used to treat cancer contributes to the onset of the disease.
- Inflammation of unknown etiology. This group includes Crohn's disease, microscopic typhlitis, eosinophilic. These diseases are mainly associated with autoimmune pathological processes.
According to the form of flow
- spicy;
- chronic.
Causes of typhlitis
The probable causes of the development of this pathology may be pathogenetic factors, such as:
- the presence in the diet of foods with a large amount of coarse fiber;
- consumption of excessive amounts of smoked, salted and fried foods;
- consumption of products containing large amounts of dyes and preservatives;
- regular heavy physical activity, most of which falls on the abdominal muscles (heavy loads, lifting weights);
- complications after peritonitis and chronic appendicitis;
- sepsis of internal organs, which is recorded due to blood poisoning;
- intestinal infections: Crohn's disease at a sluggish stage, ulcerative colitis, dysentery, rotavirus infections, foodborne illness, cholera, typhoid fever, salmonellosis;
- intolerance to lactose, gluten and some other animal and plant proteins;
- food allergy with a long asymptomatic course;
- organic lesions of the mucous membrane of the large and small intestines, as a result of other diseases of the digestive tract (gallbladder, stomach, pancreas);
- abdominal candidiasis;
- chronic dysbacteriosis;
Symptoms
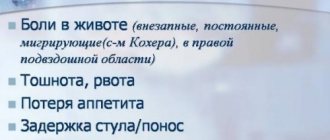
Main symptom
The most common complaint with typhlitis is pain . It occurs in the lower abdomen on the right, sometimes it is dull, but more often patients complain of colic in the right iliac region. Intensifies:
- 6 hours after eating;
- when standing for a long time;
- in a lying position on the left side.
Sometimes the pain radiates to the lower back.
Other symptoms
In addition to pain, typhlitis manifests itself:
- constipation or diarrhea (they often alternate);
- increased body temperature;
- rumbling in the stomach;
- flatulence;
- belching;
- feeling of fullness in the stomach;
- lack of appetite.
Features of the manifestation of various forms of typhlitis
In many ways, the clinical manifestations of typhlitis depend on its form.
| Symptom | Spicy | Chronic | Catarrhal | Ulcerative |
| Pain | Sharp, strong colic type | Dull, aching sometimes intensifies | Not intense | Cramping |
| Body temperature | Suddenly rises. Can increase up to 40 °C | Normal or subfebrile. Sometimes during periods of exacerbation it can suddenly rise to high values. | 37.1-38.3 °C | Over 38 °C. If the disease is chronic, then the temperature may be normal (up to 37.1 ° C) |
| Presence of impurities in stool | Depends on the degree of damage to the mucous membrane | Mucus, sometimes pus | Mucus, pus, blood | |
| Constipation | Typhlitis is characterized by alternating constipation with diarrhea. More often, retention of feces in the cecum is the cause of inflammation. And constipation itself occurs due to the consumption of food low in dietary fiber and a violation of the evacuation function of the large intestine. | |||
| Frequency of bowel movements | Depends on the severity of the disease:
| |||
Be sure to read:
Rectum: sections, structure, functions and diagnosis of the organ
Causes of Ulcerative Colitis
Like many other chronic diseases (asthma or hypertension), ulcerative colitis does not occur due to any one cause. The disease is more common in people whose relatives suffer from autoinflammatory or autoimmune diseases; in those who in childhood often received antibiotics, painkillers, or moved to distant countries. However, none of these factors alone causes ulcerative colitis. Rather, a combination of many events causes the immune system to attack the intestines.
There are many immune cells in the intestinal wall, and in the intestine itself there are many bacteria. The immune system is able to identify obviously harmful bacteria and reacts to them: it releases substances that cause inflammation and destroy bacteria (cytokines, reactive oxygen species). In ulcerative colitis, this process is disrupted: the immune system does not work correctly and mistakes “normal” bacteria for “enemies.”
With an intestinal infection, the protective inflammation of the intestines quickly ends, but with ulcerative colitis, immune cells maintain inflammation in the colon, attracting more and more cells. Therefore, ulcerative colitis rarely goes away on its own, without medication.
Causes and factors of occurrence
Typhlitis occurs when various agents act on the cells of the mucous membrane of the cecum. Increase the risk of its development:
- intestinal infections;
- dysbacteriosis;
- poor nutrition;
- medications (cytotoxins, antibiotics);
- autoimmune pathologies;
- ileocecal valve insufficiency;
- irritation of the mucous membrane of the cecum with bile;
- violation of intestinal evacuation function;
- chronic stress;
- violation of neurohumoral regulation of intestinal function;
- frequent trauma to the mucous membrane with feces during constipation;
- defect of local immunity of the mucous membrane of the cecum.
Typhlitis is a common condition that occurs against the background of immunodeficiency (including after chemotherapy, a long course of antibacterial therapy, and blood diseases). Occurs mainly in childhood and old age. It is rarely detected in people with intact immunity.
Based on clinical manifestations, it is impossible to accurately establish a diagnosis and determine the cause of the disease.
According to statistical data, such symptoms reveal:
- 60% of cases are tumor and inflammatory diseases of the ileocecal region;
- 10% – dysfunction of the colon;
- 5% – pathologies not related to the ileocecal region (inguinal hernia, adnexitis, etc.).
It is especially difficult to determine the disease only by the nature of the pain. The same pain as with typhlitis is characteristic of appendicitis. And if inflammation of the cecum, especially catarrhal inflammation, which occurs in a mild form, can be treated conservatively, then in case of appendicitis, severe ulcerative lesions of the cecum, urgent surgery is necessary. Therefore, it is imperative to undergo diagnostics.
Diagnostic methods
If the symptoms described above are detected, the patient should urgently seek professional medical help. At an appointment with a specialist, the patient will receive directions for the following clinical activities:
- Consultation with a gastroenterologist.
- Stool collection.
- Carrying out irrigoscopy and parietography.
One of the most pronounced complaints with this disease, clearly visible when scanning with an X-ray machine, is changes or shortening of the intestine. In certain situations, barium dots appear on the inside of the mucosa, indicating the presence of ulcers and erosions. More accurate examinations involve identifying the disease and distinguishing it from diverticulitis of the large intestine, oncology, appendicitis and other unfavorable processes.
Diagnostics
When diagnosing, the following goals are pursued:
- Determine the cause of damage to the mucous membrane.
- Determine whether other parts of the intestine are affected.
- Carry out differential diagnosis with other diseases.
To do this, you should contact a therapist or gastroenterologist. A consultation with a surgeon is required.
Required:
- general examination;
- palpation;
- auscultation;
- blood and urine tests;
- stool analysis.
For certain indications the following is prescribed:
- Ultrasound of the abdominal organs;
- x-ray with oral administration of contrast agent;
- colonoscopy with biopsy - endoscopic examination of the colon and tissue sampling for histological examination;
- computed tomography (if intestinal neoplasms are suspected).
Women who complain of pain in the right iliac region must be referred for consultation to a gynecologist. Since most gynecological diseases (inflammation of the genitourinary system, ectopic pregnancy, etc.) occur with similar symptoms.
Be sure to read:
Proctitis: symptoms and treatment methods (diet, drugs, surgery)
To clarify the cause of typhlitis, a morphological study is required. Only after a biopsy can you most accurately determine whether the disease is caused by autoimmune disorders or other factors. In the presence of ulcers, a biopsy is mandatory, since such lesions of the mucous membrane occur in the initial stages of cancer, precancerous diseases.
Irritable bowel syndrome
Irritable bowel syndrome is a complex of functional (i.e., not associated with organic damage) disorders of the colon, lasting more than 3 months, in which abdominal discomfort or pain is associated with bowel movements or changes in habitual bowel function and stool disorders.
Epidemiology
The prevalence of IBS in most countries of the world averages 20%, ranging from 9 to 48%. The range in prevalence rates is explained by the fact that two thirds of people experiencing symptoms of IBS do not go to a doctor and only a third of patients seek help from a doctor. The social and cultural level of the population largely determines the rate of treatment of the population regarding the disease.
In developed countries of Europe, America, Japan, China, the incidence of treatment is high and the prevalence of the disease reaches 30%. In countries like Thailand it is 5%, but in Iran it is only 3.4%.
Recent epidemiological studies among Hispanics and African Americans in the United States, residents of Japan and China have shown that the prevalence of the syndrome does not depend on race and averages 20% in all studied groups.
The incidence of IBS is 1% per year. The peak incidence occurs in young working age – 30–40 years.
The ratio of women and men among patients, according to various sources, varies from 1:1 to 2:1. The latest epidemiological studies have shown that among men of the so-called “problem” age (after 50 years), IBS is as common as among women. The social status of the sexes determines the referral rate for IBS symptoms. In those countries where women are emancipated and have equal rights with men, for example in Russia, Europe and America, their referral rate for IBS symptoms is 2–4 times higher than that of men. In countries where women have a low social status, for example in India and Pakistan, men are 4 times more likely to present with symptoms of IBS and, according to statistics, there is a significant predominance of men among patients. In most African countries, uptake rates are equal for both men and women, resulting in a 1:1 sex ratio.
The average age of patients is 24–41 years. Among older adults, 65–93 years of age, the prevalence of IBS is 10.9%, compared with 17% in those 30–64 years of age. Epidemiological studies have shown a definite relationship between the prevalence of IBS and place of residence. It is noted that among rural residents who engage primarily in physical labor and eat plant foods, the syndrome occurs much less frequently than among urban residents. In turn, among city dwellers, IBS is most common in large cities and capitals; it is somewhat less common among residents of large cities and is even less common among the population of urban settlements.
Etiology and pathogenesis According to modern concepts, IBS is a biopsychosocial disorder, the development of which is based on the interaction of 3 pathological mechanisms:
- psychosocial impact
- sensory-motor dysfunction , i.e. disturbances in the sensitivity and motor activity of the intestine, which can lead to gynecological diseases (causing reflex disorders of the motor function of the colon), endocrine disorders - menopause, dysmenorrhea, premenstrual syndrome, obesity, hypothyroidism, diabetes mellitus;
- persistent neuroimmune damage that develops after infectious intestinal diseases and is considered as a possible cause of the formation of sensory-motor dysfunction.
Clinic
The IBS clinic is extremely diverse. The most characteristic symptoms are the following:
- Abdominal pain - observed in 50-96% of patients, they are localized around the navel or in the lower abdomen, and have varying intensity (from slight aching to very pronounced intestinal colic). As a rule, pain decreases or disappears after bowel movements or passing gas. The basis of pain in IBS is a violation of the nervous regulation of the motor function of the colon and increased sensitivity of the receptors of the intestinal wall to stretching. An important distinguishing feature is the absence of pain and other symptoms at night.
- Abnormal stool is observed in 55% of patients and is expressed in the appearance of diarrhea or constipation. Diarrhea often occurs suddenly after eating, sometimes in the first half of the day. The stool often contains mucus. Many patients experience a feeling of incomplete bowel movement after bowel movements. Often the urge to defecate occurs immediately after eating. This is especially pronounced after eating fatty and high-calorie foods. It is possible to alternate between diarrhea and constipation: in the morning, the stool is dense or in the form of lumps with mucus, and during the day there are several half-formed stools.
- Flatulence is one of the characteristic signs of IBS, usually worsening in the evening. As a rule, bloating increases before bowel movements and decreases after it. Quite often, flatulence is local in nature. A. V. Frolkis (1991) identifies three main syndromes.
Splenic flexure syndrome is the most common.
Due to anatomical features (high location under the diaphragm, acute angle) in the splenic flexure in patients with IBS and motor dysfunction, favorable conditions are created for the accumulation of feces and gas and the development of splenic flexure syndrome. Its main manifestations are as follows:
- feeling of fullness, pressure, fullness in the left upper abdomen;
- pain in the left half of the chest, often in the heart area, less often in the left shoulder area;
- palpitations, a feeling of lack of air, sometimes these phenomena are accompanied by a feeling of fear;
- the appearance or intensification of these manifestations after eating, especially a large meal, stool retention, exciting situations and a decrease after the passage of gas and bowel movements;
- bloating and severe tympanitis in the left hypochondrium;
- accumulation of gas in the area of the splenic flexure of the colon (detected by X-ray examination).
Hepatic flexure syndrome - manifested by a feeling of fullness, pressure, pain in the left hypochondrium, radiating to the epigastrium, right shoulder, right half of the chest. These symptoms mimic bile duct pathology.
Cecal syndrome is common and simulates the clinical picture of appendicitis. Patients complain of pain in the right iliac region, radiating to the right abdomen; the intensity of pain may gradually increase, but, as a rule, does not reach the same severity as in acute appendicitis. Non-ulcer dyspepsia syndrome - observed in 30-40% of patients with IBS. Patients complain of a feeling of heaviness and fullness in the epigastrium, nausea, and belching of air. These symptoms are caused by impaired motor function of the gastrointestinal tract.
- Severe neurotic manifestations are quite common in patients with IBS. Patients complain of headaches (resembling a migraine), a sensation of a lump when swallowing, dissatisfaction with inhalation (a feeling of lack of air), and sometimes frequent painful urination.
Treatment
Eliminate environmental factors that are traumatic to the psyche, treat the patient in a sanatorium, dispensary, and in case of prolonged and repeated attacks of intestinal dyskinesia or functional stomach disorders - in a hospital.
If constipation predominates, diet No. 3, rich in dietary fiber: wheat bran, oat bran added to soup, rye bread, buckwheat porridge, grated carrots, beets; Spices, hot sauces, refractory fats, pastry products, fresh milk, and strong coffee are contraindicated.
Physiotherapeutic and balneological procedures: aeroionotherapy, galvanic collar according to Shcherbak, solux, diathermy, electrosleep, acupuncture, pine baths, ozokerite applications.
If there are concomitant diseases (hypothyroidism, allergic enterocolitis, dysbacteriosis, menopause, etc.), treat them.
Treatment of neuroses and depression, including psychotherapy, sedatives. For constipation - mild laxatives, oil enemas.
For spasms with pain - papaverine, no-spa.
For dominant diarrhea, antidiarrheal drugs are prescribed.
Treatment
Treatment of the disease depends on:
- degree of damage;
- causes of pathology;
- flow forms.
In mild and moderate cases, treatment is carried out conservatively, and radical methods are resorted to if conservative therapy does not help. To avoid surgery, the patient must:
- stick to a strict diet;
- take the medications prescribed by the doctor;
- use folk remedies as a complementary method, having previously discussed the possibility of such treatment with a doctor.
If typhlitis occurs with complications, surgical intervention is necessary.
Diet
Patients are recommended to use:
- Meat of dietary grades. It is a source of protein and iron.
- Dairy products. Necessary to compensate for the lack of protein and calcium. It is better to use low-fat, non-acidic cottage cheese, bio-kefir or bio-yogurt (to restore microflora in case of dysbacteriosis), and hard varieties of cheese. Milk in its pure form is acceptable if the patient tolerates it normally. Usually, with intestinal diseases, fresh milk causes bloating and abdominal pain.
- Raw vegetables and fruits can only be thoroughly ground as a source of vitamins. Better in the form of homogenized purees.
- Boiled porridge. For constipation, it is better to eat buckwheat, oatmeal, and barley. If the patient has diarrhea, then rice and semolina are recommended.
During illness or during exacerbation of a chronic process, it is recommended to exclude from the diet:
- foods rich in dietary fiber (although they help eliminate constipation);
- smoked meats;
- spicy dishes;
- canned food;
- carbonated drinks;
- kvass;
- alcohol (even low-alcohol drinks).
Meals should be fractional (5-6 times). During the period of exacerbation of the disease, treatment table No. 3 is recommended (if the disease is accompanied by constipation); in case of diarrhea, diet No. 4 is prescribed.
Nutritional therapy does not replace medications. But nutrition also plays an important role in the treatment of inflammation of the cecum.
Medicines
Medicines are prescribed depending on the cause and severity of symptoms:
- Antibiotics. They are necessary for proven bacterial etiology of typhlitis. If the disease is caused by fungi, antifungal drugs are prescribed.
- Antipyretic and anti-inflammatory drugs are recommended at temperatures above 38.3 °C.
- Antispasmodics are prescribed if the disease is caused by a spasm of smooth muscles. In this case, antispasmodics even relieve pain.
In addition, they prescribe:
- absorbents;
- astringents;
- anti-inflammatory;
- motor modulators.
Self-prescribing medications is not recommended. Only a doctor can choose the safest and most effective drugs, depending on the cause and severity of the disease.
Surgery
Indications for surgery:
- lack of effect from conservative therapy;
- development of complications (general peritonitis, intestinal perforation, bleeding);
- detection of neoplasms in the cecum.
Be sure to read:
Peritonitis: what kind of disease is it, how does it manifest and be treated?
The volume of the operation depends on the extent of the process. Resection of the affected area and restoration of intestinal integrity is performed. An examination of the abdominal organs is indicated.
Traditional methods
Traditional methods can be used as an additional component of complex treatment of typhlitis.
- For constipation, cleansing enemas with a decoction of chamomile and calendula are recommended (see here).
- A decoction of chamomile, yarrow, St. John's wort, and rose hips will help relieve inflammation and restore the water-salt balance disturbed by diarrhea and vomiting (see more about the use of herbs for the treatment of gastrointestinal diseases).
- Thermal procedures (warming up with heating pads, warm compresses) are indicated if there is no purulent process.
- Tea made from motherwort, lemon balm, valerian, and peppermint will help with typhlitis caused by prolonged stress.
It is extremely dangerous to treat typhlitis using exclusively folk methods, especially without preliminary diagnosis. The disease will lead to serious consequences.
Treatment options
Currently, modern medicine offers two types of therapeutic measures: symptomatic and etiological. And for the most effective treatment for typhlitis, doctors recommend:
- Adhere to a healthy and proper diet.
- Carry out massage procedures in the intestinal area.
- Local heat sessions.
- Use of enzyme medications.
- Use of infusion procedures.
- Promptly treat other diseases that can cause the described illness.
Possible consequences and prognosis for life
Untreated typhlitis for a long time is dangerous because the inflammatory process will affect the small intestine, other parts of the colon, and the peritoneum. In addition, other complications may arise:
- intestinal bleeding;
- abscess;
- peritonitis;
- perforation of the ulcer;
- sepsis.
Tiflitis leads to other equally serious consequences. So, with ulcerative hemorrhagic typhlitis, anemia will develop due to frequent bleeding. Inflammatory processes contribute to tissue necrosis and gangrenous changes. Due to the inflammatory process, absorption processes are disrupted, resulting in:
- Iron-deficiency anemia;
- hypo-, avitaminosis;
- hypocalcemia.
If typhlitis is accompanied by diarrhea, vomiting disrupts the water-salt balance.
Typhlitis, especially if it occurs in a mild form, can be treated with conservative therapy if treated in a timely manner. If you follow your doctor's recommendations, a quick recovery is possible. But if complications arise, the prognosis for life is somewhat worse. There is a high probability of death with peritonitis, massive intestinal bleeding, and perforation.
Prevention
The patient must comply with the following preventive measures:
- prevent the development of infectious intestinal diseases;
- If diarrhea or constipation develops, treat them immediately;
- eat small and healthy meals;
- to refuse from bad habits;
- eliminate foci of inflammation from the body, undergo regular examinations.
Typhlitis is a predictable disease, which can be easily eliminated if the patient behaves correctly and strictly follows all the recommendations of the attending physician.
More details: https://www.gastromap.ru/bolezni/drugie-bolezni-kishechnika/tiflit.html#ixzz430jlhzML
Features and benefits of treatment for ulcerative colitis at the Rassvet Clinic
Doctors at the Rassvet Clinic use treatment protocols for ulcerative colitis developed by the world's leading associations (ACG, ECCO) and based on reliable scientific research. Our specialists do not use unproven methods for treating ulcerative colitis, such as a strict diet, and help create a treatment plan during pregnancy and breastfeeding. To protect against the side effects of immunosuppressants, the doctor will propose a vaccination plan and draw up a schedule of blood tests that will allow timely recognition of unwanted reactions to medications.
Author:
Golovenko Alexey Olegovich gastroenterologist