While sitting at the holiday table, few people think or remember about the possible consequences that can significantly overshadow the joyful memories of the holiday: the occurrence or exacerbation of existing diseases of the digestive system, one of which is pancreatitis.
Unfortunately, if we look at statistical studies, this serious disease is very common, and its incidence continues to increase. Over the past thirty years, there has been a more than twofold increase in the number of pancreatitis. It is difficult to name the true incidence figures, and the frequency of chronic pancreatitis among the population of different countries varies from 0.2 to 0.68%. The disease is diagnosed in 6-8% of gastroenterological patients.
In developed countries, chronic pancreatitis has become noticeably “younger”: the average age of patients diagnosed with this disease has decreased from 50 to 39 years, and the proportion of women among patients has increased by 30%. The proportion of alcoholic pancreatitis increased from 40 to 75%.
There is also an increase in the incidence of pancreatic cancer, which develops against the background of chronic pancreatitis. In Russia, an even more dramatic increase in incidence is observed: for example, the prevalence of chronic pancreatitis among children is 9-25 cases, and among adults – 27-50 cases per 100,000 population.
What is pancreatitis?
The name itself speaks for itself: pancreas (lat.) – pancreas, -itis (lat.) – inflammation. Pancreatitis is an inflammatory disease of the pancreas. There are two types of pancreatitis: acute and chronic. Acute pancreatitis is an acute disease based on a destructive process in the pancreas (destruction of its tissue). This is an extremely serious condition that requires inpatient treatment in a surgical department.
Chronic pancreatitis is a diffuse inflammatory continuously progressive disease of the pancreas with the development of irreversible structural changes in its tissue and ducts (normally functioning tissue is replaced by denser and non-functioning tissue - connective tissue) and the development of disorders of its function. Patients with chronic pancreatitis can be treated on an outpatient basis under the active supervision of therapists and surgeons; in some cases, inpatient treatment is required.
Acute and chronic pancreatitis: symptoms
09.06.2021
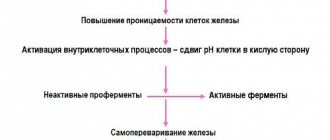
This serious illness develops when there is stagnation in the pancreas of enzymes that are supposed to process food. As a result, they promote self-digestion of the gland. Inflammation begins - pancreatitis . The reason may be:
- binge eating;
- diseases of the stomach and intestines ;
- abnormalities in liver ;
- narrowing of the gland ducts;
- alcohol and drug intoxication;
- congenital pathologies of the gastrointestinal tract (gastrointestinal tract).
Acute pancreatitis
More often occurs due to alcohol poisoning or due to a stone in the gall bladder . Also, some medications have a toxic effect on the pancreas .
4 stages of acute pancreatitis
- Lasts from 5 to 7 days. The pancreas swells and cell death occurs. The organs around the gland, the peritoneum, become inflamed. The whole body is poisoned. Possible death.
- From day 8, a pancreatic infiltrate forms.
- At the end of 2 weeks complications appear. Abscesses form, fistulas penetrate into the tissues of other organs.
- Recovery period. If pancreatitis is mild, there may be no complications (the patient recovers within 3 weeks). With an average degree, the infiltrate will resolve within 2 months, but will become chronic. In severe forms, immunity . The patient loses weight sharply, and other serious diseases develop, including diabetes mellitus .
Symptoms of acute pancreatitis:
- severe pain in the abdomen of a “girdling” nature;
- uncontrollable vomiting;
- the skin on the face is pale, moist;
- the stomach is bloated (increased gas formation);
- repeated loose stools;
- heartbeat;
- possible increase in temperature;
- general weakness, malaise.
An attack of acute pancreatitis occurs quickly with intense pain. Help must be provided immediately. Otherwise, this attack can provoke the formation of an irreversible process in the pancreas (pancreatic necrosis). Therefore, a sick person must be urgently taken to the surgical department. It must be remembered that similar pain can occur with other diseases ( infarction , hepatic colic, appendicitis ). A correct diagnosis can only be made in a hospital with the help of laboratory tests and modern equipment.
Help for acute pancreatitis:
- peace;
- cold;
- hunger;
- complex therapy in a hospital (take any medications only as prescribed by a doctor !).
Chronic pancreatitis
If the gland was severely damaged during acute pancreatitis , the pain may recur. This is already a chronic stage. The ducts of the gland narrow and cysts appear. This form of pancreatitis is characterized by periodic exacerbation, which leads to disruption of normal pancreatic . Sometimes the chronic stage may be asymptomatic or “hidden under the mask” of another ailment ( cholecystitis , stomach ulcers ).
3 stages of development:
- lasts approximately 10 years. Periods of attacks alternate with remission;
- after 10 years, painful attacks decrease, insufficiency of the secretory function of the gland appears (unstable stool, heartburn , vomiting of undigested food);
- complications develop (persistent loose stools, exhaustion of the body).
Symptoms of chronic pancreatitis:
- frequent “aching”, tingling, dull pain in the left hypochondrium;
- constant "bloating" of the abdomen ;
- unformed “liquid” stools;
- nausea or vomiting.
Help for chronic pancreatitis:
- strict diet (fractional meals);
- anti-inflammatory drugs;
- antispasmodics;
- take enzymes during meals (as prescribed by your doctor , depending on tests for pancreatic secretion).
The main thing when treating pancreatitis is to exclude the cause of the attack.
For any abdominal consultation with a gastroenterologist or surgeon is necessary . They will prescribe a special diet (for each person individually), choleretic agents, antibiotics and other drugs.
The sooner you start treating pancreatitis , the greater the chance of recovery. Also, prevention of attacks of pancreatitis ( diet , avoidance of alcohol) is of great importance in the favorable outcome of this terrible disease.
Published in Gastroentorology, Surgery Premium Clinic
Reasons for the development of pancreatitis
The main causes of primary pancreatic damage are:
- alcohol;
- heredity;
- errors in nutrition (deficiency of protein in the diet, heavy intake of fatty and protein foods while drinking alcohol);
- use of certain medications;
- circulatory disorders of the pancreas (for example, against the background of atherosclerotic vascular lesions);
- autoimmune diseases (caused by disorders in the immune system).
The causes of secondary chronic pancreatitis are:
- diseases and developmental anomalies of the gallbladder and bile ducts;
- diseases of the major duodenal papilla (the place where the bile and pancreatic ducts flow into the duodenum);
- helminthic infestations;
- liver diseases;
- mumps (popularly known as “mumps”);
- metabolic disorders (damage to the parathyroid glands, obesity, menstrual dysfunction, etc.);
- inflammatory bowel diseases of non-infectious and infectious origin;
- peptic ulcer, chronic gastroduodenitis.
Among the causes of pancreatitis in our country, alcohol abuse and cholelithiasis rank first. Scientists have found that regular consumption of alcohol up to 200 ml per day manifests itself in chronic pancreatitis after 5-8 years, and the earliest manifestations of this disease, detected only by special diagnostic methods, appear much earlier.
In patients with cholelithiasis, pancreatitis almost always accompanies the underlying disease, and sometimes even comes first. Even in the absence of biliary colic and the patient’s good subjective condition, damage to the pancreas progresses and often causes emergency hospitalization in the surgical department.
Clinical manifestations of pancreatitis
What to pay attention to:
- Loss of body weight. Decreased appetite, nausea and vomiting (possible admixture of bile), which does not bring relief, drooling. Aversion to fatty foods. Bloating, excess gas formation. Frequent, copious, fatty and foul-smelling stools.
- The development of jaundice, skin itching, and discoloration of stools is possible.
- Abdominal pain is often constant, often painful, aggravated by eating fatty and spicy foods, localized in the epigastric region, can take on the character of a “half-belt”, pain in the back and behind the sternum (in the area of the heart) is possible.
- Attacks of “ravenous hunger” (caused by a decrease in blood sugar levels) and dry mouth are possible.
- Weakness, irritability, especially on an empty stomach, sleep disturbance, decreased performance.
Chronic pancreatitis can be complicated by diabetes mellitus, intestinal dysbiosis, liver damage, cystic formations in the pancreas, pancreatic cancer, the development of gastrointestinal bleeding, abscesses of the pancreas and adjacent tissues, peritonitis, intestinal damage, pneumonia, damage to the arteries of the lower extremities, anemia, neurological disorders.
Chronic pancreatitis is not a harmless disease, which you can cope with on your own, relying on a large amount of information and a variety of treatment methods currently presented in a variety of media. You should definitely visit a doctor for timely diagnosis. A modern clinical diagnostic base makes it possible to detect the disease at the earliest stages, prescribe the correct treatment in time and prevent complications.
ATTENTION! If after a hearty holiday meal you feel unwell - nausea, aversion to fatty foods, bloating, changes in stool, know that SM-Clinic specialists are ready to help you! We work 7 days a week!
Gastritis, reactive pancreatitis, flatulence, IBS
Elena, Mytishchi
May 13, 2021
Good afternoon
Please tell me what to do in my situation? I am 28 years old. I have superficial gastritis; at 13 I had hyperplastic gastritis, but it went away. I got sick with Covid in October, took 2 antibiotics and injected another one. On New Year's Eve, I started having stomach problems. Pain appeared in the mornings and evenings. I had a gastroscopy and there was a slight exacerbation. Treatment was prescribed and she was cured. I took a bunch of tests (attached). Of these, only pancreatic amylase and Alpha amylase were problematic. In the year 16, along with an exacerbation of gastritis, I was diagnosed with reactive pancreatitis, which during this time never went away (Alpha amylase and pancreatic never returned to normal). Moreover, the exacerbation passed, I followed a strict diet for about six months, but the indicators still did not return to normal. The gastroenterologist told me that as long as there is an exacerbation, there will be reactive pancreatitis, and as gastritis goes away, so does pancreatitis, but that was not the case. The only thing that was noticed was a decrease in these two indicators over 4.5 months (I recently passed). Then, on New Year’s Eve, the attending physician prescribed me to follow a diet for six months, drink pro(pre)biotics for 10 days, sorbents for 10 days, and warm mineral water for 10 days before breakfast, lunch and dinner. And so 6 months, and the drugs are different every time. I drank almost all of it. It remains to drink 1 sorbent and probiotic. In February of this year, HPV and grade 1 dysplasia were detected; an immunostimulating drug was prescribed to suppress atypical cells, 3 courses of 10 days each with a break of 14 days. I took almost 2 courses and each time I felt very bad on all fronts (stool problems, weakness, drowsiness, pain in the stomach, intestines, fever, terrible acne, very severe hair loss), during the breaks I only came to my senses after 2 weeks of rest and it was necessary to start the next course again. I couldn’t stand the 3rd year and quit. Here I asked a question on this topic, all the doctors wrote that I didn’t need to drink it at all and just monitor it. The point is different. After the 2nd dose it didn’t go away much. The pain remained in the stomach area, under the left rib, but not in the morning, but mainly during the day and evening (now the pain is easier). But problems with stool became constant. Rarely there is formed stool, mostly liquid, not like water of course, but abnormal. Light brown with yellow. It often boils, there is pain in different places of the intestine sometimes below, on the right under the rib, and the most important problem is severe flatulence. It's a nightmare in the evening. I usually have something light for dinner before bed. During the day I sometimes eat cottage cheese and drink kefir. I don’t know if I can or not, everyone says differently. Actually, in December I just had a gastroscopy. I wouldn't want to do it again. Is it possible to do without it? And it would be possible to avoid a colonoscopy (I have never done it)? I’m very afraid to do it, and with anesthesia I’m even more afraid. My doctor said in December that I didn’t need to do it, then there was flatulence, but not so strong. Plus another problem that really upsets me is hair loss. Since the new year after Covid, I have lost half of my volume. It seemed to me that before taking the immunostimulating drug, my hair began to fall out a little less, but then I began to fall out from these pills and I don’t know what to blame: Covid, gastritis with pancreatitis, or taking medications. I remember that during the last two exacerbations of gastritis, my acne and hair loss always worsened. I would also like to receive recommendations on hair and acne. I'm very tired of this. Because all the tests (most of them were normal). When I got tested, I didn't have acne. Only after the test, a couple of weeks later, they appeared along with hair loss. Could these analyzes have changed during this time? I also have acne now. If you follow a diet, it's better. You eat a couple of cookies and that’s it, you break out, your temperature rises, it hurts under your left rib. I can't eat anything tasty. In general, my temperature is almost constantly 37, 37 and 2. I think that I have this reaction to reactive pancreatitis: a headache and a fever. When I was 16, when I ate something sweet, I almost immediately started to have a headache and a fever. But somehow it doesn’t always happen, and my reactive pancreatitis hasn’t gone away since I was 16 years old. I tested for Helicobacter a week ago and was not detected. Stool pancreatic elastase is normal, I also tested positive a week ago. I even tested the cancer antigen, CA 242. The result is less than one, while the reference result is less than 20. There is no bitterness in the mouth. The tongue is white-yellow. Now I’ve been drinking propolis for over a month now and it seems to me that I’m feeling better, I don’t know if it’s because of it or not. Can I have tomatoes, cucumbers, cottage cheese, kefir, nuts, dark chocolate? I no longer understand why it hurts and what doesn’t. And acne comes out because of everything sweet. Only if you sit on the broth for several days, roughly speaking, will your condition improve. Will it always be like this, that nothing is possible? Are there any tests that link gastrointestinal problems with hair loss and acne? Do I need to hand over something? To summarize, I would say that what worries me most is flatulence, hair loss and acne. Please help. Thank you!!! Chronic diseases:
Gastritis, cholecystitis, pancreatitis
The question is closed
gastritis
srk
flatulence
reactive pancreatitis