What it is
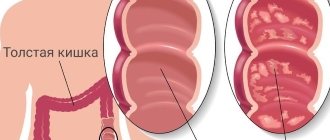
Chronic intestinal colitis is an inflammatory process that affects the mucous membrane and submucosal layer of this organ. The disorder is equally common in both women and men, but in the latter it manifests itself at a later age.
The chronic form of colitis involves phases of exacerbation and remission phases, when there are no signs. Symptoms with this form are less pronounced than with acute colitis. The pathology is diagnosed simply and treated comprehensively.
Risk factors
Risk factors for the occurrence of colitis are as follows:
- reduced immunity;
- poor nutrition;
- frequent stress;
- alcohol abuse;
- a history of autoimmune diseases;
- abnormal structure of blood vessels in the intestine.
Publications in the media
Nonspecific ulcerative colitis (UC) is a chronic inflammatory disease of the colon of unknown etiology, characterized by ulcerative-necrotic changes in its mucous membrane.
The disease always begins in the rectum and spreads proximally. Total damage to the colon occurs in 25% of cases. In severe cases, the damage can spread to the submucosa, muscular and serous membranes of the intestinal wall. Characterized by the formation of ulcers in the colon and rectum, bleeding, abscessation of the crypts of the mucous membrane and inflammatory pseudopolyposis. The disease often causes anemia, hypoproteinemia and electrolyte imbalance, and, less frequently, can lead to perforation or colon cancer.
Frequency - 2-7: 100 000. Two peaks of incidence - 15-30 years (larger peak) and 50-65 years (smaller). The predominant gender is female.
Classification • By clinical course •• acute form •• Chronic recurrent •• Chronic continuous • By severity •• Mild severity ••• Stool 4 times a day or less, pasty ••• Small amounts of blood in the stool •• • Fever, tachycardia, anemia are uncharacteristic; body weight does not change, ESR is not changed •• Severe course ••• Stool 20–40 r/day, liquid ••• Stool in most cases contains an admixture of blood ••• Body temperature 38 °C and above ••• Pulse 90 V minute or more ••• Decrease in body weight by 20% or more ••• Severe anemia ••• ESR more than 30 mm/h •• Moderate severity includes indicators that are between the parameters of mild and severe degrees.
Clinical picture
• The onset of the disease may be acute or gradual.
• The main symptom is repeated watery stools mixed with blood, pus and mucus, combined with tenesmus and false urge to defecate. During the period of remission, diarrhea may completely stop, but the stool is usually pasty, 3-4 times a day, with a slight inclusion of mucus and blood.
• Cramping pain in the abdomen. Most often this is the area of the sigmoid, colon and rectum, less often - the area of the navel and cecum. Typically, the pain intensifies before defecation and decreases after bowel movement. The localization of pain depends on the level of the lesion. Typically, the pain intensifies before defecation and decreases after bowel movement.
• Possible damage to other organs and systems •• Skin and mucous membranes: dermatitis, aphthous stomatitis (5–10%), gingivitis and glossitis, erythema nodosum (1–3%) and erythema multiforme, pyoderma gangrenosum (1–4%), ulcers lower extremities •• Arthralgia and arthritis (in 15–20% of cases), incl. and spondylitis (3–6%) •• Ophthalmological complications (4–10%): episcleritis, uveitis, iridocyclitis, conjunctivitis, cataracts, retrobulbar optic neuritis, corneal ulcers •• Liver: fatty hepatosis (7–25%), cirrhosis (1–5%), amyloidosis, primary sclerosing cholangitis (1–4%), chronic active hepatitis.
Laboratory tests • Analysis of peripheral blood •• Anemia (post-hemorrhagic - as a result of blood loss; bone marrow reaction to latent inflammation; malabsorption of iron, folic acid, vitamin B12) •• Leukocytosis of varying severity •• Increased ESR •• Hypoprothrombinemia •• Hypoalbuminemia due to malabsorption of amino acids •• Increased content of a1- and a2-globulins •• Hypocholesterolemia • Electrolyte disturbances •• Hypokalemia as a result of decreased absorption of both ions directly and vitamin D •• Hypomagnesemia.
Special studies • Sigmoidoscopy during an exacerbation is carried out without preliminary bowel preparation • Colonoscopy is prescribed after the acute phenomena have subsided, because in severe cases of the disease, perforation of the ulcer or toxic dilation is possible •• Mild UC - granularity of the mucous membrane •• Moderate UC - the mucous membrane bleeds on contact, there are ulcerative lesions and mucous exudate •• Severe UC - spontaneous bleeding from the intestinal mucosa , extensive ulcerative lesions and the formation of pseudopolyps (epithelium-covered granulation tissue) • Irrigography •• Reduced severity or absence of haustration •• Uniform narrowing of the intestinal lumen, its shortening and rigidity of the walls (the appearance of a “water pipe”) •• Longitudinal orientation of the folds of the mucous membrane with changes their structure according to the type of small and large retina •• Jagged and unclear contours of the intestinal tube due to the presence of ulcers and pseudopolyps (in the acute phase) •• The procedure is contraindicated in the development of toxic megacolon • Plain radiography of the abdominal organs is especially important in cases of severe UC, when colonoscopy and irrigography are contraindicated •• Shortening of the colon •• Lack of haustration •• Irregularity of the mucous membrane •• Dilatation of the colon (toxic megacolon) •• Free gas under the dome of the diaphragm during perforation.
Differential diagnosis • Acute dysentery • Crohn's disease • Intestinal tuberculosis • Diffuse familial polyposis of the colon • Ischemic colitis.
TREATMENT
Diet. Various diet options No. 4. You should avoid eating raw fruits and vegetables for the purpose of mechanically sparing the inflamed mucous membrane of the colon. In some patients, a dairy-free diet can reduce the severity of clinical manifestations, but if it is ineffective, it should be abandoned.
Lead tactics
• For sudden exacerbations, bowel emptying with intravenous fluids for a short period of time is indicated. Total parenteral nutrition allows for long-term rest for the intestines.
• Salicylosulfonamide drugs are effective for all degrees of severity of the disease, causing remission and reducing the frequency of exacerbations •• Sulfasalazine 0.5–1 g 4 times a day until clinical manifestations subside, then 1.5–2 g/day for a long time (up to 2 years ) for the prevention of relapses, or •• Salazodimethoxin 0.5 g 4 times / day for 3-4 weeks, then 0.5 g 2-3 times / day for 2-3 weeks •• Mesalazine - 400– 800 mg 3 times a day orally for 8–12 weeks; for the prevention of relapses - 400–500 mg 3 times a day if necessary for several years. The drug should be taken after meals with plenty of water. For left-sided UC, the drug can be used rectally (suppositories, enema). Indicated in cases of insufficient effectiveness and poor tolerability of sulfasalazine.
• GK - for acute forms of the disease, severe relapses and moderate forms, resistant to other drugs •• For distal and left-sided colitis - hydrocortisone 100-250 mg 1-2 times a day rectally by drip or in microenemas. If effective, the drug should be administered daily for 1 week, then every other day for 1–2 weeks, then gradually, over 1–3 weeks, the drug is discontinued •• Prednisolone orally 1 mg/kg/day, in extremely severe cases - 1.5 mg/kg/day In case of an acute attack, it is possible to prescribe 240–360 mg/day intravenously, followed by switching to oral administration. 3-4 weeks after achieving clinical improvement, the dose of prednisolone is gradually reduced to 40-30 mg, then sulfasalazine can be added, and then the reduction is continued until complete withdrawal.
• As an adjuvant in combination with sulfasalazine or GC - cromoglycic acid in an initial dose of 200 mg 4 times a day 15 minutes before meals.
• For mild to moderate manifestations without signs of toxic megacolon, a consolidative (eg, loperamide 2 mg) or anticholinergic drugs are cautiously prescribed. However, the use of drugs that actively inhibit peristalsis can lead to the development of toxic dilatation of the colon.
• Immunosuppressants, such as mercaptopurine, azathioprine, methotrexate (25 mg IM 2 times a week), hydroxychloroquine.
• If there is a risk of developing anemia, take iron supplements orally or parenterally; in case of massive bleeding - blood transfusion.
• For toxic megacolon •• Immediate withdrawal of consolidating and anticholinergic drugs •• Intensive infusion therapy (0.9% sodium chloride solution, potassium chloride, albumin) •• Corticotropin 120 units/day or hydrocortisone 300 mg/day intravenous drip •• Antibiotics (eg, ampicillin 2 g or cefazolin 1 g IV every 4–6 hours).
Contraindications • Sulfasalazine is contraindicated in case of hypersensitivity, liver or kidney failure, blood diseases, porphyria, glucose-6-phosphate dehydrogenase deficiency, breastfeeding • Mesalazine is contraindicated in case of hypersensitivity to salicylates, blood diseases, liver failure, gastric and duodenal ulcers, children under 2 years old, breastfeeding.
Surgical treatment • Indications •• Development of complications ••• Toxic megacolon with ineffective intensive drug therapy for 24–72 hours ••• Perforation ••• Excessive bleeding with unsuccessful conservative therapy (rare) ••• Carcinoma ••• Suspicion of carcinoma with intestinal strictures •• Lack of effect from conservative therapy, rapid progression of the disease •• Growth retardation in adolescents, not corrected by conservative treatment •• Dysplasia of the mucous membrane •• Disease duration of more than 10 years (increased risk of cancer) • The following groups of surgical interventions are distinguished • • Palliative (disconnection operations) - the application of a double-barreled ileo- or colostomy •• Radical - segmental or subtotal resection of the colon, colectomy, coloproctectomy •• Restorative-reconstructive - the application of an ileo-rectal or ileo-sigmoid anastomosis end to end.
Complications • Acute toxic dilatation (toxic megacolon) of the colon (up to 6 cm in diameter) develops in 3–5% of cases. It is probably caused by severe inflammation with damage to the muscular lining of the colon over a large area and disruption of the nervous regulation of intestinal functions. A certain role belongs to the inadequate prescription of anticholinergics and fixative drugs. The condition is usually severe, with high fever, abdominal pain, significant leukocytosis, exhaustion, and death is possible. Treatment is intensive drug therapy for 48–72 hours. Failure to respond to treatment is an indication for immediate total colonectomy. Mortality is about 20% with a higher rate in patients over 60 years of age • Major bleeding. The main symptom of UC is bleeding from the rectum (up to 200–300 ml/day). Massive bleeding is considered to be blood loss of at least 300-500 ml/day • Perforation of colon ulcers in UC occurs in approximately 3% of cases and often leads to death • Strictures in UC - 5-20% of cases • Colon cancer. Patients with subtotal or total colon disease and a disease duration of more than 10 years have an increased risk of colon cancer (at 10 years, the risk of carcinoma is 10% and can increase to 20% after 20 years and to 40% after 25–30 years) • • Colon cancer arising in the context of UC is usually multifocal and aggressive •• In patients with UC more than 8–10 years old, annual colonoscopy examinations with biopsies every 10–20 cm should be performed. In the presence of high-grade dysplasia, the possibility of prophylactic total colonectomy.
Synonyms • Ulcerative-hemorrhagic colitis, nonspecific • Ulcerative-hemorrhagic colitis, idiopathic • Ulcerative-trophic colitis • Ulcerative proctocolitis • Ulcerative-hemorrhagic rectocolitis • Purulent hemorrhagic rectocolitis.
Reduction. UC - nonspecific ulcerative colitis.
ICD-10 • K51 Ulcerative colitis
Causes
According to statistics, when visiting a gastroenterologist, 40% of patients are diagnosed with a chronic form of the disease. In approximately 30% of patients, intestinal inflammation is a consequence of intestinal infections (dysentery, salmonellosis). Less commonly, the reason is long-term treatment with antibiotics, which disrupt the normal balance of intestinal microflora.
Causes may also be related to alcohol abuse and poor diet, which contribute to inflammation. In some cases, chronic colitis is a complication of other gastrointestinal diseases, such as chronic gastritis , hepatitis, pancreatitis, as well as a consequence of abnormalities in the development or functional insufficiency of the intestine.
Prognosis and prevention of acute colitis
Severe symptoms of acute colitis persist for several days. With proper drug therapy and diet, the disease is completely eliminated. If complications arise or there is no adequate treatment, the inflammatory process can take a protracted form.
In some cases, the attack causes peritonitis, sepsis, dehydration shock or subhepatic abscess.
Preventive measures:
- complete treatment of products from contamination;
- drinking only clean water;
- compliance with personal hygiene rules;
- regular examinations by a gastroenterologist;
- complete therapy for diseases of the digestive system;
- exclusion of a sedentary lifestyle;
- compliance with the rules for taking medications;
- proper, balanced nutrition;
- rejection of bad habits.
Forms of chronic colitis
The disease comes in several types:
- Spastic. It manifests itself as severe pain that occurs in various parts of the intestine, so the dislocation of pain sensations changes.
- Nonspecific ulcerative colitis. This disease is characterized by the spread of pain throughout the intestines. Ulcers and bleeding are also possible.
Depending on the cause, chronic colitis can be allergic, infectious, ischemic, radiation, toxic, or combined. In the latter case, several etiological factors are combined.
According to the prevalence of the lesion, colitis is:
- segmental - when only a specific part of the intestine is involved in the pathological process;
- total - the entire colon is affected.
By severity:
- mild degree - when it is easy to achieve remission;
- moderate severity - to ensure long-term relief of symptoms, medications and diet are needed;
- severe degree - exacerbation prevails over remission, and it is difficult to achieve the latter.
Variants of localization of the inflammatory process in chronic colitis.
ICD-10 acute gastroenteritis
According to ICD-10, acute colitis falls into several categories. In most cases, the disease is associated with acute gastroenteritis. This pathology was assigned code K52. Depending on the cause of the attack, the disease may be classified into other groups. For example, if the disease is of an allergic nature, the code K52.2 is assigned, with a toxic form - K52.1, non-infectious colitis - K52.9.
The best folk remedy for gastritis! read here >>. How to get rid of gases in the intestines and why do they occur? Activated carbon cleaning - is it worth starting?
Symptoms
Since in a chronic course the phase of retreat of symptoms and exacerbation alternate, most often patients turn to the doctor precisely when the symptoms acutely make themselves felt. During remission, they are absent altogether or are expressed very weakly.
The main symptoms of chronic colitis are as follows:
- pain that manifests itself in the lateral parts of the abdomen (the nature of the pain can be either acute or aching);
Manifestations of chronic colitis. - rumbling in the intestines;
- belching, often with an unpleasant odor;
- measuring the abdomen in size;
- increased gas formation;
- false urge to defecate, which can occur every few days;
- nausea and weakness;
- unpleasant taste in the mouth;
- increased fatigue;
- sleep disorder;
- pale skin;
- brittle nails and hair loss;
- change in eating habits.
With nonspecific ulcerative colitis, the following symptoms are possible:
- impurities of pus or blood in the stool;
- frequent diarrhea;
- mild tingling pain in the lower abdomen;
- loss of appetite;
- inflammation of the organs of vision (extremely rare);
- pain in the joints;
- muscle weakness.
With an exacerbation of the symptoms of this form, changes in the intestinal mucosa are possible, such as swelling, bleeding, the appearance of small ulcers and formations similar to polyps.
Chronic colitis of a spastic nature manifests itself as follows:
- painful spasms that worsen with hunger or at night;
- bloating;
- flatulence;
- alternating diarrhea and constipation;
- insomnia and, as a result, constant fatigue;
- headache of varying intensity;
- complete bowel movement is often possible only the second or third time, and the process of excreting feces occurs only once a few days;
- rumbling in the stomach.
To reduce the symptoms, a constant diet is needed, but it must be taken into account that certain foods can cause constipation.
Diagnostics
To diagnose chronic colitis, you will need to consult a therapist and gastroenterologist. Its measures are as follows:
Results of irrigoscopy. conversation with the patient, during which he must talk about all the symptoms he has;- examination of the patient: palpation of the abdomen and eye examination. In the presence of inflammation of the latter, diagnosis is also carried out by an ophthalmologist;
- blood test (acute and biochemical);
- immunological analysis;
- stool analysis;
- colonoscopy (helps distinguish exacerbation from remission);
- X-ray using a contrast agent;
- Ultrasound.
Treatment of chronic colitis
Treatment for chronic colitis differs depending on the phase of the disease. At the remission stage, following a diet is sufficient; in case of exacerbation, drug therapy is needed. Treatment should be individualized, taking into account the type of disorder, severity of symptoms and general condition of the patient
Drug treatment
Typically, the following groups of medications are used for chronic colitis:
Antibacterial therapy and abuse of laxatives can lead to exacerbation of chronic colitis. Antibiotics;- probiotics - aimed at restoring the number of beneficial microorganisms in the intestinal microflora;
- antispasmodics - reduce pain;
- laxatives or fastening agents depending on the symptoms (diarrhea or constipation);
- medications containing enzymes;
- corticosteroids, immunosuppressants (for nonspecific ulcerative colitis);
- enveloping medications and sedatives (for spastic colitis).
Non-drug treatments
Among non-drug methods for chronic colitis, sanatorium-resort treatment may be indicated. Mineral waters, baths, microenemas, and intestinal lavage are useful.
Sometimes doctors recommend courses of physiotherapeutic procedures, such as magnetic therapy, acupuncture, and mud applications. Surgical intervention may be required if there are urgent indications in case of complicated colitis.
Some folk recipes can also be used:
- A decoction of sage, St. John's wort, caraway, and mint helps to cope with inflammation.
- For increased gas formation, mint, motherwort, and nettle are useful.
- To eliminate spasms in the intestines, microenemas with a decoction of calendula or chamomile can be performed.
- For ulcerative colitis, a microenema with sea buckthorn oil at night is useful.
Additional treatment methods are carried out in courses. It is recommended to consult a doctor before using them.
Diet for chronic colitis
Therapy will not be effective if the patient does not comply with a special diet. The rules of the diet for chronic colitis are as follows:
- The diet should contain a lot of fiber. It is found in vegetables, cereals, and bread.
- Food should be consumed 4-6 times a day.
- Lean fish and meat are consumed boiled. You can also eat boiled eggs.
- The diet should include many first courses cooked in vegetable broths.
- Seafood is healthy.
- Fruits and vegetables must be peeled.
- Foods that irritate the intestines should be eliminated from the diet. These include dairy and fermented milk products, legumes, spicy and salty foods, nuts, and alcohol.
Nutrition should be high in calories and include a large amount of substances needed by the body: vitamins, proteins, etc.
Diet for colitis is one of the measures included in the complex treatment of the disease
Treatment
OK therapy involves an integrated approach. It is necessary not only to relieve pain and other manifestations of the disease, but also to restore the functional state of the intestines. The basis of treatment is medication and diet. Physiotherapy is considered a good addition to such methods. Acute colitis should be treated under the supervision of a specialist.
If the disease is caused by infectious or bacteriological infections, then their therapy should be carried out separately and fully.
Drug treatment of colitis
Medicines for OK are selected taking into account the individual clinical picture of the patient’s health status. With a mild degree of pathology, you can get by with taking enveloping agents and painkillers. If the illness has caused serious deviations in the functional state of the digestive organ, then the list of necessary medications may include drugs of different categories. You cannot self-medicate OK.
Examples of drugs:
Most often, complex drug therapy is used to treat acute colitis. Thrombolytics (Urokinase, Steptokinase);- antiplatelet agents (Pentoxiillin);
- products from the category of adsorbents (Lactofiltrum);
- immunomodulators (Immunal, Polyoxidonium);
- antihistamines (Claritin, Tavegil);
- sorbents (Polysorb, Smecta);
- antidiarrheals (Enterol, Loperamide);
- intestinal antiseptics (Enterosgel, Furazolidone);
- antispasmodics (no-Spa);
- laxatives (Mukofalk, Guttalax);
- drugs to restore water balance (Regidron);
- vitamin complexes (Alphabet);
- probiotics (Bifindumbacterin, Linex).
Physiotherapeutic treatment of colitis
Physiotherapy in the treatment of acute intestinal colitis is used as an additional method of therapy. Some procedures can significantly accelerate the tendency to recovery and enhance the effect of medications. The doctor prescribes specific physiotherapeutic techniques. To obtain a pronounced result, it is recommended to carry out at least ten sessions.
Examples of physiotherapeutic procedures:
- paraffin applications;
- magnetic therapy;
- ultraviolet irradiation;
- mud applications;
- electrophoresis with drugs;
- current therapy (ultra-high frequency);
Therapeutic diet for colitis
The OK diet implies the complete exclusion of mechanical and chemical irritants that can have a negative effect on the digestive system. Legumes, mushrooms, nuts, and raw vegetables are excluded from the diet. Salted, fried, spicy, fatty, pickled and smoked foods are prohibited.
Alcoholic drinks can cause a deterioration in the patient's health. After using them, a relapse of the pain syndrome will occur.
Nutrition rules for acute colitis:
- During an attack, therapeutic fasting is recommended (you can drink water, rosehip decoction and weak tea);
- the principle of therapeutic fasting cannot be adhered to for more than a day (if the symptoms of the disease do not reduce their intensity during the day, the patient is indicated for hospitalization);
- meals during the diet should be balanced and divided (meals are taken at least five times a day);
- ingredients for dishes are crushed to the maximum extent (preference should be given to homemade pates, vegetable-based purees, jelly, slimy soups, porridges);
- The menu must include fermented milk products (kefir is recommended to be consumed an hour before bedtime to improve digestion processes);
- vegetables for acute colitis can be consumed only after heat treatment;
- When compiling the menu, the principles of Diet No. 4 are used.
After leaving the hospital, patients are advised to create an individual menu to plan their daily diet.
Possible complications and consequences
If the disease is not treated, it can cause a number of complications. This mainly concerns ulcerative colitis. The consequences may be as follows:
- Perforation of the ulcer, which often results in peritonitis. In this case, the symptoms will be manifested by severe bloating and tension in the abdominal muscles, high fever, chills, a coating on the tongue, and general weakness.
- Gangrene of the colon and affected areas of the intestine. In this case, you may feel weakness, high temperature, and decreased blood pressure.
- Blood poisoning or spread of infection to other organs.
- Bleeding in the intestines (with chronic ulcerative colitis).
- The appearance of an oncological tumor is also possible.
Video - Chronic intestinal colitis: causes, symptoms, treatment of colitis.