- What is paraproctitis (rectal fistula)?
- Symptoms of paraproctitis
- Types and stages of the disease
- Diagnosis of rectal fistulas
- Treatment of paraproctitis
- Surgery
- Main risks
- Prevention
- Popular questions
Chronic paraproctitis (rectal fistula)
is a chronic inflammatory process in the anal crypt, intersphincteric space and pararectal tissue with the formation of a fistulous tract. The affected crypt is the internal opening of the fistula.
According to statistics, most patients with rectal fistulas associate the occurrence of the disease with acute paraproctitis. About a third of patients with acute paraproctitis consult a doctor after spontaneous opening of an abscess, after which in most cases a rectal fistula is formed. Approximately half of the patients with acute paraproctitis undergo radical surgery at the time of treatment, the other half only undergo opening and drainage of the abscess without eliminating the entrance gate of the infection, which can subsequently lead to the formation of a rectal fistula. In this case, constant infection occurs from the intestinal lumen, and a fistula tract is formed from scar tissue. The external opening of the fistula is most often localized on the skin of the perineum, its diameter is often no more than 1 mm. If the fistula tract is insufficiently emptied, purulent cavities may form along its length.
The prevalence of chronic paraproctitis reaches 23 cases per 100,000 population, the proportion among rectal diseases reaches 25-30%. Males are more susceptible to this disease than women; the disease more often manifests itself in young and middle age Source: Khomochkin V.V. Operation of ligation of the fistula tract in the intersphincteric layer in the treatment of chronic paraproctitis / V.V. Khomochkin [et al.] // News of surgery. - 2022. - T. 26. - No. 5. - P. 616-623. .
Symptoms of paraproctitis
Symptoms directly depend on where the fistula is located and the state of the patient’s immunity.
Usually, after an illness, a person experiences pain in the anus and a hole appears from which pus comes out. This causes itching, irritation, and bad odor. Sometimes ichor is released along with pus. This occurs when blood vessels are damaged. If the fistula has no outlet, then patients complain only of pain and/or discharge from the rectum or vagina.
An incomplete internal fistula provokes a sensation of the presence of a foreign body in the anal area. If the infiltrate does not leave the fistula cavity enough, the following symptoms appear:
- discomfort and pain in the anal area;
- retention of urination and defecation;
- discharge of mucus, infiltrate, pus from the rectum;
- increased body temperature, chills;
- redness and irritation of the skin around the anus and part of the buttocks.
Chronic paraproctitis during the period of exacerbation gives the following symptoms:
- fast fatiguability;
- sleep disturbance;
- nervous exhaustion;
- headache;
- regular increase in body temperature;
- intimate disorders;
- gas incontinence.
Physiological changes may occur:
- anal deformation;
- disruption of the anal sphincter;
- scars on the muscle tissue of the anal sphincter.
During periods of remission of chronic paraproctitis, the general condition is normal; with proper hygiene, the quality of life is almost not reduced. But with a long course of the pathology and frequent exacerbations, the following may occur:
- sleep disorders;
- powerlessness, weakness;
- headache;
- periodic changes in body temperature;
- nervousness;
- poor work ability;
- deterioration of potency.
Symptoms and manifestations of pathology
Pararectal fistula symptoms are pronounced, the clinical picture is characterized by wave-like symptoms, alternating stages of exacerbation and remission. Depending on the stage, the symptoms of the disease are as follows:
- the presence of a wound (fistula tract) in the perianal area;
- rectal discharge (purulent, serous-purulent, sanguineous), noticeable on underwear;
- unpleasant odor of discharge;
- hyperemia of the skin around the anus, itching, burning;
- dull pain in the rectum, intensifying during bowel movements and receding after defecation due to the outflow of purulent exudate;
- a significant increase in pain during exacerbation (the appearance of an abscess in the perirectal tissue) - in the pelvis, rectum, lower abdomen, especially during bowel movements, walking, coughing;
- disturbances of urination and fecal excretion;
- temperature increase;
- signs of intoxication;
- headache;
- weakness, decreased motor activity.
After opening the fistula, remission occurs, but the wound does not heal, since the inflammatory process does not stop, the formation and outflow of exudate continues, as a result of which the patient’s sleep is disturbed, loss of performance, and disorder of sexual functions and nervous system occur.
With the development of a transphincteric fistula, the following symptoms are observed during a hardware examination of the patient:
- deformation of the anal canal;
- dysfunction of the sphincter;
- scarring of the sphincter muscles;
- disruption of the process of defecation up to fecal incontinence.
Despite the severity of the clinical picture, an incomprehensible shyness keeps some patients from turning to professional doctors. Self-medication is carried out with local drugs, although in case of perirectal fistula, treatment without surgery does not give a lasting effect and can lead to serious complications.
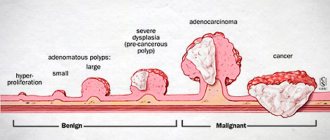
Types and stages of the disease
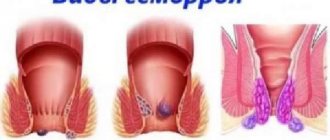
Rectal fistulas can be complete, incomplete, or internal.
- Complete ones
have two openings - located inside and opening into the rectum, as well as external, usually located next to the anus. - An incomplete fistula
has only an internal opening that opens into the rectum. There is an opinion that this is a transitional phase, because sooner or later the external opening will open and the fistula will become complete. - An internal fistula
has two internal openings that extend into the lumen of the rectum.
According to their location relative to the anal sphincter, fistulas are divided into:
- Intrasphincteric
, or marginal. The most common ones usually have a straight course without scars and an external opening near the anus. - Transsphincteric
- the course of such a fistula goes through the anal sphincter at different depths. The higher the course, the more it branches and the more often purulent streaks form, and scar tissue forms around the fistula itself. Scars can deform the anal sphincter and interfere with its function. - Extrasphincteric
- differ in the location of the internal opening - on the surface of the intestinal crypt. The stroke itself passes high and goes around without affecting the outer pulp. The incidence of such fistulas is 15-20% of the total incidence.
Extrasphincteric fistulas are usually tortuous and have a long course. With them, purulent leaks form and scars form around the fistula canals. With repeated exacerbations, new external openings appear. There is a classification that distinguishes four degrees of complexity of fistulas of this type:
- – there are no scars around the internal opening, the course is straight, infiltrates and purulent streaks do not form in the perirectal tissue.
- – scars appear around the internal opening, there are still no ulcers or infiltrates.
- – the entrance to the fistula canal is narrowed, there are no scars, there are ulcers and inflammatory infiltrates in the perirectal tissue.
- – the inlet is enlarged, surrounded by multiple scars, and there are ulcers and infiltrates in the tissue.
Focus on rapid recovery
In order for rehabilitation to be completed as quickly as possible, you will need to adhere to bed rest for the first few days. You will have to spend a little more than a week following the rules of individual antibacterial therapy.
After successful neutralization of the lesion, you will have to work on holding the stool for about five days. A special diet aimed at preventing the formation of toxins will help with this. If increased peristalsis is observed, the doctor will prescribe appropriate medications to relieve symptoms.
The first dressing occurs on the third day. Here you should prepare for the fact that the process itself is quite unpleasant, so doctors prefer to relieve pain with painkillers for the first time.
Tampons previously placed on the wound surface are first soaked in hydrogen peroxide and then removed. The wound itself is also treated with hydrogen peroxide along with antiseptics, and then loosely filled with fresh swabs with ointment. To speed up healing, a strip of ointment is inserted into the rectum itself.
And after a four-day quarantine, the use of specialized candles is allowed. If you cannot have a bowel movement the next day, then you need to use a cleansing enema.
The list of permitted products for the first postoperative period includes:
- semolina porridge cooked in water;
- broths;
- steamed cutlets;
- boiled fish;
- omelette.
But there are no special restrictions on drinking. But all dishes served to the table should not be salty or include seasonings. After a few days, while maintaining positive dynamics, it is allowed to include some more products in the main menu:
- mashed boiled potatoes and beets;
- fermented milk products;
- fruit puree and baked apples.
Still, soda, raw vegetables and fruits, legumes, and alcoholic drinks are still prohibited.
After each trip to the toilet, you will have to take sitz baths to relieve the condition and provide additional disinfection. The proctologist selects the solution for them individually. He will be the one to tell you exactly when the stitches can be removed, but the average period is often about a week. It will take a few more weeks until the healing is complete.
Partial incontinence of feces and gases over the next couple of months is a standard reaction of the body, so this is not a reason to sound the alarm. To improve the clinical picture, it is necessary to train the sphincter muscles using a special set of exercises.
Methods for diagnosing rectal fistulas
In the vast majority of cases, the diagnosis is not difficult to make. The proctologist is based on the patient’s complaints, examination and palpation data. Usually, during a digital examination, the doctor discovers holes in the anal area, from which pus comes out when pressed.
When diagnosing and subsequent treatment of rectal fistulas, the determination of the fistula tract is of fundamental importance. For this purpose, digital and mirror examination of the rectum, probing and examination of the fistulous tract with a dye solution, anoscopy or sigmoidoscopy, fistulography, ultrasound, CT, MRI are used Source: Seidova K.R. Etiopathogenesis and diagnosis of pararectal fistulas. Literature review / K.R. Seidova // Bulletin of surgery of Kazakhstan. - 2011. - No. 4. - P. 23-27. .
One of the main methods for studying pararectal fistulas is probing. With the help of probing, along with the internal opening of the fistula, it is possible to determine the depth of the fistula tract, its connection with the intestinal lumen, the relationship of the fistula to the anal sphincter, and by the movement of the tip of the probe in the canal, bay-shaped expansions and additional branches.
Examination of the rectum using a speculum and proctoscopy allows one to distinguish between altered crypts and the internal opening of the fistula. Injecting a dye into the external opening of the fistula allows you to more clearly distinguish the internal opening. For this purpose, a 1% aqueous solution of methylene blue, iodine, ink, manganese and other solutions are used.
Restoromanoscopy is an endoscopic technique that involves inserting a special tube equipped with optics into the anus. The doctor can assess the condition of the mucosa and do a biopsy to rule out a tumor if one is suspected.
Fistulography is a radiopaque technique. A contrast agent is injected into the anus, and then x-rays are taken. X-ray examination reveals the presence of pockets, cavities, extensive bays, additional branches and curved fistula tracts.
Transrectal ultrasound allows us to trace the fistula tract in the pararectal tissue, the presence of additional cavities along the course, the relationship of the fistula to the anal sphincter, determination of the internal opening of the fistula, differentiation from pararectal neoplasms. Ultrasound examination is also informative in determining anal sphincter insufficiency after surgery in patients with perirectal fistulas.
Women must receive a referral to a gynecologist for examination to rule out a vaginal fistula.
Diagnosis of the disease
Diagnosis, as well as treatment of perirectal fistula, is carried out by a proctologist. When contacting him, many patients are afraid of exacerbation of pain due to diagnostic manipulations, however, in most cases, it is enough for the proctologist to interview the patient to establish the time of onset of symptoms and the nature of the disease.
Next, an external examination is carried out to determine the location and number of openings of the fistula. Only after this does the proctologist begin a digital examination of the rectum, the purpose of which is to establish the location of the fistulous tract, especially if it is not visualized. If noticeable discomfort or pain occurs, local anesthesia is used.
When contacting a proctologist in the stage of exacerbation of a perirectal fistula, instrumental and digital examination may not be prescribed due to the fact that the picture of the disease is presented quite clearly, and any manipulations can cause unbearable pain.
In the acute stage of the disease, an additional examination (instrumental) is prescribed if the doctor has doubts about the accuracy of the diagnosis.
To complement the diagnosis, anoscopy and sigmoidoscopy are performed. To clarify the localization of the fistula tract, in case of very complex fistulas, fistulography is performed. In this study, the fistula tract is contrasted with an X-ray contrast agent and then X-ray or computed tomography is performed.
Treatment methods for paraproctitis
Complete cure is only possible through surgery. Physical therapy, antibiotics, and ointments are used in preparation for or after surgery. Drug therapy can also relieve symptoms and speed recovery. Main recommended pharmacological groups:
- painkillers;
- systemic antibiotics;
- healing ointments.
A course of physiotherapy may include ultraviolet irradiation and electrophoresis.
SM-Clinic specialists diagnose and treat complex pathologies. To make a diagnosis, the doctor collects the patient’s complaints, medical history and objective examination. To clarify the diagnosis and carry out differential diagnosis, additional instrumental studies are performed, such as anoscopy and sigmoidoscopy. These studies are carried out after cleansing the intestines by performing cleansing enemas and taking laxatives.
Features of the rehabilitation period
After recovery from anesthesia, pain appears for a short period. The patient is prescribed painkillers and antispasmodics. To avoid postoperative complications, treatment with antibacterial agents is used. For seven days after the operation, the patient takes broths, cereals, and drinking water. The consumption of fried and salty foods, baked goods, carbonated and alcoholic drinks is excluded.
After a few days, the transition to fractional meals occurs. The patient eats 5 times a day in small portions. You should include foods with a lot of fiber in your diet. Intestinal function will be normalized, constipation and diarrhea will disappear. For a quick recovery, you need to walk in the fresh air for thirty minutes every day. Exercising in the morning is welcome, as it will improve muscle tone.
The recovery period takes 4 weeks. You should avoid physical activity and heavy lifting. It is recommended to visit your doctor to monitor the condition of the wound. Every day, the affected area is washed with warm water and disinfected with antiseptics. It is necessary to establish a daily routine, including proper sleep.
To receive expanded information about the operation and complex studies, fill out an application on the official website of the proctology clinic. An employee of the medical institution will call you back and tell you in detail about the procedures being carried out.
Surgical treatment of pararectal fistulas
The only indication for surgery is the presence of a fistula.
Contraindications:
- general serious condition of the patient;
- liver and kidney failure;
- chronic diseases in the stage of decompensation;
- blood clotting disorder;
- acute infections in the body.
The operation is usually carried out as planned. In case of exacerbation, the abscess is opened, and the fistula itself is removed after 1-2 weeks.
Preparation for surgery includes standard preoperative examination: blood tests, urine tests, ECG, fluorography. Additionally, rectal examinations and/or ultrasound may be prescribed.
There are several types of operations. A specific type is selected depending on the complexity of the pathology:
- ligature technique;
- excision of the fistula along its entire length with or without subsequent suturing;
- plastic surgery of the internal opening of the fistula;
- laser cauterization of the fistula tract;
- filling the fistula tract.
The surgical intervention is performed in a hospital; from 3 to 10 days after it it is necessary to remain under the supervision of doctors. The effectiveness of the operation reaches 90%.
Postoperative period
In the first days in the hospital, a gas tube is installed, antibiotics are prescribed, and dressings are performed. The pain syndrome is relieved with analgesics. It is important that there are no stools in the first 2-3 days, so a liquid diet is prescribed.
From the second or third day you can eat pureed, easily digestible food, you need to drink a lot. It is necessary to prevent constipation, which can cause the seams to come apart. Sitz baths with antiseptic solutions are prescribed, and, if necessary, laxatives and analgesic ointments.
After discharge, the patient should listen sensitively to his body and, if the following symptoms occur, immediately consult a doctor:
- excessive gas formation;
- fecal incontinence;
- a sharp increase in body temperature;
- constant abdominal pain;
- discharge of blood and/or pus from the anus;
- pain when urinating or defecating.
Basic recommendations for the rehabilitation period:
- eat small portions 6 times a day;
- drink at least 2 liters of water per day;
- do not consume foods that irritate the intestines - carbonated drinks, alcohol, chocolate, hot spices, fatty foods, foods with flavoring additives, etc.;
- give preference to vegetables and fruits as sources of fiber, eat cereals, grain bread and dairy products.
Advantages
Radio wave excision of rectal fistula in Moscow is carried out at the Proctologist 81 clinic. The operation is performed by experienced surgeons and coloproctologists. The cost of excision of a rectal fistula depends on the severity of the pathology. Before surgery, the patient is consulted by an anesthesiologist who selects individual anesthesia. General or epidural anesthesia is used.
The following are the advantages of radio wave excision of a tumor:
- minimally invasive, which guarantees the absence of blood;
- fast healing;
- no risk of relapse or complications;
- absence of swelling and inflammatory processes after surgery;
- painlessness;
- speed of the rehabilitation period;
In addition, after the operation the patient goes home and returns to his usual lifestyle. There is no need for observation in a hospital. Minimally invasive interventions relieve the patient of rectal fistula even in advanced stages.
The main risks associated with paraproctitis
Deep fistulas of the extra- and transsphincteric types often recur.
Long-term progressive fistulas, which are complicated by the process of scarring of the walls of the rectum and purulent leaks, can lead to secondary functional changes.
Periods of new exacerbations are dangerous due to the appearance of fresh foci of inflammation and the involvement of an increasingly larger array of the anal sphincter in the inflammatory process. All of the above inevitably affects the general condition of the patient. Often there are complaints of weakened immunity, headaches, sleep problems, decreased performance, and irritability.
In addition to the above complications, a long-existing fistula can lead to pectenosis, namely a cicatricial change in the wall of the anal canal with decreased elasticity and cicatricial stricture. With a long-term illness, in some cases, malignancy of the fistula tract is possible.
Consequences of the operation
In most cases, the operation to excise the fistula takes place without any complications. In rare cases, when a patient consults a coloproctologist with an advanced form of the disease, relapses may occur or secondary functional changes may occur.
You can avoid such problems by contacting a specialist in a timely manner. You don't have to visit a clinic to do this. A preliminary consultation on the treatment of anal fistula is possible on our website. To do this, you need to fill out an application form or call the numbers provided. Here you can make an appointment with a coloproctologist.
Postoperative care
In the postoperative period, all patients must undergo local and general anesthesia. Local anesthesia includes ointments and suppositories, which can locally reduce the severity of pain. Tablets, capsules, intravenous drugs are classified as general anesthesia. If the pain is significant, potent drugs (narcotic analgesics) are also used in a hospital setting. Your doctor will tell you the regimen for using painkillers, methods of administration, and specific names of drugs.
The average hospital stay is 1-5 days. It depends on the extent of the operation, the presence of complications and some other individual characteristics. During the postoperative period, you will undergo daily dressing changes and monitoring of wound healing. Antibacterial therapy is not indicated for all patients, but only if there are indications determined by the doctor. Mandatory wound care includes washing it with a stream of water at room temperature 3-4 times a day. This facilitates mechanical cleaning and will reduce the risk of infectious complications. The doctor will also show you how to properly perform dressings so that you can do them yourself at home.
Why the fistula opened - the main reasons
The formation and opening of fistula canals is always provoked by the active development of the bacterial environment in the operated soft tissues. Staphylococcus aureus becomes the most common causative agent of this pathogenesis after replacement of hip and knee joints; it is found in 60%-70% of cases. In approximately 25%, Staphylococcus epidermidis is cultured. Very rarely, a combination of these two types of staphylococcal infection or other forms of pathogens (Pseudomonas aeruginosa, enterococci, diphtheroids, anaerobes, fungi, etc.) is determined.
The colonization and activation of pathogenic bacteria in the wound area can be influenced by various reasons, we list the most common of them (probability in descending order):
- violation of the rules of asepsis and antisepsis at the time or after removing the suture material from the wound;
- inadequate removal of non-absorbable nylon threads during suture removal (their fragments remaining in the subcutaneous tissue);
- suturing of soft tissues after endoprosthetics initially with insufficiently sterile thread;
- a specific autoimmune response of the body to ligatures applied to a wound or to an installed endoprosthesis, causing a local inflammatory reaction and rejection of threads and implants;
- separation of the edges of the wound at any of the post-surgical stages (this is an open gate for free entry of infection);
- intraoperative infection into the wound due to poorly processed surgical instruments and materials, or severe tissue trauma during the surgical process due to careless work of the surgeon;
- a chronic infectious process in the active phase in any part of the body (genitourinary organs, nasopharynx, teeth, etc.), which is carried through the bloodstream into the area of prosthetics.
It is definitely worth noting those patients who are at risk for the development of purulent fistulas. They have the highest risks, even without the involvement of these provoking factors, not to mention their presence. This group includes people with a history of aggravating concomitant pathology: rheumatoid arthritis, systemic lupus erythematosus, diabetes mellitus, obesity, hemophilia, HIV. Also, older people have a certain predisposition to functioning fistulas due to a weakened immune capacity to resist infections, as well as insufficient activation of tissue repair and regeneration processes.
Anesthesia
For surgical interventions in the perineal area, regional anesthesia is currently used. It includes subarachnoid (spinal) anesthesia at the lumbosacral level, which allows you to block the transmission of sensory and painful nerve impulses to the lower part of the body, including the anorectal area. In this case, the motor function of the lower extremities is not lost. Subarachnoid anesthesia is a fairly safe method and has a low risk of complications from the heart, respiratory system and nervous system. During the operation, for maximum comfort, the patient is conscious or in a state of medicated sleep (sedation). General anesthesia in anorectal surgery is used in individual cases at the discretion of the anesthesiologist-resuscitator.
What to do if the fistula has opened and is leaking?
If a person, after replacing a joint with an artificial endoprosthesis, after some time develops a fistula and, especially, exudate released from the lesion, he should consult a surgeon as soon as possible. The inflammatory process should be carefully examined for the quantity and quality of discharge, the depth of the fistula, infectious genesis, the presence of foreign bodies, the condition of the prosthetic bed, the orientation and stability of the prosthesis. Only on the basis of all these diagnostic data does a specialist develop the optimal treatment tactics, which will prevent the spread of a dangerous infection throughout the body and bring a final recovery.
Before seeing a doctor, the maximum that can be recommended as first aid at home is to treat the affected area with hydrogen peroxide or furatsilin solution. These agents have a local bactericidal and anti-inflammatory effect, which will somewhat reduce the progression of inflammatory and infectious pathogenesis. Carrying out local antibacterial procedures at home is carried out by washing the wound using a disposable syringe without a needle with appropriate antiseptics. Such tactics are a temporary supportive measure; they do not solve the problem, which everyone should be clearly aware of.
After knee/hip replacement, the option of completely relying on yourself (trying to cure an open fistula yourself, waiting for it to close, etc.) is more than absurd and doomed to failure . We emphasize that this type of complication requires strictly medical care and is an absolute indication for hospitalization of the patient in a hospital. There are no other alternatives. The forecasts are directly affected by the timing of the patient’s request for specialized help at the clinic from the moment the first symptoms of the fistula appear.