An irreversible phenomenon during which cells, tissues, and organs cease their vital activity is called necrosis. It can be triggered by pathogenic microbes, mechanical, thermal, chemical, infectious and toxic agents that contribute to tissue destruction. In addition, necrosis can occur as a result of allergies or impaired blood circulation. Taking into account the state of the body and unfavorable local factors, it is possible to determine the pronounced degree of cell necrosis.
The provoking factors for the occurrence of necrosis are pathogenic microorganisms, fungi, and viruses. If blood circulation is impaired and there is hypothermia in this part of the body, vascular spasm will increase and severe disruption of blood circulation will occur. With excessive overheating, metabolism increases, and if blood circulation is impaired, the risk of developing a necrotic process increases.
How does necrosis manifest itself?
If we talk about the first symptoms of necrosis, they are presented in the form of numbness and lack of sensitivity. In such a situation, you must immediately visit an experienced and qualified doctor at a medical center. In addition, the skin becomes pale. This happens because blood circulation is impaired. Over time, the skin will acquire a bluish tint, then turn black or dark green. In the presence of necrosis in the lower extremity, a person notices rapid fatigue while walking, a feeling of coldness, cramps appear, as well as lameness, as a result of which non-healing trophic ulcers will form, which will necrotize over time.
Due to the fact that the respiratory and central nervous systems, kidneys, and liver cease to function normally, blood circulation is disrupted, and a person’s general condition of the entire body deteriorates. In addition, the immune system decreases, as concomitant blood diseases, anemia appear, and metabolic processes are disrupted, the body is depleted, hypovitaminosis and fatigue are observed.
Preparing for treatment
Before surgery, diagnostic tests are usually performed to check your general health and ensure that the surgery can be performed. This may include blood sampling, chest x-ray, electrocardiogram (ECG), angiography, CT or ultrasound, or endoscopy. You should follow a diet that excludes legumes, baked goods, alcohol, fresh fruits and vegetables. A liquid diet is administered at least the day before surgery, with nothing taken on the day of surgery. Depending on the type of bowel resection, it may be necessary to cleanse the bowel. This usually involves taking a laxative 1-2 days before surgery. Cleansing enemas may also be given in the hospital. Immediately before the procedure, antibiotics are prescribed to help prevent infection. You should also tell your doctor about all the medications, supplements, and herbal products you take.
Varieties
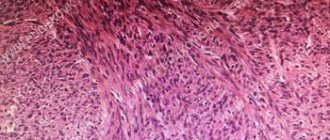
Given the changes that occur in the tissue, there are some forms of necrosis. Namely:
- The cause of coagulation or dry necrosis is the folding, compaction, drying of tissue protein, which then becomes a curdled mass. This is the result of the fact that blood has stopped flowing and moisture has evaporated. Areas of tissue become dry, brittle, and also acquire a dark brown or yellowish gray tint with clear demarcation lines. In the place where the dead tissue was rejected, ulcers will appear, a purulent process will develop, and an abscess will form. The localization of dry necrosis is the spleen, kidneys, and umbilical cord stump in a newborn child.
- With colliculative or wet necrosis, swelling, softening and liquefaction of dead tissue occurs, and a mass with a gray tint is formed and a putrid odor appears.
There are some types of necrosis
1. If the blood supply to a tissue or organ suddenly stops, a heart attack occurs. The term ischemic necrosis refers to the death of any part of a vital organ (brain, heart, intestines, lungs, kidneys, spleen). If the infarction is small, autolytic melting or resorption is observed, followed by tissue restoration. A heart attack can result in impaired tissue functioning, various complications, and even death.
2. If necrosis of a section of bone tissue occurs, the localization of which is the sequestral cavity, this is called sequestration. In such a situation, this area will separate from healthy tissue. The reason for this is a purulent process.
3. Death of the skin, mucous surface, and muscle tissue is called gangrene. The cause of gangrene is tissue necrosis.
4. The presence of bedsores is observed in a person who is completely immobilized. This is explained by prolonged compression of the tissue and damage to the skin. As a result, deep purulent ulcers form.
Possible complications during treatment
The side effects that may occur depend mainly on the type of bowel resection and your overall health. They include:
- obstruction (obstruction) of the intestine,
- paralyzed or inactive bowel
- damage to nearby organs such as the bladder, ureter or spleen, anastomotic leak associated with infectious problems,
- excessive bleeding wound infection,
- hernia,
- thrombophlebitis,
- inability to control urination.
The attending physician should be informed of any of the following problems after surgery: severe pain, swelling, redness, drainage or bleeding in the incision area, muscle pain, dizziness or fever, constipation, nausea or vomiting, rectal bleeding or black, tarry stools.
Stages of the disease
There are several stages of development of this disease. The first stage is characterized by a slight change in bone tissue, when the hip joint maintains functionality, and painful sensations are periodic. At the second stage, cracks begin to form on the surface of the joint, its mobility is impaired, and the person experiences constant pain. The third stage is called secondary arthrosis, when the acetabulum is involved in the process. There is a significant decrease in joint mobility. This stage is manifested by constant and severe pain. At the fourth stage, the bone begins to deteriorate, the muscles atrophy, and the pain is not eliminated by medications.
Staging and classification of sigmoid colon cancer
Based on the type of tumor growth, exophytic and endophytic cancer are distinguished. Exophytic tumors grow into the intestinal lumen and have the appearance of a nodular formation or growth. If they grow excessively, they can obstruct the intestinal lumen, causing intestinal obstruction.
The endophytic, or infiltrative form of cancer is characterized by the fact that it grows in the thickness of the intestinal wall. The tumor can circularly cover the intestinal wall, narrowing its lumen, which also causes intestinal obstruction.
Staging of the disease is carried out based on data on the extent of tumor spread:
- carcinoma in situ - malignant cells are found only in the superficial layer of the intestinal mucosa.
- Stage 1 - the tumor grows into the intestinal mucosa and reaches the submucosa and muscle layer.
- Stage 2 - cancer infiltrates the entire intestinal wall and can extend beyond its limits, but does not yet metastasize.
- Stage 3 - metastases appear in regional lymph nodes. The tumor can be of any size.
- Stage 4 - there are distant metastases, or the tumor spreads throughout the peritoneum (peritoneal carcinomatosis).
What is aseptic necrosis of the femoral head
The head of the femur is considered a problem area where there is an increased risk of arterial blockage and cumulative damage caused by overload and household injuries. The presence of various pathological processes can provoke aseptic necrosis of the thigh.
The main reasons include long-term use of hormonal drugs and antibacterial agents. And also, if a person abuses alcohol, he is often in a stressful state. The provoking factor may be the presence of congenital hip dislocation, osteopenia, osteoporosis, systemic lupus erythematosus, ankylosing spondylitis, rheumatoid arthritis.
The majority of cases have a disappointing orthopedic prognosis and the presence of severe deforming arthrosis. In such a situation, the patient is prescribed endoprosthetics, joint arthrodesis or corrective osteotomy. If magnetic resonance imaging is performed in a timely manner, the disease can be detected at an early stage, which can be treated using conservative methods.
Observation program after treatment method
After your bowel resection you will need to stay in the hospital for several days. The patient should be given warm, liquid food for 1-2 days after surgery. Solid foods and meals will be introduced gradually. If a colostomy or ileostomy has been performed, a specially trained health care professional will teach the patient how to care for themselves. Temporary ostomies usually remain in place for several months. After the rest of the colon has healed, another operation, an anastomosis, will be performed. The hole in the stomach will be closed. A nasogastric tube is inserted through the nose into the stomach during surgery and may be left in place for 24 to 48 hours after surgery. This eliminates stomach secretions and prevents nausea and vomiting. It will remain until bowel activity resumes. Postoperative patient care also includes monitoring of blood pressure, pulse, respiration and temperature. Fluid intake and output are measured, and the color and amount of drainage from the wound is observed at the incision site. The patient can get out of bed approximately 8-24 hours after surgery. Most patients will stay in the hospital for 5-7 days, although laparoscopic surgery can reduce this stay to 2-3 days. Postoperative weight loss accompanies almost all bowel resections. Weight and strength are slowly restored over several months. You will need to follow a diet prescribed by your doctor. Full recovery from surgery may take two months. Laparoscopic surgery can reduce this time to one to two weeks.
What is necrosis of the hip and knee joints
The hip joint includes the acetabulum and the head of the femur. The hip joint is the largest ball-and-socket joint in the human body. It is supplied by a single artery passing through the neck of the femur.
If blood circulation is disrupted, the blood supply to the area will be disrupted, and oxygen and nutrients will not be supplied, and bone tissue will lose its properties. The recovery process will become impossible, osteoarthritis will appear, which is accompanied by severe pain.
After some time, necrosis of the hip joint develops. In such a situation, the patient needs to replace the damaged joint. For this, an artificial analogue is used. The procedure is called endoprosthetics, when motor activity is completely restored.
Destructive processes in the knee joint occur as a result of injury and loss of blood supply. The joints lose their functions, and the person may become disabled. With aseptic necrosis of the knee joint, a person experiences severe pain and observes that the motor ability of the knee has decreased. Magnetic resonance imaging and bone scanning can detect early changes, thereby preventing further bone loss.
Using non-steroidal anti-inflammatory drugs can get rid of pain and reduce inflammation. If a person is indicated for surgery, a bone transplant will be performed.
Original surgical technique
Resection and extirpation are carried out on the basis of an operation - total mesorectal excision - TME. To prevent the appearance of satellite metastases when isolating the rectum in the traditional way, when the lymph nodes located in the mesorectum remain unremoved, I perform the operation through laparoscopic access. This technique allows us to reduce the development of local relapses to a minimum; in our clinic this figure does not exceed 5% (instead of 45%).
Our clinic is equipped with the most modern equipment and instruments, for example, to prevent stricture or failed anastomotic suture after treatment, staplers are used during surgery, mobilization of the intestine is performed bloodlessly thanks to the use of the LigaSure electrothermal tissue ligation device, etc.
Considering that removing part of the intestine onto the abdominal wall can negatively affect the psychological state of the patient, I strive to perform organ-preserving operations, if possible. Therefore, during surgical treatment, my goal is to maintain the continuity of the intestine and anal sphincter, as well as gentle surgery to preserve the nerve structures in the intervention area. If the formation of an anastomosis is impossible, and placing a temporary intestinal stoma on the abdominal wall is the only correct solution, then after a few months the patient can undergo reconstructive surgery, which makes it possible to return to the person’s usual method of bowel movement.
What is necrosis of the talus and humerus?
With this disease, painful sensations appear in the shoulder joint, its movement is limited, as a result of which the risk of atrophy increases. A rare phenomenon includes an altered structure of the humerus. As the disease progresses, the patient is prescribed surgical intervention, which is called endoprosthetics. In this situation, this is the only way to restore lost functions of the upper limbs.
Necrosis of the talus occurs spontaneously and rapidly progresses. With degenerative changes in the ankle joint, deforming arthrosis develops. Thanks to modern diagnostic methods used in the medical center, it is possible to determine the early stage of changes in the ankle joint. In such a situation, mosaic osteochondroplasty is used, as a result of which the anatomy of the joint is restored.
Risk group
Currently, several risk factors have been identified, the presence of which increases the likelihood of developing malignant tumors in the sigmoid colon. These include:
Nutritional Features
The following dietary habits increase the likelihood of developing colorectal cancer:
- Excessive consumption of animal fats and red meat.
- Insufficient content of plant fiber in the diet.
- Regular alcohol consumption.
- Excessive nutrition.
It has been proven that colorectal cancer is diagnosed much less often in vegetarians than in people with a standard diet. For some time it was even considered that meat is the main carcinogen for the intestines and leads to the formation of malignant tumors. The modern theory is based on the fact that plant fibers, which are rich in the diet of vegetarians, cleanse the intestines and do not allow its contents to stagnate. This reduces the contact of the intestinal epithelium with carcinogens and prevents its malignant transformation.
The second risk factor is the presence of polyps . In the vast majority of cases, intestinal cancer develops as a result of malignancy of adenomatous polyps. Moreover, the longer it exists and the larger its size, the more likely its malignant degeneration.
Heredity . The role of hereditary predisposition has been proven in relation to two syndromes: familial adenomatous polyposis (FAP) and Lynch syndrome - hereditary non-polyposis colon cancer. Hereditary cancer accounts for 5-7% of cases of malignant tumors of this localization.
Other risk factors:
- Inflammatory diseases of the large intestine - ulcerative colitis, Crohn's disease.
- History of breast and ovarian cancer.
- Immunodeficiency diseases.
Diagnostic measures
If necrosis is suspected, the patient may be sent for an X-ray examination. However, it should be taken into account that this method does not detect pathology at the initial stage of development. An X-ray can reveal pathology if it has progressed to the second or third stage. During the study of this disease, taking a blood test will also not bring an effective result. Thanks to modern devices that are used for magnetic resonance and computed tomography, it is possible to detect changes in tissue structure in a timely manner and with maximum accuracy.
Introduction
Torsion and necrosis of the omental processes (fat pendants, appendices epiploicae) of the colon (hereinafter referred to as the processes) is a rare disease and occurs in 0.04-0.3% of patients with acute surgical diseases of the abdominal organs. To date, little attention has been paid to the study of diseases of the appendages. As a rule, in the literature there are descriptions of isolated cases of diagnosis and treatment of torsion and necrosis of the processes, and only a few authors provide an analysis of several dozen observations. The diagnosis of torsion and necrosis of the processes can rarely be made at the preoperative stage. In most cases, disease of the appendices is detected during laparoscopy or laparotomy, the indications for which, as a rule, are other diseases of the abdominal cavity and pelvis [8-10, 15, 16].
In the development of torsion and necrosis of processes, the influence of a number of factors is considered significant. It is assumed that the development of torsion and necrosis of the processes is facilitated by disturbances in intestinal motor function, the presence of an inflammatory focus (diverticulitis, cholecystitis, Crohn's disease, etc.), and adhesions in the abdominal cavity. Provoking factors for the development of appendicular disease include sudden movements (flexion, extension), heavy physical activity, sudden loss of body weight, fasting or overeating, closed abdominal injury [3-9, 15, 17]. Torsion and necrosis of the processes occurs in mature and elderly people, with approximately the same frequency in men and women. In most of the described observations, patients with torsion and necrosis of the processes were overweight [3, 5, 6, 11, 12, 14-17].
Torsion and necrosis of processes is extremely rarely diagnosed at the preoperative stage - no more than in 63% of cases [1, 3-4, 7, 9]. This is primarily due to the nonspecificity of the clinical manifestations of the disease of the appendages. As a rule, the disease occurs acutely with constant abdominal pain, which is the main symptom of the disease [3-6, 8, 14-17]. The pain is most often localized in the left or right iliac region, can periodically intensify, and does not radiate (in the absence of involvement of other organs in the inflammatory process). Self-administration of various medications (analgesics, antispasmodics) does not relieve pain, which forces patients to seek medical help. Nausea, vomiting, stool and gas retention, diarrhea are not typical for torsion and necrosis of the processes and occur in no more than 30% of cases [1, 6, 14]. Body temperature may remain normal, but in some cases it rises to low-grade fever. Torsion and necrosis of the processes is characterized by a milder course and a slower increase in symptoms, which causes late presentation of a number of patients (up to 8 days from the onset of the disease). On average, the time of admission of patients to the hospital from the onset of the disease is 1-3 days [2, 6, 8, 14, 15].
Physical examination of patients, as a rule, reveals only local pain on palpation, and in some cases - local tension in the muscles of the anterior abdominal wall. Significant diagnostic difficulties arise when pain is localized in the right iliac region, since these patients often exhibit symptoms of acute appendicitis (Rovzing, Sitkovsky, etc.) [3, 6, 9].
With the long-term existence of torsion and necrosis of the processes, the development of infiltrates may develop, involving neighboring organs of the abdominal cavity and small pelvis, which may be indicated by complaints of dysuric phenomena (with the involvement of the bladder wall), pain in the right hypochondrium (with the involvement of the gallbladder, liver), etc. This often leads to an erroneous diagnosis and incorrect patient management tactics [3-6, 9, 14-16].
Laboratory research methods do not detect any specific changes: blood tests may show moderate leukocytosis (up to 12'109/l), a slight increase in the level of C-reactive protein. Foreign authors emphasize the significant role of ultrasound, computed tomography and magnetic resonance imaging of the abdominal cavity in the diagnosis of torsion and necrosis of the processes [11, 12, 14]. These non-invasive methods make it possible to visualize the altered appendix and make a differential diagnosis with other diseases of the abdominal cavity and pelvis. However, in 50-63.4% of cases, non-invasive radiation methods do not detect changes in the processes, or they are interpreted as another disease [13, 15]. In this regard, at the preoperative stage, as a rule, a diagnosis of other diseases of the abdominal cavity and pelvis is made, the most common being diverticulitis (up to 50% of cases), acute appendicitis (13-76.5%), renal colic (up to 35% ), peritonitis (up to 27.3%), diseases of the uterine appendages (up to 19.6%) [1-3, 6-8]. Most authors consider laparoscopy to be the main method for diagnosing torsion and necrosis of processes, which makes it possible to verify the diagnosis in 83-100% of cases [1, 8-10, 13, 15-16].
At present, the issue of therapeutic tactics for torsion and necrosis of processes has not been completely resolved. Foreign authors are of the opinion about conservative treatment of this disease [11, 12], however, such tactics can lead to the development of complications and relapse of the disease (up to 10% of cases). Most authors are proponents of surgical treatment—removal of the affected appendix, which can be performed using both laparoscopic and laparotomic approaches [1, 6, 8, 12, 16]. Some surgeons [3, 6,] always prefer to perform the operation from a laparotomic approach in case of torsion and necrosis of the processes, in a number of cases combining removal of the process with peritonization of its bed with seromuscular sutures. Recently, more and more works have appeared devoted to laparoscopic interventions for torsion and necrosis of processes [7, 13, 15-16]. In the absence of necrotic changes in the twisted appendage, a number of authors suggest performing endoscopic detorsion using a manipulator, followed by assessment of the viability of the appendix (performed in 4.3-10% of cases). In 14.3-100% of cases, laparoscopic removal of pathologically altered processes is performed with various methods of processing and crossing the pedicle of the process: coagulation, clipping, ligation [2, 4, 5, 7, 8, 15-16].
The rare occurrence, the lack of awareness of doctors about the disease of the appendages, and the need for surgical treatment of the disease determine the relevance of studying the features of the clinical picture, the capabilities of various laboratory and instrumental methods in the diagnosis of diseases of the omental processes of the colon.
The purpose of the study is to study the characteristics of clinical symptoms and evaluate the capabilities of laparoscopy in modern diagnosis and treatment of patients with pathological changes in the omental processes of the colon.
Material and methods
A retrospective analysis of the medical records of 87 patients with a diagnosis of torsion and necrosis of the omental processes of the colon, who underwent laparoscopic intervention in the clinic from January 1995 to December 2012, was carried out. The age of the patients ranged from 20 years to 81 years (average 44±16 years ). There were 44 (50.6%) men, 43 (49.4%) women.
Statistical analysis of the data was carried out using the SPSS 19 program. For qualitative characteristics, data are presented in absolute values and percentages. For quantitative characteristics with a normal distribution of results, the data are presented in the form M
±
SD
, where
M
is the arithmetic mean,
SD
is the standard deviation. For quantitative characteristics with a distribution of results different from normal, the data are presented in the form Me [25; 75], where Me is the median, 25 and 75 are the 25th and 75th percentiles.
Results and discussion
84 (96.6%) patients were admitted to the clinic as an emergency, of which 64 (76.2%) were delivered by an ambulance team, 20 (23.8%) independently went to the clinic’s emergency department. 3 patients were admitted routinely for surgical treatment of other diseases (papillary cystadenoma of the left ovary, chronic salpingoophoritis, polyp of the sigmoid colon). The diagnosis of torsion and necrosis of the processes was suspected at the prehospital stage by the clinic doctor only in 1 observation; by emergency department doctors - in 5 observations. The time from the onset of the disease to admission varied significantly, ranging from 2 hours to 7 days (on average 48 [24; 69] hours).
Diagnosis in the hospital at the preoperative stage was based on patient complaints, anamnesis data, physical examination, data from laboratory and instrumental research methods. Clinical manifestations of torsion and necrosis of the processes were scanty and nonspecific, which led to an erroneous diagnosis at the preoperative stage in most patients. The main clinical manifestations in patients with torsion and necrosis of the processes are shown in Table. 1
.
The leading symptom was constant abdominal pain, observed in 85 (97.7%) patients. The predominant localization of pain was the lower abdomen - in 67 (78.8%) patients, some of them noted local pain in the right or left iliac region (see Table 1)
. 7 (8.0%) patients had the Kocher-Volkovich symptom. Radiation of pain was present in 16 (18.4%) patients, most often to the right thigh. It was not possible to explain the occurrence of irradiation of pain in these patients with intraoperative data; in only 8 of them the necrotic processes were fused with the surrounding organs and tissues - the wall of the colon, neighboring processes, the greater omentum, the parietal peritoneum or the uterine appendages. In 14 (16.1%) patients, pain intensified with movement.
When ascertaining the medical history, 7 (8.0%) patients noted the presence of provoking factors: heavy physical activity (3), sudden movement (1), taking antibacterial drugs (1), food (1), alcohol (1). 26 (29.9%) patients independently took various medications (antispasmodics, analgesics, antibacterial drugs) that did not relieve pain. The ineffectiveness of self-administration of medications and the increasing intensity of pain forced patients to seek medical help.
27 (31.0%) patients complained of dry mouth, 19 (21.8%) of nausea. Vomiting and stool disturbances were observed in isolated patients. 33 (37.9%) patients suffered from fever, most often with a rise in body temperature to subfebrile values. 4 patients had uncharacteristic complaints, which led doctors to suspect another disease and led to an erroneous preoperative diagnosis. Taking into account the data from the intraoperative laparoscopic picture, the occurrence of complaints can be associated with the presence of concomitant diseases, as well as with the development of infiltration around the necrotic appendix. 2 patients complained of dizziness (intraoperatively, in addition to the disease of the appendix, a tense cyst of the corpus luteum was discovered in 1 and a cystadenoma of the left ovary and a uterine pregnancy of 5 weeks in 1). One patient had spotting blood from the genital tract for 11 days (external pelvic endometriosis was diagnosed intraoperatively). One patient complained of frequent urination with pain above the pubis (intraoperatively, a dense infiltrate was discovered around the necrotic process, involving the greater omentum, the wall of the sigmoid colon, adjacent processes and fixed to the parietal peritoneum in the area of the bottom of the bladder).
The condition of 81 (93.1%) patients was assessed as satisfactory, 5 (5.8%) - moderate, 1 (1.1%) - severe. The degree of severity in the last 6 patients was associated with the presence of concomitant diseases - acute gangrenous-perforated appendicitis (1), perforation of the diverticulum of the left half of the colon (1), concomitant therapeutic and neurological diseases (4). It should be noted that 50 (57.5%) patients were overweight, including pre-obesity in 13 (15.0%) patients, class I obesity in 29 (33.3%), class II obesity in 6 (6.9%), grade III obesity - in 3 (2.3%). The average body mass index of patients with torsion and necrosis of the processes was 29.7±5.0 kg/m2.
The main data obtained during physical examination and laboratory and instrumental research methods are presented in table. 2
.
The tongue was wet in 79 (90.8%), light coating on the tongue was observed in 60 (69.0%) patients. Upon examination, the abdomen in all patients was symmetrical; dullness in the sloping areas of the abdomen was not found in any patient. The abdomen was distended in 5 patients. In most patients, peristalsis was of normal sonority; only in 4 cases was it weakened; in 2 of these patients, local fibrinous-purulent peritonitis was detected intraoperatively.
Local tension in the muscles of the anterior abdominal wall was found in 15 (17.2%) patients.
In the majority of observations - 83 (95.4%) - there was pain on palpation of the abdomen, often local - in 52 (59.8%) patients. The areas in which maximum pain was detected on palpation of the abdomen are shown in the figure
.
Figure 1. Pain on palpation of the abdomen.
In 77 (88.5%) cases, pain on palpation was detected in the lower abdomen, of which in 44 (50.6%) maximum pain was detected in the right iliac region, in 29 (33.3%) - in the left iliac region. Symptoms of acute appendicitis (Rovzinga, Sitkovsky, Voskresensky) were found in 31 (35.6%) patients, which led to a diagnosis of acute appendicitis at the preoperative stage in these observations. During laparoscopy, only 3 of them were diagnosed with acute appendicitis: phlegmonous - in 2, gangrenous-perforated - in 1. The Shchetkin-Blumberg symptom from doubtful to positive was found in 29 (33.3%) patients.
A palpable mass in the abdominal cavity was found in 3 patients. Intraoperatively, they revealed a loose infiltrate consisting of a loop of the sigmoid colon, the right fallopian tube, omental processes of the sigmoid colon (1), torsion of two processes of the sigmoid colon among themselves (1), a process of the sigmoid colon fused to the parietal peritoneum (1).
Significant diagnostic difficulties at the preoperative stage were encountered in one patient who complained of pain in the right hypochondrium. Upon examination, in addition to pain in this area, a dubious Ortner’s symptom was detected, and therefore she was treated for acute cholecystitis for 24 hours. Only on the next day the pain was localized in the left iliac region, the patient underwent diagnostic laparoscopy for the purpose of differential diagnosis between diverticulosis and diverticulitis of the left half of the colon and torsion of the process of the sigmoid colon, the latter diagnosis was confirmed. An inactive, dense, painful palpable formation in the abdominal cavity during rectal and two-hand examination was described in one patient. Intraoperatively, a loose infiltrate was discovered around the necrotic process of the sigmoid colon, involving a strand of the greater omentum, soldered to the parietal peritoneum of the small pelvis and the right lateral canal.
During a vaginal examination, a painful displaced formation to the left or right of the uterus was found in 6 (14.0%) patients, which forced differential diagnosis with gynecological diseases at the preoperative stage: torsion of ovarian cystadenoma (4), rupture of an endometrioid ovarian cyst (1), exacerbation chronic salpingoophoritis with the formation of pyosalpinx (1). In all 6 patients, laparoscopy revealed a twisted and necrotic process of the sigmoid colon, while in 2 of them a loose infiltrate had formed around the processes. Only one patient out of 6 was found to have a concomitant disease—ovarian cystadenoma without malnutrition.
Laboratory examination methods for all patients included a general blood test with determination of the level of hemoglobin, erythrocytes and leukocytes, and a general urinalysis. Indicators of hemoglobin (mean value 146 [135; 150] g/l) and erythrocytes (mean value 4.88 [4.38; 5.21] '1012/l) in the general blood test were within normal limits in all patients. The level of leukocytes was increased in 45 (51.7%) patients: 28 (32.2%) had moderate leukocytosis with an increase in the level of leukocytes to (9-12)'109/l, in 17 (19.5%) - more 12'109/l. In 9 patients, during dynamic observation, a repeat blood test was performed to determine the level of leukocytes; its increase was noted in 8 of them. The average leukocyte level was 9.0 [8.2; 11.4]'109/l. In 39 (44.8%) patients, ESR was measured, the average value was 16 [10; 16] mm/h.
For the purpose of further examination and differential diagnosis between various surgical, gynecological and urological diseases, in a number of cases, radiography of the abdominal cavity was performed in search of free gas and fluid levels (12), ultrasound of the abdominal organs (7), ultrasound of the pelvic organs in women (8 ), survey urography (12), ultrasound of the kidneys (6), emergency esophagogastroduodenoscopy (1), excretory urography (1), colonoscopy (1). The data obtained from the listed instrumental research methods were most often nonspecific; they made it possible to exclude other diseases of the abdominal cavity and pelvis, but did not make it possible to diagnose torsion and necrosis of the processes.
Based on abdominal radiography data, moderate pneumatosis of the colon was detected in 4 patients, pneumatosis of the small intestine and a single level of fluid in the small intestine in 2 of 12 patients. According to ultrasound of the abdominal organs, free fluid was found in the abdominal cavity (1), infiltrate (2; not confirmed by intraoperative data).
Of interest is a patient who was admitted routinely for polypectomy for a polyp of the sigmoid colon, but colonoscopy revealed no changes. This forced me to clarify my medical history (pain in the lower abdomen) and schedule a consultation with a gynecologist and an ultrasound of the pelvic organs. According to pelvic ultrasound, a formation up to 32 mm in size was identified, located medial to the left ovary and intimately adjacent to it, with a hypoechoic cellular structure without blood flow during colorectal circulation. Laparoscopy was performed for the purpose of differential diagnosis between ovarian cystadenoma with a history of torsion and torsion of the intestinal process (intraoperative: torsion of the sigmoid process). The remaining 7 patients who underwent ultrasound of the pelvic organs, based on the detected changes and clinical data, were diagnosed with gynecological diseases that were not confirmed by intraoperative data.
Survey urography (12), ultrasound of the kidneys (6), excretory urography (1) were carried out for the purpose of differential diagnosis with renal colic at the preoperative stage; only in one observation this diagnosis could not be excluded. Emergency esophagogastroduodenoscopy (1) was performed on the operating table due to the preoperative diagnosis of perforation of the duodenal bulb ulcer, but no ulcers or erosions were found.
A number of patients were prescribed consultations with specialists. 24 (55.8%) patients were prescribed a consultation with a gynecologist, 14 of them were diagnosed with acute gynecological diseases. 19 (21.8%) patients were consulted by a urologist, only in 1 of them the diagnosis of right-sided renal colic could not be excluded. Patients with concomitant medical and neurological diseases were consulted before laparoscopic surgery by a therapist (11) and a neurologist (1); no contraindications to the operation were identified.
Torsion and necrosis of the processes was suspected in 30 (34.5%) patients based on the results of examination before surgery. In 7 (8.0%) of them it was the main diagnosis in the preoperative epicrisis, in 25 (27.5%) it was suspected during differential diagnosis with other acute surgical and gynecological diseases. In the remaining 57 (65.5%) patients, the indication for surgical intervention was suspicion of other acute surgical and gynecological diseases of the abdominal organs and the need for differential diagnosis between them. The main diagnoses in the preoperative epicrisis for which laparoscopic intervention was performed are presented in Table. 3
.
The most common preoperative diagnoses were acute appendicitis (51.7%), diverticulosis with diverticulitis (13.8%), perforation of a hollow organ (6.9%), ovarian cystadenoma (5.7%), ovarian apoplexy (3.4% ). It is worth noting that the difficulties in diagnosing torsion and necrosis of the processes led to the fact that in the majority of patients - 60 (68.9%) - laparoscopic intervention was performed for the purpose of differential diagnosis between several surgical - 52 (59.7%), surgical and gynecological - 6 (6.9%) and several gynecological - 2 (2.3%) diseases of the abdominal organs. In 58 (66.7%) patients, differential diagnosis was carried out between two diseases. In one patient, differential diagnosis was carried out between three diseases (acute appendicitis, acute mesadenitis and torsion and necrosis of the appendix), in one patient - between four diseases (diverticulosis of the left half of the colon with diverticulitis, colon tumor with perifocal inflammation, torsion and necrosis of the appendix and sigmoiditis). In only 27 (31.1%) patients, laparoscopic intervention was undertaken due to the suspicion of the presence of any one disease.
Laparoscopic interventions in 74 (85.1%) cases were performed within the first 6 hours after admission. On average, the time from admission to laparoscopic intervention was 3 [2; 4] Part 3 patients were operated on more than 24 hours after admission: 2 were admitted for planned treatment and 1 received conservative treatment due to a diagnosis of a painful form of ovarian apoplexy.
Laparoscopic exploration of the abdominal cavity made it possible to establish a diagnosis of torsion and necrosis of the processes in 84 (96.6%) of 87 patients. In the remaining 3 (3.4%) patients, the diagnosis of torsion and necrosis of the processes was established after conversion, which was performed due to the presence of a dense infiltrate of the abdominal cavity (2) and the unsafety of opening a pelvic abscess, the wall of which was the wall of the bladder (1).
Laparoscopic treatment of torsion and necrosis of appendiceal processes was performed in 79 (90.8%) of 87 patients. Removal of twisted and necrotic processes using monopolar coagulation was performed in 61 (77.2%) cases, clipping - in 9 (11.4%), ligation - in 1 case. Necrotic processes that self-amputated during manipulation were removed in 7 out of 79 cases. In one patient, the hydatid of the fallopian tube was excised, which caused torsion of the process, after which the process was considered viable and was not removed.
In the remaining 8 (9.2%) patients, the altered process was removed by ligation and subsequent cutting with scissors during laparotomy. The reasons for conversion in these 8 patients were tight fixation of the appendix to the intestinal wall (3), dense infiltration of the abdominal cavity (2), pelvic abscess (1), combined diseases - diverticulum perforation (1), acute gangrenous-perforated appendicitis with retrocecal retroperitoneal location vermiform appendix (1).
Preoperative diagnosis of diseases of the appendices is also complicated by the possible combination of torsion and necrosis of the appendices with other diseases of the abdominal cavity and pelvis. Comorbid diseases according to laparoscopic intervention were identified in 20 (23.0%) patients (Table 4)
.
Combined laparoscopic intervention was performed in 8 (9.2%) cases, including adhesiolysis (4), removal of fallopian tube hydatid (2), laparoscopic appendectomy (2), electrocoagulation of endometriosis foci (1), opening and coagulation of a tense corpus luteum cyst (1).
There were no intra-abdominal complications. A postoperative complication in the immediate postoperative period was observed in 1 of 79 patients who underwent laparoscopic treatment of torsion and necrosis of the processes. On the 9th day after laparoscopic intervention, an infiltrate was detected in this patient in the projection of the wound in the left iliac region; On the 11th day, an incomplete external colonic fistula was diagnosed. The development of this complication was apparently associated with the presence of a concomitant disease - diverticulosis of the left half of the colon and microperforation of the diverticulum with subsequent formation of an external colonic fistula through the drainage tract, which was confirmed by fistulography and irrigoscopy data. The postoperative period after laparoscopic intervention in the majority of patients with torsion and necrosis of the processes proceeded without complications. The average length of hospital stay after surgery was 5 [5; 8] days.
Death after laparoscopic treatment of torsion and necrosis of appendices occurred in 1 patient out of 79 25 hours after the intervention.
Patient L.
, 76 years old, with pronounced concomitant therapeutic (coronary heart disease - angina pectoris functional class IV, stage III hypertension, paroxysmal atrial fibrillation against the background of atherosclerotic cardiosclerosis) and neurological (cerebral atherosclerosis, 2 acute cerebrovascular accidents with the development of right-sided hemiparesis and dysarthria) diseases was admitted to the clinic in serious condition. As a result of the examination, a suspicion arose of mesenteric thrombosis and peritonitis in the lower abdomen, and therefore a decision was made to perform diagnostic laparoscopy. After preparation in the intensive care unit, 33 hours from the onset of the disease, 4 hours after admission, the patient was operated on, and torsion and necrosis of the process of the sigmoid colon was diagnosed. Laparoscopic removal of the necrotic appendix was performed by coagulating its pedicle (within 10 minutes). Laparoscopic intervention without any special features, with intra-abdominal pressure of 8 mm Hg. The lethal outcome was associated with paroxysm of atrial fibrillation and the development of ischemic stroke in the temporofrontal region of the left hemisphere of the brain, which occurred 25 hours after laparoscopic intervention.
In 8 cases, conversion was performed, while a complication in the immediate postoperative period developed in 1 patient, in whom on the 9th day after removal of the necrotic appendix, appendectomy (for necrosis of the appendix of the sigmoid colon, secondary appendicitis), a hematoma of the postoperative wound was revealed when removing the sutures . Subsequently, conservative treatment was carried out: evacuation of the hematoma, sanitizing dressings, dressings with levomekol, chymotrypsin, analgesic and desensitizing therapy; Slow healing of the wound by secondary intention was noted, which was associated with the presence of type II diabetes mellitus in the patient.
Recurrence of the appendix disease after laparoscopic treatment was noted in 1 (1.3%) of 79 patients. In patient G.
, 25 years old, 28 days after laparoscopic removal of the necrotic process of the sigmoid colon, a relapse of the disease occurred with the appearance of a similar clinical picture, reminiscent of that of acute appendicitis. A diagnostic laparoscopy was performed, which revealed torsion and necrosis of the process of the ascending colon; It was removed laparoscopically using monopolar electrocoagulation with a favorable outcome.
Thus, the clinical picture and data from laboratory and instrumental research methods for torsion and necrosis of the processes are scarce and nonspecific, which significantly complicates the preoperative diagnosis of this disease. The assumption of the presence of torsion and necrosis of the processes before surgery occurs in 34.5% of cases. In unclear diagnostic situations, laparoscopy is the method of choice and allows diagnosing torsion and necrosis of the processes in 96.6% of cases. Successful surgical treatment using laparoscopic access is possible in 90.8% of cases.
How does necrosis end?
A favorable outcome of the pathology will be with enzymatic melting of tissues, germination of connective tissues into the remaining dead tissue, followed by the formation of a scar. The area of necrosis can become overgrown with connective tissue, resulting in the formation of a capsule. In addition, bone can form in the dead area. This phenomenon is called ossification.
An unfavorable outcome of the pathological condition is characterized by purulent melting, as a result of which the risk of bleeding and spread of the lesion increases. This is how sepsis will develop.
With ischemic stroke, myocardial infarction, necrosis of the kidney or pancreas, that is, when vital organs are affected, there is a high probability of death.