All articles
Using suppositories for pain relief and treatment of hemorrhoids
26.09.2017
Suppositories for hemorrhoids are an effective treatment for the disease. The combination of various active ingredients allows you to eliminate the symptoms of the disease.
Today there are many effective ways to treat hemorrhoids. Symptoms can often be relieved with over-the-counter medications and lifestyle changes. One of the most popular remedies are suppositories, or rectal suppositories “for hemorrhoids”. Such candles have different effects and are used for specific purposes. Doctors do not recommend using several remedies to treat hemorrhoids at the same time. Also, you should not use medications containing glucocorticosteroids uncontrollably for longer than 5–7 days. Be sure to tell your doctor if your symptoms worsen while using them, such as increased itching.
Advantages and disadvantages of candles
Rectal suppositories are intended for insertion into the rectum. They contain an active substance and various auxiliary components. The candles soften and melt at the temperature of the human body, ensuring the supply of the active substance, and at room temperature they retain their shape.
Maintaining candles does not require outside help or special medical education, is a non-invasive treatment method, does not cause nausea and vomiting, and in most cases does not cause discomfort. Thanks to these advantages, rectal suppositories have gained popularity and are considered an effective remedy for hemorrhoids.
Like any other dosage form, suppositories also have disadvantages. Firstly, they require storage at low temperatures, often in a refrigerator. Secondly, using candles is not always convenient. Thirdly, some components of suppositories cannot be stored for a long time, so it is not recommended to buy suppositories for hemorrhoids for future use. Remember, candles cannot be used if they are cracked or damaged, or if their color or smell has changed.
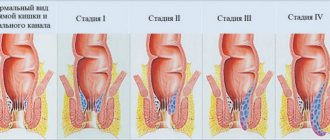
Causes of anal fissure
Anal fissure: schematic illustration
Before moving on to how to treat a crack and which suppositories are best to use, it is necessary to dwell in more detail on the main reasons for their appearance. Because depending on what caused it, treatment will be prescribed. The main reasons include:
- Childbirth, namely the strong tension that appears at the moment of pushing. This tension, as well as a large load, can lead to rupture
- Incorrect management of the postpartum period, namely incorrectly induced first stool. Or rather, it would be more appropriate to say here, not the use of laxatives that soften stool
- Injuries resulting from the passage of hard feces. Most often, this is also supplemented by an infection that penetrates through them.
- Straining with constipation, which stretches the skin
- Lifting weights, as this increases pressure on the rectum
- Mechanical injuries that can result from improper administration of an enema by a nurse, during anal sex, etc.
- Vascular problems that can lead to anal fissures
- Problems with epithelial cells, namely disruption of the maturation process of superficial skin cells
- Neuromuscular lesions of the sphincter, which disrupts cell nutrition processes, which creates a favorable environment for the proliferation of bacteria and microbes
When treating an anal fissure, it is necessary to get rid of not only the consequence itself, but also treat the cause, because otherwise there will be no positive and lasting effect after the procedures, and after some time the disease will return again.
Effects of rectal suppositories
Anesthesia
Reduce pain due to analgesic components (novocaine, lidocaine, etc.). Anesthetic suppositories for hemorrhoids are prescribed for acute pain.
Reduce blood clot formation
Achieved through anticoagulants, which block blood clotting mechanisms. After taking such suppositories, blood stops clotting normally, so patients with a tendency to bleed are advised to first consult a doctor.
Anti-inflammatory effect
You can relieve inflammation with the help of non-steroidal anti-inflammatory drugs (aspirin, diclofenac), as well as hormonal drugs (drugs containing glucocorticosteroids). Natural substances (sea buckthorn oil, propolis) are also widely used.
Stop bleeding
In this case, drugs that are opposite in action to anticoagulants are used. That is, they activate the blood clotting process, stop bleeding, but can lead to the formation of blood clots if used uncontrolled.
Strengthening veins
Achieved by increasing their tone, strengthening the wall, and increasing elasticity.
In order to increase the effectiveness of suppositories for hemorrhoids and ensure ease of use, they sometimes include several active ingredients. For example, suppositories with analgesic, anti-inflammatory and hemostatic effects are popular.
The most effective suppositories for hemorrhoids according to buyers
This section includes suppositories that received the largest number of positive reviews from patients with the initial stages of the disease.
- Methyluracil is an effective drug with a pronounced immunostimulating and anti-inflammatory effect. The use of this drug allows achieving remission in 95% of patients. It accelerates the healing of damage to the mucous membrane and stimulates epithelial renewal. Another advantage of the drug is its price - less than 100 rubles.
- Nigepan. These suppositories have analgesic, anti-inflammatory and thrombolytic effects. Its cost ranges from 400 to 500 rubles.
- Proctosan is a medicinal product with a natural composition. These suppositories relieve inflammation, pain, itching, and also reduce bleeding from hemorrhoids and promote their rapid healing.
Features of application
When using suppositories, it is necessary to take into account their features and follow some rules:
- Carefully study the instructions for use and pay attention to storage conditions.
- Do not hold the candle in your hands for a long time, as it may begin to melt.
- If suppositories are used once a day, it is best to use them at night. If twice, then in the morning and in the evening.
- It is necessary to insert the suppository with clean hands while lying on your side, after bowel movements and performing hygiene procedures.
You can find out which suppositories for hemorrhoids are best for the patient, as well as how to take them correctly and for how long, after consultation with a specialist.
A comprehensive plan is drawn up individually for each patient, taking into account his age, gender, presence and absence of concomitant pathology and individual characteristics of the body.
Share:
Symptoms of a chronic fissure
We need to talk separately about chronic anal fissure, since the symptoms may vary slightly. These include:
- Painful sensations that occur during the act of defecation, straining, and last about 4 minutes after it. The pain cannot be called severe; the term “tolerable” is more appropriate.
- Sphincter spasm, which is not as pronounced as in the case of the acute stage
- Bleeding from the anus. You can notice it by traces of blood on toilet paper or on the surface of stool
- The appearance of a “bump”, which indicates the presence of a constant inflammatory process
- Cyclicity of symptoms. This happens because the crack can heal, and then, under the influence of hard feces, begin to bleed again. Also, a crack can make itself felt after heavy physical exertion.
If a person has at least one of the above symptoms, then it is necessary to consult a specialist as soon as possible, because a chronic disease is much more difficult to treat than the acute stage.
Prevention
Preventive measures include:
- A healthy balanced diet without abuse of alcohol, various herbs/spices, spicy and fried foods.
- Maintain hygiene of the anal area and genitals.
- Sexual intercourse only with barrier contraception.
- Avoiding anal injury/hypothermia.
- Adequate physical activity, especially when sitting for a long time.
- If signs of inflammatory diseases of the pelvic organs appear, it is imperative to consult a doctor.
Tests and diagnostics
The diagnosis of “proctitis” is established based on the patient’s complaints, medical history, the results of a visual examination of the anus, a digital examination of the rectum, as well as data from stool tests (bacterial stool examination, coprogram, stool analysis for worm eggs) and instrumental research methods (sigmoidoscopy ). If necessary, PCR/ELISA diagnostics are performed for a specific infection ( syphilis , gonorrhea ). Proctitis is differentiated from paraproctitis , hemorrhoids , rectal fissure , polyposis .
Diet
Diet for proctitis, along with hygienic procedures and drug therapy, is the most important component of treatment, which is based on therapeutic Tables No. 3 , 4 ( 4a , 4b ) and is specifically determined by the type of functional disorders present - diarrhea/constipation. The basis of therapeutic nutrition for acute proctitis/complications of chronic proctitis is maximum mechanical/chemical sparing of the rectal mucosa. This requirement is achieved by eliminating all irritating foods from the diet.
First of all, the consumption of food containing plant fiber, which irritates the intestinal mucosa and increases gas formation, is limited: all spicy/spicy/fried foods, pickles, smoked legumes, salads and canned vegetables are completely removed from the daily diet. Freshly prepared juices, fruits/berries, sweets, chocolate, bran, seeds, dried fruits, and nuts are excluded. Drinking alcoholic and carbonated drinks is strictly prohibited.
The basis of nutrition is soups in non-concentrated chicken/vegetable broth, well-cooked porridge in water, soft-boiled chicken eggs, semi-liquid dishes, boiled fish/steamed meat, steamed cutlets, cottage cheese, low-fat yogurt, kefir, jelly, rosehip decoction. Bread - in the form of crackers or stale white. Fruit: baked apples. The amount of fluid consumed should be 1.5-2.0 l/day.
During the remission stage, the diet is expanded by including kefir and sour cream, vegetables/fruits (carrots, potatoes, cabbage, plums, strawberries, apples) consumed in moderation. In case of diarrhea, it is necessary to include in the diet foods that help slow down intestinal motility: mashed potatoes, mucous, pureed dishes (non-concentrated soups, minced meat dishes, pureed porridges, pureed rice, jelly, jelly), as well as products with an astringent effect - strong tea, quince decoctions, pomegranate peel, dogwood, bird cherry, pear, lingonberry, blueberry.
In cases of constipation, the diet includes foods that help activate the motor function of the intestine, as well as promote the act of defecation: foods that contain coarse plant fiber: wholemeal bread (bran, grain), cereals, sauerkraut, vegetables/berries/fruits, dried fruits (figs, prunes), muesli, as well as vegetable oils. It is recommended to increase the amount of fluid consumed to 2-2.5 l/day through mineral water, green/herbal tea, apricot, plum, carrot, pumpkin and peach juices. Taking bifido-drugs is indicated.
Pathogenesis
Despite the fact that the pathogenesis of proctitis in most cases is based on an inflammatory process, the etiological features of its development determine its specificity, which is not possible to consider within a short article. Therefore, we will consider only the pathogenesis of radiation proctitis , which is based on the activation of the cytokine system in the mucous-submucosal layer of the intestine, which is caused by the massive destruction of tissue cells during the irradiation process. As a result, a cascade of reactions is launched that promotes the development of inflammatory changes in the walls of blood vessels.
Ischemia of the mucous-submucosal lining of the rectum occurs and increases to a critical state with gradually progressive atrophy and fibrosis of the submucosal layer (often with necrotic changes), the end result of which is bleeding from telangiectasias (newly formed vascular plexuses), the formation of recto-vesical / recto-vaginal fistulas and rectal strictures .
Classification
The classification of proctitis is based on various signs.
According to the duration of the disease/morphological features, inflammation of the rectum is divided into acute and chronic.
Acute proctitis, which in turn, according to characteristic changes in the rectal mucosa, is divided into:
- catarrhal-hemorrhagic (edematous mucosa/presence of hemorrhages);
- catarrhal-purulent (presence of purulent plaque on the mucous membrane);
- polyposis (growth of polyps on the rectal mucosa);
- erosive (there are surface defects on the mucosa).
- ulcerative (ulcers of different sizes form on the mucous membrane);
- ulcerative-necrotic (ulcers and local areas of mucosal necrosis are present on the mucosa).
Chronic proctitis, which is divided according to the condition of the mucous membrane into:
- normotrophic (mucosa without noticeable changes);
- atrophic (folds of the mucous membrane are thinned/smoothed);
- hypertrophic (folds of the mucous membrane are loose and thickened).
According to the etiology, there are nutritional, stagnant (with constipation of various origins), radiation (with radiation therapy), infectious, parasitic, chlamydial, gonorrheal and other proctitis.
During pregnancy
Distal colitis (proctosigmoiditis/proctitis) during pregnancy proceeds similarly to that in non-pregnant women. It is important that childbirth with proctitis occurs with minimal severity of symptoms (that is, symptoms in acute proctitis should be stopped as much as possible, and in cases of chronic proctitis, childbirth should take place in the stage of remission of the disease).
Treatment of the disease during pregnancy is carried out similarly; the use of mesalazine during pregnancy is not limited, and the dose of mesalazine is not reduced. As evidenced by numerous reviews (forum for pregnant women), childbirth with inflammatory bowel diseases, including isolated proctitis, in most cases occurs without complications.
List of sources
- Vorobyov G.I., Zaitsev V.G. Incidence of the population with diseases of the colon, anal canal and perineum // Current issues of coloproctology. - Ufa, 2007. - P. 550-554.
- An V.K., Rivkin V.L., Solomka A.Ya. Dangers, complications and errors in proctology. - M., 2011. -112 p.
- Tkachev A.V., Mkrtchan L.S., Nikitina K.E., Volynskaya E.I. Inflammatory bowel diseases: at the crossroads of problems // Practical. medicine. 2012. T. 58. No. 3. P. 17–22.
- Valuyskikh E.Yu., Svetlova I.O., Kurilovich S.A., Osipenko M.F., Maksimov V.N., Voevoda M.I. Clinical and genetic aspects of inflammatory bowel diseases. Russian Journal of Gastroenterology, Hepatology and Coloproctology. - 2008. - T. 18. - No. 6. - P. 68-74.
- Radiation (radiation) damage to the intestine / Burkovskaya V.A. // Gastroenterology of St. Petersburg - 2013 - No. 3-4.